The dynamics of AFib and Heart Failure often lead to patients navigating both diseases simultaneously. Learn how to apply effective strategies for management, including team-based care, shared decision-making, addressing adherance barriers, and more, in this conversation with Kathy Wood, PhD, RN, FAHA, FAAN, and Eryn Bryant, MSN, APRN-CNP, FPCNA.
Episode Resources
[00:00:00] I’m Erin Ferranti, board president for PCNA, and I’d like to welcome you to this episode of the Heart to Heart Nurses Podcast. PCNA is the proud home of cardiovascular nurses and one of the leading figures in the fight against cardiovascular disease. We have the resources you need for your day-to-day practice or to follow your passion to new areas of learning and growth.
Geralyn Warfield (host): (00:19)
I’d like to welcome our audience today to an episode where we are going to be discussing the interrelationships of two different diseases, but we’re going to get to that in a moment. First, I’d like to introduce you to our guests. Kathy, could you start introducing yourself to our audience?
Kathy Wood (guest): (00:32)
Sure, my name is Kathy Wood, and I teach at the Emory University School of Nursing.
Geralyn Warfield (host): (00:39)
Excellent. Eryn, how about you?
Eryn Bryant (guest): (00:41)
My name is Eryn Bryant. I am a heart failure nurse practitioner at Ohio State, And I run our transition of care program. I also co-founded our heart function wellness program, which is kind of rooted in lifestyle medicine for our heart failure population.
Geralyn Warfield (host): (00:58)
Well, thank you both for being with us today.
And the two diseases that we are going to discuss today are heart failure and atrial fibrillation. And there’s definitely a lot of interconnectedness there, a lot of overlaps. Let’s talk a little bit about how those two disease states really are complementary, if that’s a good word to use (it’s probably a horrible word to use), but how they interact with one another. And I’m not sure who would like to start.
Eryn Bryant (guest): (01:23)
I’m happy to start. I mean, I think both—I know we kind of talked that when we were asked to speak about heart failure and AFib, it’s just they’re just such big topics. But the reality is their huge prevalence in the population. Most of us are going to be hard pressed to get through our career and not see many heart failure patients and many AFib patients and many that have both.
The prevalence of patients who have heart failure and AFib, it’s quite a large footprint, and is continuing to grow. And they’re both complex disease states to manage. And sometimes it goes back to chicken or egg, in that one can contribute to the other and vice versa.
And so it is important to have a well understanding of the both of these states, management of both diseases, and then, kind of the complexities that go into these patient discussions.
Because while they’re common, and we kind of live in these worlds, it can be very burdensome to the patient to be trying to navigate these two things simultaneously.
Kathy Wood (guest): (02:27)
I think that’s right, Eryn. I think with AFib, patients lose about 25 to 33 % of their ejection fraction. So, it can lead to heart failure that way. As well as if they have heart failure first, the extra fluid and stretch of the left ventricle puts stretch on the atrium. And so, the wiring that is normally there is kind of short-circuited. So, they can add to one another and exacerbate situations.
About 41% of patients with AFib go on to heart failure, and about 41% also of patients with both AF and heart failure developed the AF first. So, it’s interesting how there’s such a symbiotic relationship between the two.
But normally if you have AF, you’ll have it forever and you’ll eventually develop heart failure. If you have heart failure, you’ll eventually develop AF. So, it’s kind of a double-edged sword of both situations.
Geralyn Warfield (host): (03:39)
I can imagine as a patient that is dealing with one or the other or both of these diseases that it can be overwhelming. So, what can we do as healthcare professionals to help these patients with that complexity?
Kathy Wood (guest): (03:52)
Yeah, I think with patients that develop heart failure first, we talked about early, as soon as you obtain an AF diagnosis, referral to the EP department so that that communication and relationship has been set up so patients can then call on the EP contact if they develop AFib later on.
If the patient has AFib first, it’s really great to bring in the heart failure group as the AFib worsens and they develop, go from paroxysmal to persistent, and that’s usually when you see the heart failure kick in.
