PAD Walking Program Patient Handout
PAD Activity Program Patient Tool
Research in vascular exercise has demonstrated remarkable improvement in symptoms of leg pain (claudication) without expensive or invasive interventions. Regular walking programs are extremely helpful for patients with PAD and intermittent claudication.
This instruction sheet is designed to help get patients started with an activity program.
Get Your Patients Walking
Video Transcript
Hello! I am Jane Nelson Worel, Nurse Practitioner and Director of Clinical Education at the Preventive Cardiovascular Nurses Association.
Our topic today is What You Can Do to Help Patients with PAD Feel Better Today. Because treatment options are limited, working with patients with peripheral artery disease, PAD, can be frustrating.
Symptoms such as leg pain or weakness when walking, known as claudication, limits the distance and duration the patient can walk without rest. This can make climbing stairs or activities of daily living difficult—and the pain may even persist when the individual is resting or lying down.
How can you help these patients feel better today?
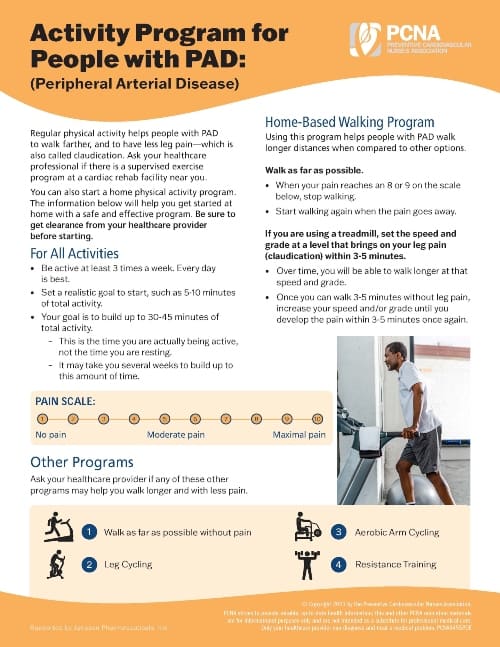
Regular walking programs are extremely helpful for patients with PAD and intermittent claudication.
Studies have demonstrated that participants in a walking program may be able to walk up to three or four times farther and have less leg pain within twelve weeks. This benefit can be a significant motivator for patients.
Walking may seem counter-intuitive to your patients, so it is important to provide guidance as to how to start, build and maintain their walking program.
A set of written instructions, such as those found on the PCNA web site at pcna.net/PAD, may help patients and their families/caregivers remember what you have discussed during the clinical visit. This is also a great way for patients to track progress.
As you are discussing the walking program with your patient and perhaps their family/caregiver, it is important to assess their readiness to make changes and their perceived ability to change. You can assist by listening for potential barriers and helping the patient identify possible solutions.
Based on your patient, identify a starting place for their walking program. The goal is 30-45 minutes of total walking time (not counting rest breaks) and it may take several weeks to build to this level.
It is important to review the pain scale with your patient so that they can identify when to continue and when to stop walking.
On a treadmill, the patient should set the speed and grade at a level that brings on claudication pain within 3 to 5 minutes. The patient should then walk at this rate until they experience claudication of moderate severity, rest until the pain improves, and then continue walking.
Over time, the patient should be able to walk longer at the designated speed and grade. At this point, the speed and grade should be increased until the patient experiences the pain within 3 to 5 minutes once again.
An example of your initial instructions to a patient might be, “Please begin your walking program with 5 to 7 minutes of walking 3 times per week. Remember to rest when your leg pain is an 8 to 9 on the pain scale.”
If your patient does not have access to a treadmill, a park or shopping mall that provides a level walking surface and comfortable spots to rest – such as a bench – will do. Apartment dwellers can also use the hallways of their buildings.
It is important to note that patients with PAD are at high risk for coronary artery disease. Make certain to provide your patients with instructions as to how to identify symptoms including chest pain or shortness of breath and identify the steps they should take if they experience angina or heart attack-like symptoms.
Managing risk factors associated with cardiovascular disease is important for those with PAD. Lowering cholesterol, quitting smoking and improving blood sugar and blood pressure control may improve claudication symptoms while reducing the risk of heart attack and stroke.
In conclusion, you can help your patients with PAD feel better starting today. Thank you for taking the time to join us, and please visit pcna.net/PAD for additional information and resources.
Funded through a grant from Janssen Pharmaceuticals, Inc.
Disclaimer: Please be aware that these forms include a sample of current clinical guidelines. However, clinical guidelines (federal, state, local, or those issued by clinical organizations) change over time, so the reader should remember to investigate any recent legal or clinical developments.
