Information for healthcare providers about the uses of ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring in the diagnosis and management of hypertension. Patient-centered information includes validated blood pressure devices and how to take blood pressure at home.
Components
Components are available to download individually or together as the whole section. You can also view all sections of the Heart Healthy Toolbox.
For Patients
- Taking Blood Pressure at Home
For Providers
- Ambulatory Blood Pressure Monitoring (ABPM) for the Clinician (also available below)
- Home Blood Pressure Monitoring (SMBP vs HBPM) for the Clinician (also available below)
Ambulatory Blood Pressure Monitoring (ABPM) for the Clinician
WHAT IS IT?
An ABPM device is a portable device that offers an accurate 24-hour measurement of blood pressure, providing reliable readings outside the office setting.
It is useful for:
- Confirmation of hypertension (HTN) diagnosis
- Diagnosis of white coat HTN or masked HTN
- Detection of nocturnal HTN, episodic HTN and hypotension
- Surveillance and monitoring with confirmed white coat HTN, white coat effect, masked HTN, and masked uncontrolled HTN
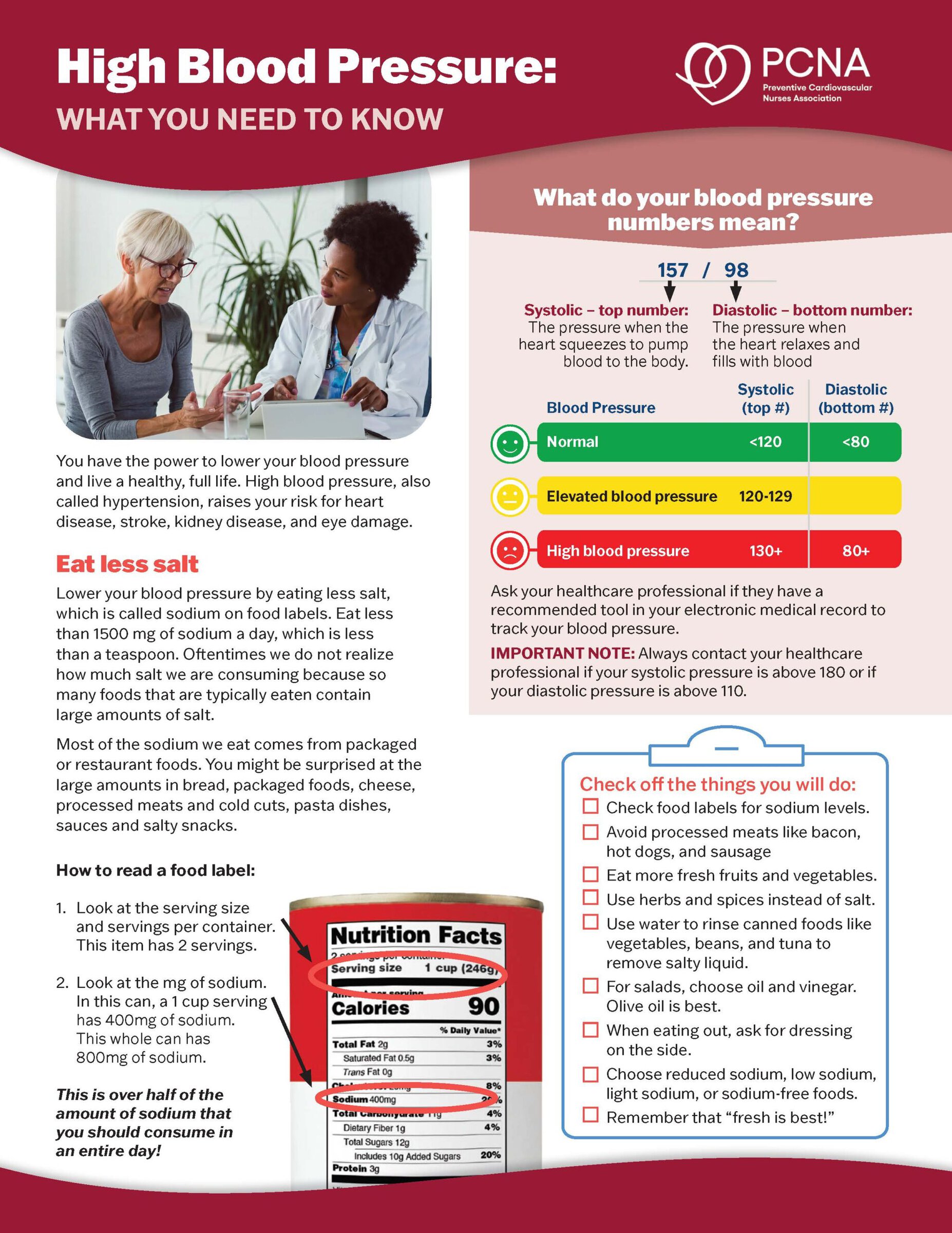
HTN is diagnosed with ABPM when the 24-hour average blood pressure is ≥125/75 mmHg or the average daytime blood pressure is ≥130/80 mmHg.
