Enhancing Nurse-Patient Communication: Managing Heart Failure and Hypertrophic Cardiomyopathy
The Role of Nursing Education in Improving Patient Outcomes
Effective communication between nurses and patients is crucial in managing heart failure and hypertrophic cardiomyopathy (HCM). Nurse-patient communication plays a significant role in promoting patient understanding, treatment plan adherence, and overall care satisfaction.
Additionally, nursing education is vital in preparing nurses to provide high-quality care and support to individuals with these conditions. This article will explore the importance of enhancing nurse-patient communication in improving patient outcomes for individuals with heart failure and HCM.
Hypertrophic Cardiomyopathy Basics
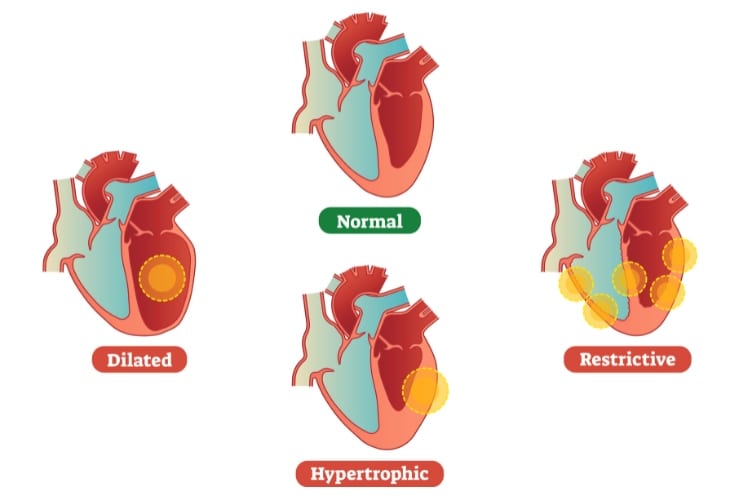
Cardiomyopathy relates to changes in the heart muscle that may affect how well the heart functions. This disorder may affect the heart’s electrical system or structural components, causing dilated cardiomyopathy or restricted or hypertrophic cardiomyopathies.[i]
Hypertrophic cardiomyopathy’s (HCM) incidence rate is between 1:200 and 1:500 patients in the US, which means an estimated 750,000 patients have been diagnosed with HCM.[ii] The estimates are believed to be lower than the actual number of patients not yet diagnosed. HCM is often genetic and affects patients of all ages and races; other HCM patients may be found within the same family.[iii]
Cardiac imaging is required to assess the left ventricular wall thickness and observe potential left ventricular obstruction for accurate diagnoses of HCM. A transthoracic echo and cardiac MRI usually are part of the cardiac imaging.[iv] To assess whether a patient may have an obstructive gradient, a transthoracic stress echo may also be needed.[v]
There are multiple presentations or expressions of HCM: obstructive, non-obstructive, and apical. Patients with HCM require the care of cardiologists, cardiac radiologists, and, often, electrophysiologists.[vi]
Due to the thickened ventricles affected by HCM, the ventricles can become stiff, and the patient may eventually develop diastolic dysfunction or heart failure with preserved ejection fraction (HFpEF).
Heart Failure Overview
The prevalence of heart failure is estimated to affect 64 million people worldwide, or 1-20 per 1,000 people.[vii],[viii] Heart failure has been an emerging epidemic for over 20 years, although the current data report the incidence has declined in more industrialized countries.[ix] An increase in diagnosis has occurred in patients with obesity, the elderly, and in less-industrialized countries.[x]
Heart failure is often characterized by a low left ventricular ejection fraction (LVEF), although the right ventricle can also be affected. A normal heart’s ejection fraction is between 55-70%.
