HDL Cholesterol: Too Much of a Good Thing?
Can High Good Cholesterol be a Bad Thing?
It is considered a well-established fact that high-density lipoprotein cholesterol (HDL-C) is a robust, inverse predictor of the risk of experiencing an atherosclerotic cardiovascular (ASCVD) event.[i] Whereas, low HDL-C characterizes an atherogenic dyslipidemia that reflects adverse lifestyle choices, impaired metabolism, and increased cardiovascular risk.[ii]
Substantial new evidence exists in the area of dyslipidemia treatment to indicate that extremely high HDL-C[iii] levels are not necessarily always protective against CVD and may in certain instances, be harmful. The exact cause is unknown, although the European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) dyslipidemia guidelines were recently updated to highlight the potential for an increased risk of ASCVD when HDL-C levels exceed 90 mg/dL (2.3 mmol/L).[iv] This update provides additional evidence to the 2018 American College of Cardiology (ACC) and American Heart Association (AHA) multi-society guidelines for the management of blood cholesterol.[v] While the American guidelines have not endorsed 90 mg/dl as a cut-off, high HDL-C levels >80 mg/dl have been found to be associated with an increased risk of all-cause death.[vi]
Types of Cholesterol
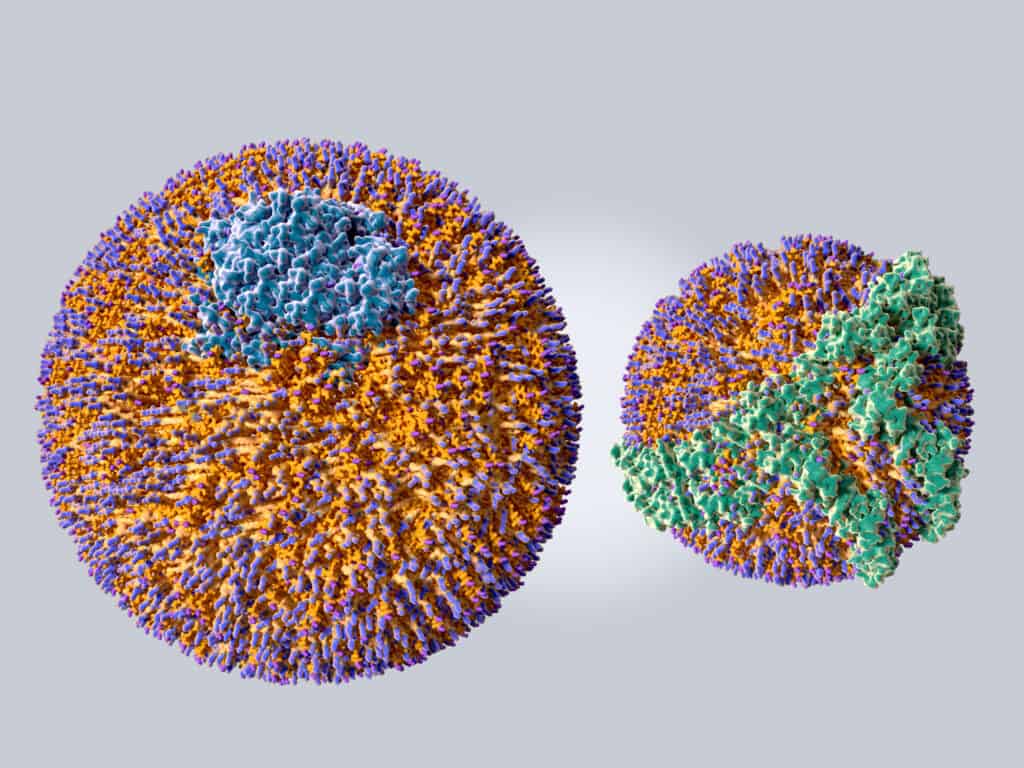
Cholesterol is a lipoprotein composed of various quantities of fat and protein;[vii] HDL-C is denser than low-density lipoprotein (LDL-C) because it has more protein and less fat.[viii] HDL-C has anti-inflammatory properties, protects the intimal lining of arteries from the effects of LDL-C, has positive antioxidant effects, and has a protective effect on cells and chemical messengers in the blood and tissues.8 HDL-C promotes cholesterol efflux from the cells in the body to the liver for degradation and removal, thereby reducing plasma cholesterol levels.[ix]
According to new evidence, the association between very high HDL-C levels and CVD risk, very high HDL-C levels and all-cause mortality[x]–[xi] is represented by a U-shaped curve.12 CVD risk is associated with very low levels of HDL-C below 40mg/dL in men and below 50-58 mg/dL in women, and a modest, increased ASCVD risk exists with HDL-C levels above 90 mg/dL in Asians, above 97 mg/dL in White males and above 135 mg/dL in White females.11, [xii]
Mach et al.,2 recently demonstrated an inverse association between plasma HDL-C and ASCVD risk. This inverse association is among the most consistent and reproducible of associations in observational epidemiology. Randomized controlled trials have failed to provide compelling evidence that HDL-C is causally associated with ASCVD risk.[xiii] Furthermore, no evidence from randomized trials[xiv] exists to indicate that therapeutically increasing plasma HDL-C will reduce the ASCVD risk.[xv] Therefore, it is unknown if therapies exist to alter the function of HDL-C particles to reduce ASCVD risk.[ii]
