Hypertension control is an intersection of factors at the patient, provider, system, and societal levels. Guest Yvonne Commodore Mensah, PhD, MHS, RN, FAAN, FAHA, FPCNA, describes actions in the clinic, in the community, and in advocacy to help address this disease that affects 1 in 2 U.S. adults. Learn about validated devices for measurement, strategies for effective community screening, and the impacts of health inequity on our patients.
Episode Resources
[00:00:00] Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Thank you so much for joining us today. We’re here with Dr. Yvonne Commodore Mensah. We’re going to talk about hypertension. So, Yvonne, I’m going to have you introduce yourself and then we’ll get started on our content.
Yvonne Commodore Mensah (guest): Thank you so much, Geralyn, for having me. Hello everyone. I’m Yvonne Commodore Mensa. I’m an Assistant Professor at Johns Hopkins School of Nursing. I also have a joint appointment at the Department of Epidemiology at the School of Public Health.
I am a nurse first, but also a cardiovascular disease epidemiologist. My focus is on understanding disparities in cardiovascular health, [00:01:00] but more importantly, understanding how we might intervene to eliminate these disparities and advance equity in cardiovascular health outcomes. I’m also interested in addressing social determinants of health to promote cardiovascular health in underserved populations.
Geralyn Warfield (host): So, you have your fingers in a lot of different topic areas, and so we’re going to narrow it down today and focus a little bit specifically on controlling hypertension. And you, as well as anybody else who’s listening to this podcast, understand that hypertension is a risk factor for cardiovascular disease and that hypertension, overall, is not very well controlled. And do you want to talk a little bit about that lack of control that we have over hypertension? And then we can talk a little bit about what might be some next steps that we can do to help our patients.
Yvonne Commodore Mensah (guest): Geralyn, as you rightfully said, hypertension is a major [00:02:00] risk factor for cardiovascular disease, stroke, kidney disease, and recently some studies have shown that hypertension is linked with vascular dementia. So, we know that this is a major risk factor that has to be addressed.
Unfortunately, in the U.S., over 108 million adults—or 1 in 2 U.S. adults—have hypertension. And this is a major public health and it’s also a clinical, challenge. So even beyond the U.S., globally, we know that hypertension, again, is a major contributor to preventable deaths that are attributed to cardiovascular disease.
So, bottom line is the burden is high, the risk is also high. We also know that, in terms of hypertension, there are disparities in the prevalence of hypertension. [00:03:00] So, in terms of the prevalence, we know that there are sex differences, or disparities by sex. So, men are more likely to have hypertension than women.
But we also know that in terms of racial and ethnic minorities, Black men are more likely to have hypertension than white men, for instance. And among women, Black women, again, have the highest. prevalence of hypertension. So, there are established disparities in hypertension.
But we also care about hypertension control.
Although we know that the burden of hypertension is high, we also know that only about 1 in 5 adults who have hypertension actually have their condition under control. We know that controlling blood pressure lowers the risk for cardiovascular disease, stroke, kidney disease, and other complications. We also [00:04:00] know that there are effective and affordable medications that treat hypertension and lower cardiovascular disease risk.
But unfortunately, there are many reasons why we haven’t done a great job with controlling hypertension in the US and some of these reasons include patient-level issues or patient-level factors such as adherence, or literacy in terms of understanding risk factors for hypertension.
But they’re also clinical challenges. It’s not all on the patients. We know that sometimes clinicians do not intensify treatment when blood pressure control is not achieved. We also know that sometimes clinicians don’t do a great job of interacting with patients, in terms of cultural humility and communicating effectively with patients, so that ultimately interferes with the quality of care that [00:05:00] is provided.
We also know that there are system-level issues, right, in terms of not having an adequate healthcare workforce to treat, or deal with the burden of hypertension. And so, as a society too, we know that there are societal barriers and factors.
We know that there are issues surrounding healthcare access. There are over 30 million uninsured Americans who ultimately will have challenges with controlling their hypertension if they don’t have access to clinicians. So, when we think about the reasons for the poor blood pressure control in the U.S., it’s not one thing, but an intersection of different factors at the patient level, provider level, system level, and the societal levels as well.