As well as rate control is really important with AFib. The faster their heart rate, the more likely they are to develop a tachycardiomyopathy. And so, by controlling that rate and the rhythm and maintaining sinus as often as you can, you can prevent that heart failure.
Eryn Bryant (guest): (04:50)
Absolutely. And I’ll add kind of two concepts that I think are important to have integrated into practice, which are an interdisciplinary care team. Just navigating and interfacing with the health care system, especially when you have one or more chronic diseases, is so complex, so burdensome to patients and their families.
So, to have an Interdisciplinary team, all of which lending their expertise, lending navigation services, especially from our nursing colleagues is really, really helpful to these patients.
And then a lot of education is done with these patients about what to expect. What their symptoms mean, how do we monitor this? How do we take all of these medicines and do the lifestyle things in our real lives. Making sure we’re doing proper determinants of health screening.
This is a journey we go on with our patients. It’s not a one-time consult and send you out into the world, hopefully. We really are on this life-long journey with them and really building on the support that each person needs. And and trying to personalize that.
And then, the second piece of that is shared decision-making. I think it’s really important to understand what are the patient’s goals?
We have our goals in terms of optimizing medicines and looking at rhythm control and just various things, weight loss for these patients. But we really do need to understand what are the patient’s goals, health, and make sure that we’re letting them drive their health ship.
Kathy Wood (guest): (06:21)
I think that’s so important. You mentioned earlier this morning about the importance of the integrated team and bringing pharmacy in to help with medications, and social workers, and behavioral therapists to help with lifestyle modification. I think that’s a really important point that we stress is the importance of an integrated team when dealing with both types of patients.
Geralyn Warfield (host): (06:46)
When you’re talking about integration, think it’s also important that the family, the caregivers, the community, wherever that individual is, also understands what’s happening. What kind of strategies can we offer to those individuals to help these patients navigate this complexity?
Kathy Wood (guest): (07:02)
And that’s part of the integrated team is the family and the caregiver. And the model that you’ll see illustrated in the European AFib guidelines stresses that you incorporate the family in that. So, we welcome patients to bring their families in for discussions. In the beginning, when they learn about the disease and the treatment options, as well as the shared decision-making conversations because it’s important that the patient have that support as well.
As well as using patient education tools and websites that then the patients can go back and visit after they leave the clinic.
Eryn Bryant (guest): (07:42)
And our heart function wellness clinic, and this is for patients with heart failure specifically, many of which are AFib, part of the intake that we do is asking the patient who are your two, three health support people?
And then I also ask them, who buys the groceries, and who cooks in your home? How many times are you eating in the home versus eating out? So, it’s pretty comprehensive. And as part of that then, if we can link this person to nutrition support, if that’s their need, then we encourage them to bring along whoever’s actually preparing the food and doing the cooking for them if it’s not the patient themselves, so that they’re also hearing this information.
Same for social determinants of health screening is understanding do they have access to their appointments, who does the driving, how do they get to and from ? And so really by understanding those barriers we can link—especially as nurses and advanced practice nurses—we can link patients, hopefully, to resources to that that support them and their family.
Geralyn Warfield (host): (08:47)
You talked a little bit earlier, Kathy, about the rate control and alluded to rhythm control as well. What are the latest guidelines for these patients?
Kathy Wood (guest): (08:54)
So, there was an important paper that we should talk about called the EAST trial that came out of Europe in 2022 I believe. And it looked at the consequences of living with AFib in rate control and rhythm control.
And the patients who were on rhythm control as well as rate control—or without rate control, just rhythm control—had much better outcomes and less consequences such as heart failure, stroke, and cognitive impairment.
So, it changed the paradigm. Because for so long in the AFFIRM study, it was avoiding rhythm control and we were all about rate control because rhythm control had pro-rhythmic effects. But now we found that the benefits of maintaining sinus rhythm are worth the efforts.
So, it’s moved ablation up in the trajectory, or list of treatment options, so that patients are referred for ablation more readily than they were in the past.
Eryn Bryant (guest): (10:01)
I think that’s important for those of us caring for heart failure patients. Because I can imagine, or I know, that there’s been times when I’ve had patients—that I’m sure others had patients—that are like, “Well, I feel fine. My heart rate’s fine, why do I…?”