Currently, the principal goal of lipid therapy is to decrease LDL-C levels rather than increase HDL-C levels. Extensive evidence has demonstrated LDL-C and apoprotein B–containing lipoproteins are causally associated with CVD and therefore, primary targets in dyslipidemia treatment.[xvi]According to the new guidelines, LDL-C levels should be lowered as much as possible, specifically to <55 mg/dL in very high-risk individuals, those with established CVD or familial hypercholesterolemia, ASCVD, or other risk factors.[ii]
The recently updated, Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health,[xvii] suggests non-HDL-C is the metric of interest. It is desirable to have a low non-HDL-C, specifically, less than 130 milligrams per deciliter (mg/dL). Non-HDL-C refers to different atherogenic lipoprotein fractions of which LDL-C is the most concerning. A non-HDL-C assessment can be reliably measured in a non-fasting state. LDL-C contributes to plaque accumulation in the intimal lining of arteries[xviii] thereby increasing the risk for atherosclerosis. Plaque narrows vessel size, diminishes blood flow, and increases vascular pressure contributing to hypertension CVD, stroke, and kidney disease.[xix]
HDL Cholesterol and Cardiovascular Disease Risk
While common causes of HDL-C include foods high in unsaturated fats (fish, nuts, and green leafy vegetables), exercise, and alcohol (all factors associated with a decreased CVD risk), it is important to note that recent study outcomes related to HDL cholesterol and the risk of CVD are somewhat controversial[xx]. Sun et al.,[xx] observed that extremely low HDL-C (<20 mg/dL) levels contributed to high CVD mortality. Extremely low HDL-C levels were more frequently found in males, older individuals, inpatients, and those with multiple adverser factors. Whereas an analysis of data on individuals with CVD in the UK Biobank (14,478 participants) and the Emory CVD Biobank (5,467 participants) demonstrated that very high HDL-C levels were paradoxically associated with higher mortality risk.[xxi] Of those individuals with HDL-C levels greater than 80 mg/dl, 6.86% experienced an all-cause death compared with 11.26% of individuals with normal HDL-C concentrations of 40-60 mg/dl (p=0.01). Similarly, the results of a cohort study by Liu et al. (2022) suggest that in individuals with coronary artery disease compared with those with normal HDL-C levels (40-60 mg/dL), those with very high HDL-C levels (>80mg/dL) had a higher risk of all-cause and cardiovascular death, independent of traditional cardiovascular risk factors and alcohol use.[xxi]
This controversy regarding HDL-C and CVD may be due to the balance between beneficial and harmful subspecies of HDL-C.[xxii] Subspecies of HDL-C have surface proteins that affect functions of thrombosis, inflammation, immunity, and lipid metabolism, and while some are protective, others are detrimental to cardiovascular health. Detrimental subspecies contribute to thrombosis, inflammation, immunity, or lipid metabolism. For example, HDL-C containing Complement C3 or alpha-2-Macroglobulin (α2M) are associated with a higher risk.18 In contrast, HDL-C containing apoC1 or apoE are associated with a lower CVD risk. Jensen et al.[xxiii] observed HDL-C containing apoC3 to be predictive of a higher relative risk of a first coronary heart disease event.