Current 2022 AHA/ACC/HFSA guidelines identify the following types of LVEF-based heart failure:
- LVEF ≥ 50%
- HFpEF: Heart failure with preserved EF
- LVEF 41-49%
- HFmrEF: Heart failure with mildly reduced EF
- Previous LVEF ≤ 40 % and follow-up measurements LVEF > 40%[xi]
- HFimpEF: Heart failure with improved ejection fraction
- HFimpEF is considered to be a subset of HFrEF, as the LVEF improved ≥ 41 %, but it is important to continue on their guideline-directed medical therapy (GDMT)[xii]
- HFimpEF: Heart failure with improved ejection fraction
- LVEF ≤ 40%
- HFrEF: Heart Failure with reduced EF
The Importance of Nursing-Patient Communication for Successful Patient Management
Adequate nurse-to-patient communication involves having the right foundational skills built with knowledge and training, respect, empathy, and mutual understanding.[xiii]
If HCM is suspected, providers need to pay close attention to the patient’s symptoms, family history, and diagnostic testing that has been conducted. HCM patients may have a normal life expectancy, while others may have complications such as atrial and ventricular arrhythmias, including atrial fibrillation, non-sustained ventricular tachycardia, and ventricular tachycardia.[xiv]
Heart failure patients may also be prone to atrial and ventricular arrhythmias.[xv] Screening and monitoring are recommended in the form of Holter monitors and—in some patients—implantable recording devices.[xvi]
Patients with both conditions often live with symptoms of shortness of breath, chest pain, fatigue, dizziness, edema, and decreased exercise tolerance.[xvii] They require specific medications to control and help improve their heart function and symptoms. HCM patients often require beta-blockers or calcium channel blockers to improve the contraction and allow for appropriate filling of their hearts.[xviii]
Fluid volume is managed cautiously in patients diagnosed with HCM and HFpEF, mild diuresis with spironolactone, SGLT-2, or low-dose diuretics.[xix]
It is essential to recognize that patients may feel burdened or overwhelmed with their medication regime, limitations due to symptoms, and exhibit symptoms of depression.
Healthcare provided respectfully based on the patients’ and their family’s needs can promote positive outcomes by continually providing patient-centered care (PCC).
Nursing Care and Guidance
Nursing care should be individualized, as each patient may have specific needs, questions, or gaps in knowledge that require assessment by their providers. Patients with heart failure may have frequent hospital admissions, which may be due to gaps in their knowledge due to lack of communication, miscommunication, and/or low health literacy.[xx]
Frequent guidance and review with the patients and their support system on ways they can be successful with self-care and reiterating the warning signs of worsening symptoms may prevent symptom exacerbations and hospital readmissions.[xxi]
Referral to social work may provide additional support and assistance for patients who lack necessities. Psychological support may further assist the patient in other aspects of their life that may contribute to their health.
Some patients with HCM and heart failure find patient support groups helpful. In addition to more than just the emotional support offered, support groups also provide patient education and guidance.
To rebuild physical and emotional strength, cardiac rehab may be recommended. Cardiac rehab is supervised by a health care professional, providing an exercise program designed for the individual patient, emotional support, and education on lifestyle modifications. Cardiac rehab can help the patient avoid an exacerbation.[xxii]
Healthcare provided respectfully based on the patients’ and their family’s needs can promote positive outcomes by continually providing patient-centered care (PCC).[xxiii] PCC can be defined as health care directed at meeting a patient’s goals and understanding their circumstances using a holistic view to guide the patient on improving their health and addressing their needs.[xxiv]
Potential benefits of improved communication and patient-centered care
- Improved health outcomes with a further understanding of the condition and treatment plan
- Greater sense of trust in the care team and medical treatments
- Patients may take greater ownership of their care outside of the medical system[xxv]
- Reduction in the length of hospital stays and readmissions[xxvi]
- Improved resource access and use.
- Better morale and productivity among clinicians[xxvii]
Elements of Patient-centered Care
- Identifying the patient’s understanding of their disease, facilitators, and barriers to their medications and treatment plans[xxviii]
- Provide a caring and supportive environment by showing presence and respect for individual and cultural beliefs
- Multi-disciplinary care teams are essential when providing holistic and coordinated care
- Shared decision-making involves the patient, their family, and the care team
Strategies for Enhancing Patient-Centered Care
- Active listening and empathetic communication
- To improve patient understanding, ask about the preferred learning style and gear educational tools with plain language in their preferred language
- Promote open communication and shared decision-making[xxix]
PCNA Resources
The Preventive Cardiovascular Nurse Association (PCNA) has various resources to help healthcare providers and patients increase their knowledge about HCM and heart failure.