Nocturnal HTN when the average nighttime blood pressure is ≥110/65 mmHg
HOW DOES ABPM WORK?
- Wearable device, monitors blood pressure measurements over a 24- to 48-hour period, usually every 15 to 30 minutes during the daytime and every 30 to 60 minutes during sleep
- BP cuff applied to nondominant arm unless contraindicated
WHAT CLINICAL INFORMATION CAN BE DETERMINED BY ABPM?
- Mapping of systolic and diastolic BP over the 24-hour period
- Provides daytime, nighttime, and total readings obtained with averages, including heart rate
- Percentages of BP exceeding the upper limit of normal
IS ABPM A REIMBURSABLE PROCEDURE?
Yes. Medicare will reimburse an ABPM test meeting requirements for CMS services; commercial insurance for suspected white-coat HTN; private insurance varies dependent upon the carrier.
Medicare criteria for ABPM reimbursement includes:
- Suspected white coat HTN — average clinic BP of systolic BP > 130 mmHg but < 160 mmHg, or diastolic BP > 80 mmHg but < 100 mmHg on two separate clinic visits with at least two separate measurements made at each visit, and with at least two BP measurements taken outside the office which are < 130/80 mmHg.
- Suspected masked HTN—average clinic BP 120-129 mmHg for systolic BP, or between 75-79 mmHg for diastolic BP on two separate clinic visits with at least two separate measurements made at each visit, and at least two BP measurements taken outside the office which are ≥ 130/80 mmHg.
Commercial carriers common ABPM insurance coverages:
- White Coat HTN
- Masked HTN
- Resistant or labile HTN
- Nocturnal HTN
- Post-prandial or orthostatic hypotension
- Syncope
WHAT REIMBURSEMENT CODES DO I NEED TO KNOW?
CPT code
- 93784 – Report generating software, automated, worn continuously for 24 hours or longer, including recording, scanning analysis, interpretation, and report
- 93786 – Recording only
- 93788 – Scanning analysis with report
- 93790 – Review with interpretation and report
ICD-10 code
- 796.2 – Elevated blood pressure reading without diagnosis of HTN
HOW MUCH IS REIMBURSEMENT?
APBM devices cost around $2,000 to $2,500 each, plus the cost of software
- Medicare: Average $52, depending upon geographic region
- Commercial insurance carriers: Average $89
Dietrich E., Desai R., Garg M., Park H, Smith SM. Reimbursement of ambulatory blood pressure monitoring in the US commercial insurance marketplace. Journal of Clinical Hypertension. 2020;22(1):6–15. doi.org/10.1111/jch.13772
Desai R., Dietrich EA, Park H, Smith SM. Out-of-Pocket payment for ambulatory blood pressure monitoring among commercially Insured in the United States. American Journal of Hypertension. 2020;33(11):999–1002. doi.org/10.1093/ajh/hpaa120
Kronish IM, Hughes C, Quispe K, Viera AJ. Implementing Ambulatory Blood Pressure Monitoring in Primary Care Practice. Family Practice Mgmt. 2020;27(3):19-25.
Home Blood Pressure Monitoring (HBPM) for the Clinician
CLASSIFICATION
| BP Classification | Systolic BP, mmHg* | and/or | Diastolic BP, mmHg* |
|---|---|---|---|
| Normal | <120 | and | <80 |
| Elevated | 120-129 | and | <80 |
| Stage 1 hypertension | 130-139 | or | 80-89 |
| Stage 2 hypertension | ≥140 | or | ≥90 |
| Severe hypertension without symptoms* Patient should call HCP | >180 | and/ or | >120 |
| Hypertensive emergency with any symptoms* Patient should call 911 | >180 | and/or | >120 |
* Symptoms: chest pain, shortness of breath, back pain, numbness, weakness, change in vision, or difficulty speaking
TREATMENT GOALS
Encouragement to achieve SBP <120 mm Hg
If there is a disparity in category between the systolic and diastolic pressures, the higher val-ue determines the stage.