Treatment Targets and Lifestyle Interventions for Managing Lipid Levels
The current guidelines recommend using total cardiovascular risk assessment tools such as the Framingham Risk Score and ACC/AHA Pooled Cohort Equations when considering the primary prevention of CVD risk calculator. Since these tools do not consider current evidence, ASCVD prognosis should include LDL-C lowering as the primary target for reducing risk in addition to HDL-C levels.[ii]
| Lipid Treatment Targets | ||
|---|---|---|
| LDL-C | Very-high risk in primary or secondary prevention | Achieves >50% LDL-C reduction from baseline. LDL-C <55 mg/dL. |
| No current statin use: likely to require high-intensity LDL-lowering therapy. | ||
| Current LDL-lowering treatment requires increased treatment intensity | ||
| High risk | Achieves >50% LDL-C reduction from baseline and LDL-C <70 mg/dL. | |
| Moderate risk: | A goal of <100 mg/dL. | |
| Low risk: | A goal of <116 mg/dL. | |
| Non-HDL-C | Non-HDL-C secondary goals are <2.2, 2.6, and <85, 100, and 130 mg/dL for very-high-, high-, and moderate-risk people, respectively. | |
| Apolipoprotein (Apo)B | ApoB secondary goals are <65, 80, and 100 mg/dL for very-high-, high-and moderate-risk people, respectively. | |
| Triglycerides | No goal, but <150 mg/dL indicates lower risk. Higher levels require need to assess other risk factors. | |
Implications for Nurses: Educating patients regarding high HDL Cholesterol
Nurses should counsel patients regarding lifestyle modification to maintain cholesterol levels for vascular protective effects. This includes a healthy and balanced diet, weight loss, regular exercise, avoiding/quitting smoking, and limiting alcohol consumption.[xxiv] Weight loss, smoking cessation, a healthy diet and exercise all promote raising HDL-C.[xxv]
Lifestyle Interventions for Cardiovascular Disease Prevention
Smoking
Smoking contributes to arterial plaque and smoking cessation reduces CV risk, specifically by increasing HDL-C levels.[xxvi]
Physical Activity
Varying modes and intensities of physical activity increase HDL levels and decrease non-HDL levels.[xxvii] Moderately vigorous physical activity is recommended for 30 to 60 min most days of the week. Exercise and vigorous physical activity was positively correlated with HDL (r = .30, p < .05) and negatively (r = -.26, p < .05) with LDL cholesterol levels in overweight/obese and lean individuals.[xxvii] A moderately positive association was observed between omega-3 levels and vigorous-intensity PA indicating the benefit of physical activity intensity to enhance the utility of omega-3-containing foods.[xxvii]
Resistance training significantly increased HDL levels and decreased LDL, total cholesterol, and triglyceride levels.[28] Similarly, a 9-month lifestyle coaching program involving 104 participants who ate more favorable food for CVD risk and were more active demonstrated a decrease in total cholesterol, LDL-C, non-HDL-C, and triglyceride levels in addition to an increase in HDL-C.[xxiv]
The benefits of physical activity separate from diet were demonstrated[xxx] in older adults with metabolic syndrome. Those who consumed an energy-restricted Mediterranean diet and engaged in physical activity improved HDL cholesterol and triglyceride metabolism compared to a nonrestrictive Mediterranean diet without physical activity.
Diet
From a dietary standpoint, the best way to lower your cholesterol is to reduce your intake of saturated fat and trans fat. The American Heart Association recommends:
- limiting saturated fat to less than 6% of daily calories and minimizing trans fat in the diet
- limiting red meat and dairy products made with whole milk, fried food
- emphasizing low-fat dairy products
- cooking with healthy oils
- emphasizing fruits, vegetables, whole grains, poultry, fish, nuts, and nontropical vegetable oils
- limiting red and processed meats, sodium and sugar-sweetened foods and beverages
The DASH (Dietary Approaches to Stop Hypertension) and the Mediterranean diet fit this description.[xxxi]
Dietary factors influence CVD development through traditional risk factors, such as plasma lipids, blood pressure, and plasma glucose[ii] and the benefits of physical activity separate from diet were demonstrated[xxx] in older adults with metabolic syndrome; those who consumed an energy-restricted and engaged in physical activity improved HDL-C and triglyceride metabolism compared to a nonrestrictive Mediterranean diet without physical activity. Alcohol has also been found to increase HDL-C levels.[xxi]
Body weight
Modest reductions of 5-10% of body weight favorably impact cardiovascular risk factors and improve lipid profiles.[xxxii] For every kilogram decrease in body weight, especially abdominal fat, HDL-C increased by 0.4 mg/dL.[iv]
How Often Should Patients Be Screened?
Cholesterol should begin in childhood with testing should be done every 5 years for people age 20 or older who are at low risk for cardiovascular disease and more often for those with CVD risk factors, although according to the 2018 ACC/AHA Guidelines, cholesterol management is based an individual’s lifetime cardiovascular risk.[v]
Future Considerations for HDL Cholesterol
The key to a healthy plasma lipid profile and CVD prevention is a lifestyle involving regular physical activity and exercise, a healthy diet, limited alcohol consumption, and managing blood cholesterol levels. Future studies focusing on new insight and analysis of HDL-C subclasses and the effects of HDL subspecies proteins and their function while lowering LDL-C will assist to develop and standardization HDL-C and provide insight into HDL-C targets for all individuals.
