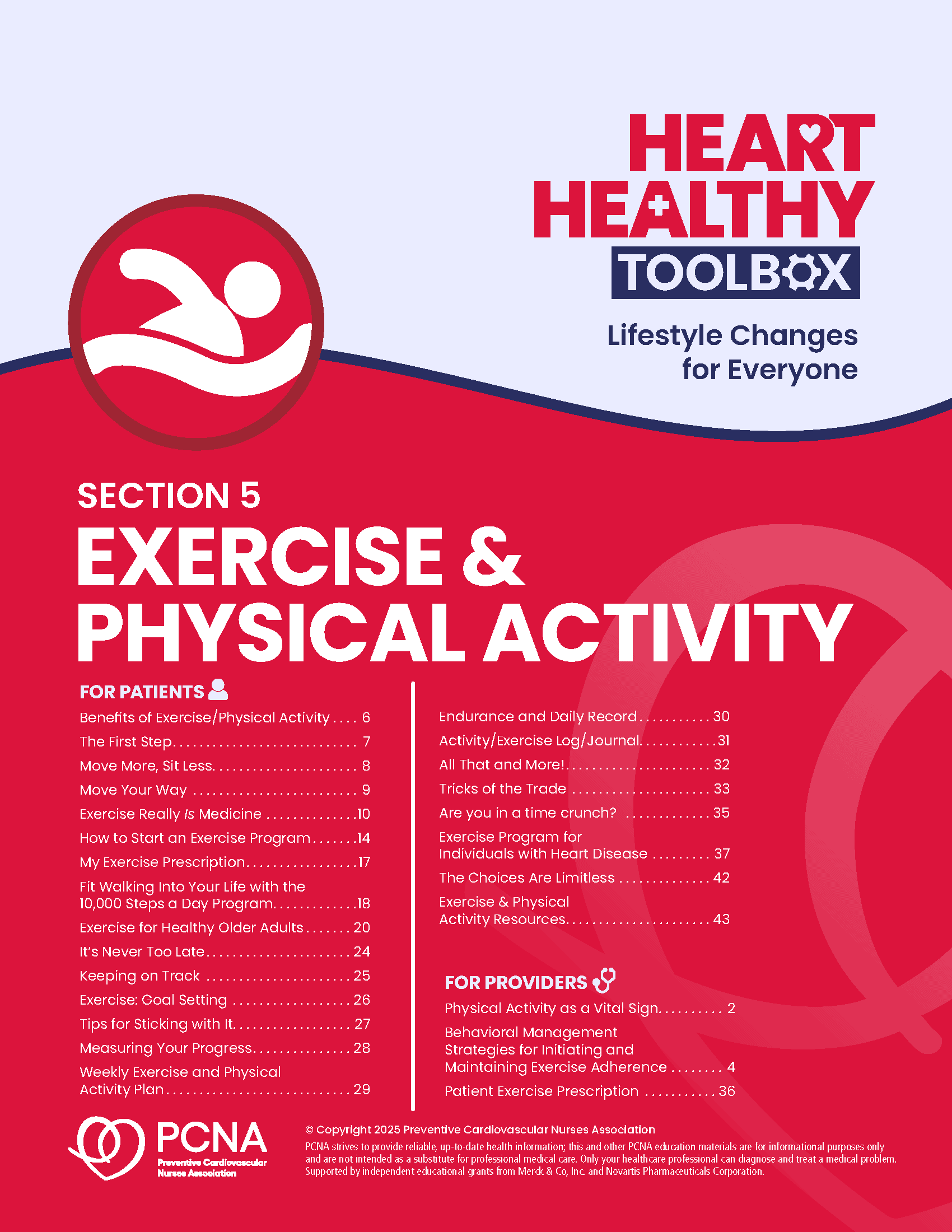
Focused on the importance of activity for health at all ages and fitness levels, this section includes tools for both patients and HCPs. From exercise prescriptions and adherence to easy-to-follow instructions and tracking documents, these resources provide a complement of information and action items to help patients move more.
Components
Components are available to download individually or together as the whole section. You can also view all sections of the Heart Healthy Toolbox.
For Patients
- Benefits of Exercise/Physical Activity
- The First Step
- Move More, Sit Less
- Move Your Way
- Exercise Really IS Medicine
- How to Start an Exercise Program
- My Exercise Prescription
- Fit Walking Into Your Life with the 10,000 Steps a Day Program
- Exercise for Healthy Older Adults
- It’s Never Too Late
- Keeping on Track
- Exercise: Goal Setting
- Tips for Sticking with It
- Measuring Your Progress
- Weekly Exercise and Physical Activity Plan
- Endurance and Daily Record
- Activity/Exercise Log/Journal
- All That and More!
- Tricks of the Trade
- Are you in a time crunch?