GOALS FOR DIFFERENT DISEASE STATES
Diabetes and chronic kidney failure <130/80 mmHg
HOME BLOOD PRESSURE MONITORING (HBPM)
Diagnosing HTN
• Out of Clinic BP measurements
• Masked and white coat hypertension (HTN)
Follow up/Long term management of HTN
• Titration of BP meds
Adapted from
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the pre-vention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice Guidelines. Hypertension. 2018;71(6):1269–1324. doi.org/10.1161/HYP.0000000000000066
EVALUATING NEED FOR TREATMENT OF HIGH BLOOD PRESSURE (BP)

FREQUENCY OF MEASUREMENT
- For initial use:
- To diagnose HTN, obtain two measurements separated by at least one minute twice daily. Instructed to record readings over 3-7 days. These readings should then be averaged.
- Two measurements with 1-min interval in the morning and in the evening. The measurement should be performed for 7 days (at least 5 days) for the initial diagnosis, and duplicate measurements should be taken 1x or 2x per week or per month for long-term follow-up.
- To assess treatment effects
- At least 12-14 measurements should be obtained, with both morning and evening measurements taken, over a period of one week every month
- Once controlled
- Take at least 2 readings 1 min apart in morning before taking medications and in evening before supper. Optimally, measure and record BP daily. Ideally, obtain weekly BP readings beginning 2 weeks after a change in the treatment regimen and during the week before a clinic visit.
MONITORS
Arm
Monitors that measure the BP in the brachial artery are the most reliable and is the preferred type of monitor. Correct cuff size is important for accurate BP measurement.
Wrist or Finger
At present these devices have failed the validation studies and therefore are not recommended.
Kiosk
Many kiosks have not been validated by standard protocols, and there are limited data on the reproducibility of their readings.
VALIDATED HOME BLOOD PRESSURE MONITORS (HBPM)
Find lists of validated blood pressure monitors at validatebp.org, and stridebp.org
Home measures: HTN is diagnosed if the average BP is > 130/80 mmHg
NUMBER OF READINGS TO MAKE A CLINICAL DECISION
- Take at least 2 readings 1 min apart in morning before taking medications and in evening before supper. Optimally, measure and record BP daily. Ideally, obtain weekly BP readings beginning 2 weeks after a change in the treatment regimen and during the week before a clinic visit.
- BP should be based on an average of readings on ≥2 occasions for clinical decision making.
- Patient education should include appropriate BP technique, checking validation of home devices including return demonstration, how to handle unusual readings, and BP reports.
RELATIVE CONTRAINDICATIONS TO HBPM
- Patients who have atrial fibrillation or other arrhythmias such as frequent ectopic beats.
- Patients who may become very anxious with elevated readings.
For adults with uncontrolled hypertension, an integrated treatment model that includes accurate BP measurement, prompt treatment, patient engagement, and ongoing review of HBPM is recommended to improve BP control.
Adapted from:
Shimbo D, Artinian NT, Basile JN, et al. Self-Measured Blood Pressure Monitoring at Home: A Joint Policy Statement From the American Heart Association and American Medical Association. Circulation. 2020;142(4):e42–e63. doi.org/10.1161/CIR.0000000000000803
McCarthy CP, Bruno RM, Rahimi K, Touyz RM, McEvoy JW. What Is New and Different in the 2024 European Society of Cardiology Guidelines for the Management of Elevated Blood Pressure and Hypertension? Hypertension. 2025;82(3):432–444. doi.org/10.1161/HYPERTENSIONAHA.124.24173
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice Guidelines. Hypertension. 2018;71(6):1269–1324. doi.org/10.1161/HYP.0000000000000066
Supported by independent educational grants from Merck & Co, Inc. and Novartis Pharmaceuticals Corporation.
Resource Details
Reviewed on
September 3, 2025
Language(s)
- English
Download Resource
Related Resources