[i] Barter P, Genest J. HDL cholesterol and ASCVD risk stratification: A debate. Atherosclerosis. 2019;283:7-12. doi:10.1016/j.atherosclerosis.2019.01.001
[ii] Rohatgi A, Westerterp M, von Eckardstein A, Remaley A, Rye KA. HDL in the 21st Century: A Multifunctional Roadmap for Future HDL Research. Circulation. 2021;143(23):2293-2309. doi:10.1161/CIRCULATIONAHA.120.044221
[iii] Güle., S.E.C. High-density lipoprotein cholesterol and risk of cardiovascular disease. J. Cardiol. Pract. 2020, 19, 133–134.
[iv] Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2019, 41, 111–188.
[v] S.M. Grundy, et al., AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines, Circulation 139 (25) (2018) e1082–e1143, 2019.
[vi] Liu C, Dhindsa D, Almuwaqqat Z, Sun YV, Quyyumi AA. Very High High-Density Lipoprotein Cholesterol Levels and Cardiovascular Mortality. Am J Cardiol. 2022;167:43-53. doi:10.1016/j.amjcard.2021.11.041
[vii] CDC (2021). Cholesterol Myths and Facts. Accessed August 8, 2022
[viii] British Heart Foundation, “Risk Factors for High Cholesterol” (2022). Retrieved from https://www.bhf.org.uk/informationsupport/risk-factors/high-cholesterol.
[ix] Hunjadi M, Lamina C, Kahler P, et al. HDL cholesterol efflux capacity is inversely associated with subclinical cardiovascular risk markers in young adults: The cardiovascular risk in Young Finns study. Sci Rep. 2020;10(1):19223. Published 2020 Nov 5. doi
[x] Franczyk B, Rysz J, Ławiński J, Rysz-Górzyńska M, Gluba-Brzózka A. Is a High HDL-Cholesterol Level Always Beneficial?. Biomedicines. 2021;9(9):1083. Published 2021 Aug 25. doi:10.3390/biomedicines9091083
[xi] Madsen CM, Varbo A, Nordestgaard BG. Extreme high high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J. 2017;38(32):2478-2486. doi:10.1093/eurheartj/ehx163
[xii] Huang YQ, Liu XC, Lo K, et al. The U Shaped Relationship Between High-Density Lipoprotein Cholesterol and All-Cause or Cause-Specific Mortality in Adult Population. Clin Interv Aging. 2020;15:1883-1896. Published 2020 Oct 2. doi:10.2147/CIA.S271528
[xiii] ASCVD Risk Predictor Plus is available at: http://tools.acc.org/ASCVD-Risk-Estimator-Plus/#!/calculate/estimate/)
[xiv]Holmes MV, Asselbergs FW, Palmer TM, Drenos F, Lanktree MB, Nelson CP, Dale CE, Padmanabhan S, Finan C, Swerdlow DI, Tragante V, van Iperen EP, Sivapalaratnam S, Shah S, Elbers CC, Shah T, Engmann J, Giambartolomei C, White J, Zabaneh D, Sofat R, McLachlan S, consortium U, Doevendans PA, Balmforth AJ, Hall AS, North KE, Almoguera B, Hoogeveen RC, Cushman M, Fornage M, Patel SR, Redline S, Siscovick DS, Tsai MY, Karczewski KJ, Hofker MH, Verschuren WM, Bots ML, van der Schouw YT, Melander O, Dominiczak AF, Morris R, Ben-Shlomo Y, Price J, Kumari M, Baumert J, Peters A, Thorand B, Koenig W, Gaunt TR, Humphries SE, Clarke R, Watkins H, Farrall M, Wilson JG, Rich SS, de Bakker PI, Lange LA, Davey Smith G, Reiner AP, Talmud PJ, Kivimaki M, Lawlor DA, Dudbridge F, Samani NJ, Keating BJ, Hingorani AD, Casas JP. Mendelian randomization of blood lipids for coronary heart disease. Eur Heart J 2015;36:539 550.
[xv] Lincoff AM, Nicholls SJ, Riesmeyer JS, Barter PJ, Brewer HB, Fox KAA, Gibson CM, Granger C, Menon V, Montalescot G, Rader D, Tall AR, McErlean E, Wolski K, Ruotolo G, Vangerow B, Weerakkody G, Goodman SG, Conde D, McGuire DK, Nicolau JC, Leiva-Pons JL, Pesant Y, Li W, Kandath D, Kouz S, Tahirkheli N, Mason D, Nissen SE; ACCELERATE Investigators. Evacetrapib and cardiovascular outcomes in high-risk vascular disease. N Engl J Med 2017;376:1933 1942.