Healthcare Provider Resources
- HCM in Clinical Practice (CE program)
- HCM: Novel Treatments (education program)
- HCM: Patient Access and Team-Based Care (education program)
- HCM: Patient Adherence (education program)
- HCM: Ask the Experts (education program)
Patient Resources
- Hypertrophic Cardiomyopathy: What You Need to Know
- Patient education sheet
- Patient video
- Hypertrophic Cardiomyopathy: Is Your Heart Holding You Back? (Poster)
- Hypertrophic Cardiomyopathy Infographic: What Every Patient Should Know (Video)
Clinical Takeaways
- Enhancing nurse-patient communication is essential in managing heart failure and hypertrophic cardiomyopathy.
- Nursing education equips nurses with the necessary knowledge and skills to communicate effectively with patients and improve outcomes.
- By incorporating patient-centered education in professional development, nurses can enhance their communication abilities and provide high-quality care to individuals with heart failure and HCM.
- Patients will experience better understanding, increased adherence to treatment plans, higher satisfaction levels, and improved overall outcomes.
[i] Nicholson, Christopher, et al. “Structural Heart Disease.” Cardiac Care, 2022, pp. 399–411, https://doi.org/10.1002/9781119117810.ch25.
[ii] Maron, Barry J., et al. “Diagnosis and Evaluation of Hypertrophic Cardiomyopathy.” Journal of the American College of Cardiology, vol. 79, no. 4, Jan. 2022, pp. 372–389, https://doi.org/10.1016/j.jacc.2021.12.002.
[iii] Casella, Michela, et al. “Characteristics of Patients with Arrhythmogenic Left Ventricular Cardiomyopathy.” Circulation: Arrhythmia and Electrophysiology, vol. 13, no. 12, Dec. 2020, https://doi.org/10.1161/circep.120.009005.
[iv] Maron, Barry J., et al. “Diagnosis and Evaluation of Hypertrophic Cardiomyopathy.” Journal of the American College of Cardiology, vol. 79, no. 4, Jan. 2022, pp. 372–389, https://doi.org/10.1016/j.jacc.2021.12.002.
[v] Maron, Barry J., et al. “Diagnosis and Evaluation of Hypertrophic Cardiomyopathy.” Journal of the American College of Cardiology, vol. 79, no. 4, Jan. 2022, pp. 372–389, https://doi.org/10.1016/j.jacc.2021.12.002.
[vi] Casella, Michela, et al. “Characteristics of Patients with Arrhythmogenic Left Ventricular Cardiomyopathy.” Circulation: Arrhythmia and Electrophysiology, vol. 13, no. 12, Dec. 2020, https://doi.org/10.1161/circep.120.009005
[vii] Savarese, Gianluigi, et al. “Global burden of heart failure: a comprehensive and updated review of epidemiology.” Cardiovascular Research vol. 118, no. 17, 2023, pp. 3272-3287, https://doi.org/10.1093/cvr/cvac013.
[viii] Groenewegen, Amy, et al. “Epidemiology of heart failure.” European Journal of Heart Failure vol. 22, no. 8, 2020, pp. 1342-1356, https://doi.org/10.1002/ejhf.1858.
[ix] Heidenreich, Paul A., et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation, vol. 145, no. 18, 2022, https://doi.org/10.1161/cir.0000000000001063.
[x] Heidenreich, Paul A., et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation, vol. 145, no. 18, 2022, https://doi.org/10.1161/cir.0000000000001063.
[xi] Heidenreich, Paul A., et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation, vol. 145, no. 18, 2022, https://doi.org/10.1161/cir.0000000000001063.
[xii] Heidenreich, Paul A., et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation, vol. 145, no. 18, 2022, https://doi.org/10.1161/cir.0000000000001063.