- Exercise Program for Individuals with Heart Disease
- The Choices are Limitless
- Exercise & Physical Activity Resources
For Providers
- Physical Activity as a Vital Sign (also available below)
- Behavioral Management Strategies for Initiating and Maintaining Exercise Adherence (also available below)
- Patient Exercise Prescription
Physical Activity as a Vital Sign
Assessment and Exercise Prescription
Becoming more physically active may be the most beneficial thing your patients can do to improve their health. Patients with lower baseline fitness levels may experience the greatest improvements. Guidance and support from you will give patients the tools and confidence they need to get started with a safe and effective exercise program.
Steps You Can Take to Help Your Patients Become More Physically Active:
- Make exercise a vital sign.
- Consider adding a question to your office visit check in template. Do you exercise? If so, what type?, how long?, how hard?, and how often? Many health systems have added this question to their electronic medical record to ensure consistency and convenience. Documenting physical activity at every visit allows you to track patient’s progress over time. NOTE: For patients with Peripheral Artery Disease, a physical activity program can help reduce pain and improve circulation. See section 14, Peripheral Artery Disease.
- Provide advice.
- If patient is inactive, briefly discuss the benefits of exercise. Give them a copy of the tool, “All That and More.” You may also encourage them to move more throughout their day even if they don’t feel ready to start an exercise program. The tool “Move More, Sit Less!” provides great suggestions to for increasing daily activity, even without a structured exercise program.
- Assess.
- If patients are ready to start an exercise program, determine if the patient is healthy enough to exercise independently. If they have no cardiovascular symptoms and are low risk, provide them with an exercise prescription and advice on starting an exercise program. Use the tools “The First Step” and “My Exercise Prescription” as a basis for your instruction.
- Assist.
- If your patients need more support in starting an exercise program, consider a referral to a health and fitness professional. Your health system’s cardiac rehabilitation or physical therapy programs may be good resources.
- Become familiar with other local resources. Senior centers and the YMCA may offer chair or water-based exercise programs for your patients that have orthopedic or balance problems.
- The tool, “It’s Never Too Late!” is a resource for older patients as well as those with health concerns.
- Encourage patients to report any exercise-induced symptoms such as shortness of breath, chest pain, excessive fatigue or orthopedic concerns
- Arrange follow up.
- Have your patient come back to discuss their progress with exercise and to update their exercise prescription as needed. This is a good time to problem-solve any barriers to exercise and help patient’s problem-solve ways to stick with the plan.
- “Tricks of the Trade” provides good suggestion for overcoming common situations that get in the way of regular exercise and “The Choices are Limitless” tools provides suggestions for dealing with travel, weather, boredom or fatigue.
Visit the American College of Sports Medicine’s Exercise is Medicine for more resources and tips regarding helping your patients become and stay active!
Behavioral Management Strategies for Initiating and Maintaining Exercise Adherence
| Techniques | Practical Applications/Recommendations |
|---|---|
| Preparation | Establish realistic expectations for patients new to exercise/ physical activity. |
| Shaping | Begin the exercise program at a dosage (frequency, intensity, duration) that is comfortable for the patient and increase slowly until an optimal level is attained. |
| Goal-setting | Goals should be individualized and based on the patient’s physiologic and psychological status. Goals that are specific, yet flexible, are more effective than longer term goals. |
| Reinforcement | Patients should be queried as to what reinforcers (rewards) would work for them. Rewards might include certificates of achievement, attendance records, or getting a medal for having completed an event (10K run). |
| Stimulus Control | Environmental cues or stimuli (written notes, watch alarms, dates on a calendar) may be used to remind patients to maintain their exercise commitment. Having a routine time and place for exercise establishes a powerful stimulus control. |
| Contracting | A behavioral contract has been shown to enhance the commitment to exercise. Signing the contract formalizes the agreement and makes it more significant. |
| Cognitive Strategies | Patients should be oriented to the advantages and disadvantages of exercise. Individuals who select their own goals generally demonstrate better adherence. |
| Generalization Training | Specific steps should be taken to generalize the exercise habit from a structured class or home setting to other environments (travel, work, etc). |
| Social Support | Support from family, friends, coworkers, or other trusted individuals can benefit patients throughout the process of behavior change. An exercise partner, for example, may help keep a patience on track with activity. |
| Self-management | Patients should be empowered to use behavioral tools or encouragement in daily life. They can focus on increased self-esteem, enjoyment of the exercise itself, and the anticipated health and fitness benefits. |
| Relapse Prevention Training | Prepare patients for situations that may produce relapse and ways of coping with them so that a complete relapse is avoided. Relapses should be viewed as inevitable challenges, rather than failures. |
Adapted from: American College of Sports Medicine’s Guidelines for Exercise Testing and Prescription (11th ed.), Lippincott, Williams, and Wilkins.2022.
Supported by independent educational grants from Merck & Co, Inc. and Novartis Pharmaceuticals Corporation.
Resource Details
Reviewed on
August 29, 2025
Language(s)
- English
Download Resource
Related Resources