[xvi] Atar D, Jukema JW, Molemans B, et al. New cardiovascular prevention guidelines: How to optimally manage dyslipidaemia and cardiovascular risk in 2021 in patients needing secondary prevention?. Atherosclerosis. 2021;319:51-61. doi:10.1016/j.atherosclerosis.2020.12.013
[xvii]Lloyd-Jones DM, Allen NB, Anderson CAM, et al. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: A Presidential Advisory From the American Heart Association. Circulation. 2022;146(5):e18-e43. doi:10.1161/CIR.0000000000001078
[xviii] NIH (2022). What is Atherosclerosis?. Accessed AUG 8, 2022
[xix] American Heart Association. Understanding & Managing Cholesterol. Date: march 24, 2022. Accessed 8 AUG, 2022.
[xx] Sun L, Duan L, Jia D. Clinical characteristics of cardiovascular patients with extremely low levels of high-density lipoprotein cholesterol. Lipids Health Dis. 2021;20(1):149. Published 2021 Oct 30. doi:10.1186/s12944-021-01583-w
[xxi] Liu C, Dhindsa D, Almuwaqqat Z, et al. Association Between High-Density Lipoprotein Cholesterol Levels and Adverse Cardiovascular Outcomes in High-risk Populations. JAMA Cardiol. 2022;7(7):672-680. doi:10.1001/jamacardio.2022.0912
[xxii] Sacks FM, Liang L, Furtado JD, et al. Protein-Defined Subspecies of HDLs (High-Density Lipoproteins) and Differential Risk of Coronary Heart Disease in 4 Prospective Studies. Arterioscler Thromb Vasc Biol. 2020;40(11):2714-2727. doi:10.1161/ATVBAHA.120.314609
[xxiii] Jensen MK, Aroner SA, Mukamal KJ, Furtado JD, Post WS, Tsai MY, Tj.nneland A, Polak JF, Rimm EB, Overvad K, et al. High-density lipoprotein subspecies defined by presence of apolipoprotein C-III and incident coronary heart disease in four cohorts. Circulation. 2018;137:1364–1373. doi:10.1161/CIRCULATIONAHA.117.031276
[xxiv] Ruiz-Ramie JJ, Barber JL, Sarzynski MA. Effects of exercise on HDL functionality. Curr Opin Lipidol. 2019;30(1):16-23. doi:10.1097/MOL.0000000000000568
[xxv] https://www.heart.org/en/health-topics/cholesterol/prevention-and-treatment-of-high-cholesterol-hyperlipidemia
[xxvi] Maeda K, Noguchi Y, Fukui T. The effects of cessation from cigarette smoking on the lipid and lipoprotein profiles: a meta-analysis. Prev Med 2003;37:283 290.
[xxvii] Aljaloud KS, Hughes AR, Galloway SDR. Impact of Physical Activity on Adiposity and Risk Markers for Cardiovascular and Metabolic Disease. Am J Mens Health. 2022;16(2):15579883221092289. doi:10.1177/15579883221092289
[xxviii] Zaman GS, Abohashrh M, Ahmad I, et al. The Impact of Body Resistance Training Exercise on Biomedical Profile at High Altitude: A Randomized Controlled Trial. Biomed Res Int. 2021;2021:6684167. Published 2021 Jun 1. doi:10.1155/2021/6684167
[xxix] Castela Forte J, Gannamani R, Folkertsma P, et al. Changes in Blood Lipid Levels After a Digitally Enabled Cardiometabolic Preventive Health Program: Pre-Post Study in an Adult Dutch General Population Cohort. JMIR Cardio. 2022;6(1):e34946. Published 2022 Mar 23. doi:10.2196/34946
[xxx] Sanllorente A, Soria-Florido MT, Castañer O, et al. A lifestyle intervention with an energy-restricted Mediterranean diet and physical activity enhances HDL function: a substudy of the PREDIMED-Plus randomized controlled trial. Am J Clin Nutr. 2021;114(5):1666-1674. doi:10.1093/ajcn/nqab246
[xxxi] American Heart Association. “Prevention and Treatment of High Cholesterol” (2022). Retrieved from https://www.heart.org/en/health-topics/cholesterol/prevention-and-treatment-of-high-cholesterol-hyperlipidemia.
[xxxii] Zomer E, Gurusamy K, Leach R, Trimmer C, Lobstein T, Morris S, James WP, Finer N. Interventions that cause weight loss and the impact on cardiovascular risk factors: a systematic review and meta-analysis. Obes Rev 2016;17:1001 1011.