[xiii] Tuohy, Dympna, and Evan Wallace. “Maximizing nurse-patient communication in the
emergency department.” Emergency nurse: the journal of the RCN Accident and Emergency Nursing Association, 1 Aug. 2023, https://doi:10.7748/en.2023.e2179.
[xiv] Ommen, Steve, J., et al. “2020 AHA/ ACC Guideline for the Diagnosis and Treatment of Patients with Hypertrophic Cardiomyopathy”. Circulation, vol 142, no. 25, pp.558-631. doi.org/10.1161/CIR.000000000000937
[xv] Ommen, Steve, J., et al. “2020 AHA/ ACC Guideline for the Diagnosis and Treatment of Patients with Hypertrophic Cardiomyopathy”. Circulation, vol 142, no. 25, pp.558-631. doi.org/10.1161/CIR.000000000000937
[xvi] Heidenreich, Paul A., et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation, vol. 145, no. 18, 2022, https://doi.org/10.1161/cir.0000000000001063
[xvii] Heidenreich, Paul A., et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation, vol. 145, no. 18, 2022, https://doi.org/10.1161/cir.0000000000001063.
[xviii] Heidenreich, Paul A., et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation, vol. 145, no. 18, 2022, https://doi.org/10.1161/cir.0000000000001063.
[xix] Heidenreich, Paul A., et al. “2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation, vol. 145, no. 18, 2022, https://doi.org/10.1161/cir.0000000000001063
[xx] Ivynian, Serra E., et al. “Patient preferences for heart failure education and perceptions of patient-provider communication.” Scandinavian Journal of Caring Sciences, vol. 34, no. 4, 2020, pp. 1094-1101, https://doi:10.1111/scs.12820.
[xxi] Tuohy, Dympna, and Evan Wallace. “Maximizing nurse-patient communication in the emergency department.” Emergency nurse: the journal of the RCN Accident and Emergency Nursing Association, 1 Aug. 2023, https://doi:10.7748/en.2023.e2179.
[xxii] American Heart Association. Cardiac Rehab for Heart Failure. American Heart Association. Jul, 2023. Retrieved from https://www.heart.org/en/health-topics/heart-failure/treatment-options-for-heart-failure/cardiac-rehab-for-heart-failure. Retrieval date Aug 25, 2023
[xxiii] “What is Patient-Centered Care?” NEJM Catalyst, vol. 3, no. 1, jan. 2017. https://doi.org/doi:10.1056/CAT.17.0559
[xxiv] Araki, M. “Patient Centered Care and Professional Nursing Practice.” Journal of Biomedical Research and Clinical Investigation, vol 1, no. 1.1004. Oct. 2019. doi.org/10.31546/JBRCI.1004
[xxv] Ivynian, Serra E., et al. “Patient preferences for heart failure education and perceptions of patient-provider communication.” Scandinavian Journal of Caring Sciences, vol. 34, no. 4, 2020, pp. 1094-1101, https://doi:10.1111/scs.12820.
[xxvi] Busch, Isolde M et al. “Humanization of Care: Key Elements Identified by Patients, Caregivers, and Healthcare Providers. A Systematic Review.” The Patient, vol. 12, no. 5, 2019, pp. 461-474, doi:10.1007/s40271-019-00370-1.
[xxvii] Kwame, Abukari, and Pammla M. Petrucka. “A Literature-Based Study of Patient-Centered Care and Communication in Nurse-Patient Interactions: Barriers, Facilitators, and the Way Forward.” BMC Nursing, vol. 20, no. 1, 2021, https://doi.org/10.1186/s12912-021-00684-2.
[xxviii] Ivynian, Serra E., et al. “Patient preferences for heart failure education and perceptions of patient-provider communication.” Scandinavian Journal of Caring Sciences, vol. 34, no. 4, 2020, pp. 1094-1101, https://doi:10.1111/scs.12820.
[xxix] Kwame, Abukari, and Pammla M. Petrucka. “A Literature-Based Study of Patient-Centered Care and Communication in Nurse-Patient Interactions: Barriers, Facilitators, and the Way Forward.” BMC Nursing, vol. 20, no. 1, 2021, https://doi.org/10.1186/s12912-021-00684-2.