And so, it’s nice to have this knowledge and to really understand. And we can educate our patients on we do need to be aggressive with trying to get this rhythm control.
Geralyn Warfield (host): (10:26)
And trying to get that rhythm control more urgently than we had in the past. So, having that as part of our armamentarium of treatment options early on so that we are trying to avoid some of those issues that we have seen in the past with those patients then, too.
Kathy Wood (guest): (10:42)
That’s exactly right. It used to be that you had to fail one or two different antiarrhythmics before you were referred for an AFib ablation. But now, AFib ablation is considered a primary treatment, just such as antiarrhythmics and rate control.
Geralyn Warfield (host): (11:00)
We’re going to take a quick break, and we will be right back.
Geralyn Warfield (host):
And we’re back with some more information about that interconnectedness between AFib and heart failure. And Eryn, you had mentioned earlier in our conversation about the clinic where you work. Could you describe that a little bit more because it’s a really intriguing model.
Eryn Bryant (guest): (11:17)
So, I think we all know that for our heart failure population and our AFib population, in the guidelines, for both, it stresses that one of the first things we should think about and what we should be talking about with our patients is lifestyle modifications: healthy diet, and activity, and sleep, and all these things.
But the reality is it’s a challenge to do in our practice with all the other things that we are thinking about: medicines, GDMT, procedures, managing symptoms, etc.
And so, what my colleagues and I were finding is that we were managing disease, and kind of focusing on survival, and keeping people out of the hospital which is of course important.
But we didn’t feel like were helping people, partnering with them, to live vitally, to live well, to feel good, to really restore their health, and sense of confidence and purpose.
And so, we founded this heart function wellness clinic. We thought that name was a little more positive than heart failure. To really give people the tools, and support to implement lifestyle change, And, we’ve opened this up to be a pretty broad definition for a referral base, so we have lot of people who have a lot of patients from our EP colleagues with AFib and stage B heart failure, or stage C.
And we really can meet the patients where they are. And it’s within an interdisciplinary team. We do a comprehensive cardiovascular risk assessment and lifestyle medicine risk assessment. It’s really rooted in the 6 pillars of lifestyle medicine.
That intake is both with an advanced practice nurse and then also with our behavioral health team who do a pretty comprehensive anxiety, depression screening, motivation screening. And we help the patient set some SMART goals and then link them up to things that they need like nutrition, exercise is medicine.
And the other thing is cardiac rehab. We all know how important cardiac rehab is for our heart failure population and our AFib population. So, we do a lot of cardiac rehab referrals for our patients that qualify and maybe hadn’t understood the importance and hadn’t gotten that referral yet.
Kathy Wood (guest): (13:24)
That’s so important, because I think we want to broach lifestyle modification and losing weight and increasing physical activity. But it’s all how to do it and the support that those patients need to make those behavioral changes.
And I think this wellness center is such a brilliant idea because it’s really stressing the positive that patients can do to control the situation, as well as supporting them through that. So that’s really a great feature.
Eryn Bryant (guest): (13:56)
Absolutely. I think that the conversation I have a lot with patients is knowing what to do, and knowing how to do it and implement it into our lives, are kind of two different skill sets.
And so, we want to give both education and do proper assessments but also understand and give them mental health and behavioral health support, and how do we build habits and maintain things.
And it’s just been so gratifying and I think people are ready for this. I really find my patients are ready for this education, and people want to understand how to feel better. They want to take some control and have some autonomy over their lives.
I’m really excited about lifestyle medicine, kind of this movement that’s growing, both from patient support, provider support. And I think we all know it’s important, but I think now there’s this call to action to really implement it in our clinic for our patients because we want to give them the best.
Kathy Wood (guest): (14:50)
A lot of providers have mentioned how difficult it is to broach the subject of lifestyle modifications without saying, “You need to lose weight. You need to be more active.”
So, one of the PCNA discussions that we’ve had is how to broach it with a statement of, “Are you aware of the new research showing that up to a 10% weight loss can reverse AFib from persistent to paroxysmal, or can decrease your frequency of episodes if you’re paroxysmal?” So those kind of ways of entrée into that discussion is a little more positive than, you know, “You need to do this, this, this, and this.”
Geralyn Warfield (host): (15:33)
And speaking of having a conversation that is more collegial than perhaps we’ve seen in the past, what do we do about these patients that are juggling multiple medications? How do we help them be successful? Because we know as human beings, we like to do what we like to do. And if you’ve given me four heart failure meds, obviously I can get by with one. I only need to take this one pill.
Obviously education is important, how do how else do we help?
Kathy Wood (guest): (16:04)
Yes, I think there’s some great tools online. There’s a great PCNA website that talks about patient education and has a toolkit that helps patients address some of these issues, as well as a form about getting medicines that are more expensive paid for and how to start that process. So, it’s really a great feature that helps often.
I know a lot of our NPs use apps on their phones such as GoodRx or other apps that direct them to help the patient of which pharmacist has the medicine for a cheaper price and helps the patients negotiate some of that.
But the focus on adherence is really important because it’s timing. Some are once, some are twice, some are three times a day, and it can be overwhelming. So, I think that’s part of the shared decision-making conversation that Eryn mentioned earlier. And what kind of lifestyle does this patient have?
And so, we can tailor the medication so that it might be a once-a-day that we do instead of a twice-a-day. Certainly, that’s true with anticoagulants and some of the rhythm control medicines can even be ordered as ‘pill in the pocket’ so they take it when an episode starts, and they don’t need to take it every day.
So, there’s different ways to work the strategies, but it brings the patient into the conversation and more of a shared decision-making.
Eryn Bryant (guest): (17:33)
Absolutely. And I think we as providers have maybe a best-case scenario. It is amazing when we have a med list, we’re checking all of our guidelines, and we’ve optimized everything, and it looks really good. So, we have this best-case scenario.
But then, I think we also have to remember that for this person sitting in front of us, we might have a best realistic case scenario. And I think it’s just having direct but compassionate conversations, providing education, non-judgmental, really just understanding, like you mentioned, Kathy.
“What does your life look like? Do you work third shift? What are your kids’ schedules? When do you have to get your kids off the bus? Then do you have to jump in the car and drive an hour?” We’re probably not going to do diuretics right before that.
It’s individualized medicine and it’s having those conversations. And I think it really does start by just explaining to patients or having the discussion about we are on a journey together. And we will figure out what works for you, and letting them make some decisions about what’s realistic for them and what fits their goals of care.
Geralyn Warfield (host): (18:46)
Thank you so much for all of those nuggets of wisdom. I’m going to ask you a rather tough question, which is what one key takeaway do you wish our audience would come away with?
Eryn Bryant (guest): (18:55)
Maybe this, I don’t know if I can just do one, but I’ll try. You know, I think it’s just remembering that we live in this world, oftentimes, as caregivers. And so we are dealing with heart failure and AFib quite a lot. But there are diagnoses. They are life-altering, life-modifying conditions, especially when they’re added one on top of the other and then with other chronic diseases. So meeting the patients where they are, providing the needed support. Understanding the social determinants of health for this person and then leveraging our interdisciplinary care team, really does yield best outcomes for this pretty complex patient population.
Kathy Wood (guest): (19:39)
I think you’re right. I guess what I would offer is that the patients are getting, with these two conditions, patients are getting a lot of negative, is what you can’t do. And so having those conversations with patients about lifestyle modifications and risk management gives them options that they can control the situation.
So, presenting that to them that if you lose 10% of your body weight, you can reverse your AFib.If you spend 150 minutes a week exercising, that can also prevent episodes of AFib. So those kind of instructions, and bringing in lifestyle and risk management, gives patients an opportunity to control the situation. So, I think that’s a good takeaway.
Geralyn Warfield (host): (20:24)
Well, thank you both so very much for being here today and sharing with our audience. Eryn and Kathy, we are really appreciative of your time and expertise. This is Geralyn Warfield, your host, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. Visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Atrial Fibrillation
- Heart Failure
Published on
September 2, 2025
Listen on:

PhD, RN, FAHA, FAAN

MSN, NP-C
Related Resources
Online Interactive Guides
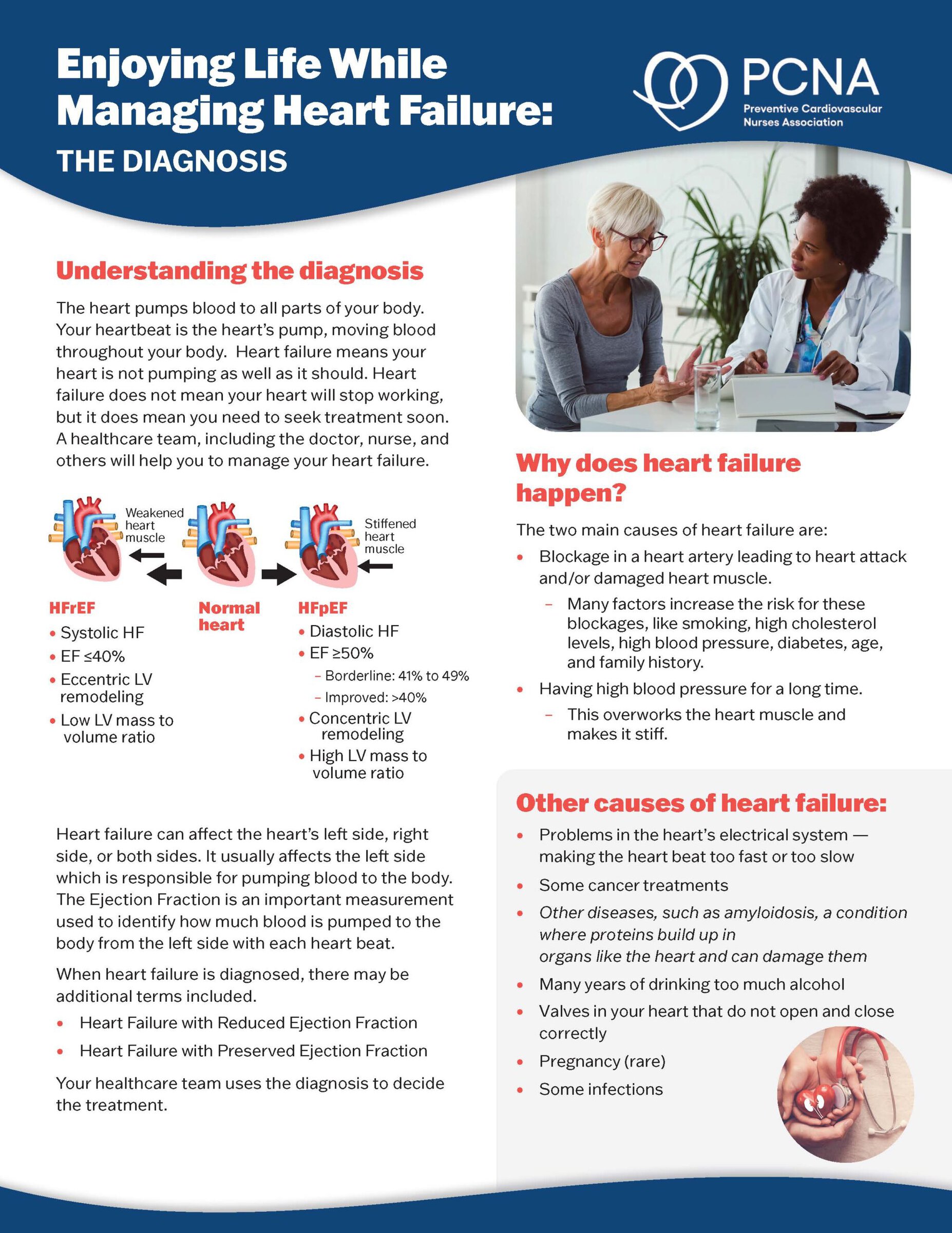
Enjoying Life While Managing Heart Failure Online Patient Interactive Guide
March 12, 2024

Online Interactive Guides
The Beat Goes On: Living with Atrial Fibrillation Online Interactive Patient Guide
July 30, 2025