Geralyn Warfield (host): Wow. You have really provided a great cultural context, a great global context, and a great clinician context for hypertension control or lack [00:06:00] thereof that we have here in the United States and elsewhere. If you were speaking specifically about what a cardiovascular care clinician can do each and every day in practice, what kinds of tips or even resources might you offer them?
Yvonne Commodore Mensah (guest): There are definitely solutions to tackle this challenge of poor blood pressure control as cardiovascular clinicians, and let me be specific, as cardiovascular nurses too. We play a critical role in addressing the burden of hypertension and eliminating these disparities.
The first thing I’ll touch on is education. We need to educate patients about the importance of, one, adhering to prescribe therapy, but also, lifestyle modifications. So, the importance of physical activity, dietary modification, [00:07:00] so, exercise is medicine. Patients need to understand that being more physically active can also help to improve your blood pressure control.
Also adhering to what we call the DASH diet, the Dietary Approaches to Stop Hypertension. That is an effective approach to improved blood pressure control.
Limiting alcohol use. So, if someone drinks, limiting, if they’re, it’s a woman, so limiting the alcohol intake to one drink a day, and if they’re a man, to no more than two drinks a day.
So, lifestyle modification. I think nurses do a great job of educating patients, and these are things that we need to emphasize.
Another thing we need to address is social determinants, right? So, there are many reasons why, for instance, a patient may not be able to adhere to these lifestyle guideline, or be able to consume a [00:08:00] diet that is high in fruits and vegetables. For instance, if they live in a neighborhood, and that may be classified as what we would call a food desert, right, where they have limited access to healthy and affordable foods, they may not be able to adhere to this DASH diet, right? If unhealthy foods are more convenient and are cheaper, our patients are going to opt for those unhealthy options, and that would ultimately interfere with their blood pressure control.
So, really understanding a patient’s context, right? So, are they dealing with issues surrounding food insecurity, right? Are they in a safe environment? So, it’s one thing to tell a patient you should be more active, you should walk around in your neighborhood. But if we don’t really understand if their neighborhood is safe enough to walk in, then it really, I feel like we lose [00:09:00] credibility with our patients if we don’t understand their social needs and their social context. So, understanding these social determinants and how that might impact blood pressure control.
And I think cardiovascular clinicians also play a critical role in advocacy, right, to address these social determinants of health. So, everyone, every American and globally, everyone has access to universal health care where they can get quality care, to be able to improve their health. And cardiovascular clinicians, and nurses in particular, have a critical role to play in in advocacy efforts.
Geralyn Warfield (host): We have been listening to Dr. Yvonne Commodore Mensah discuss hypertension and disparities in the assessment and management of that. We’ll be back in just a minute to talk about that a little bit more.
Geralyn Warfield (host): We’re back with Yvonne Commodore [00:10:00] Mensah, talking about hypertension, particularly for those who are working in cardiovascular prevention and treatment.
And I have a specific question for you, and it has to do with accurate assessment of blood pressure and how that factors into this whole process.
Yvonne Commodore Mensah (guest): That’s a great question. I would say that the first step in controlling blood pressure is measuring blood pressure accurately. And we know that in many clinical settings, nurses are responsible for measuring blood pressure and we need to do a good job of measuring blood pressure accurately because those blood pressure values will be used to make clinical decisions.
So, the first step is measuring blood pressure accurately, and there are a number of resources that are available in terms of understanding how to position a patient, instructions that can be provided in terms of not crossing their legs, emptying their bladder before the blood pressure measurement is [00:11:00] performed, the positioning of the arm, the positioning of the cuff, selecting the correct cuff size. So, these are all factors that influence our, our ability to obtain an accurate blood pressure measurement.
And so, there’s a resource called validatebp.org that provides a listing of validated blood pressure devices. So, we need to understand which blood pressure devices are validated and accurate in order to obtain accurate blood pressure readings. So, anyone can refer to this resource or website to understand which clinic-based devices are validated, which home blood pressure devices are validated.
And a patient may come up to you and ask, “Well, there are a number of devices on online. If you go to a local pharmacy, there are a number of devices [00:12:00] that are supposed to measure blood pressure, but which ones are accurate?” So, all cardiovascular clinicians should be aware of this resource and share this information with patients to allow them to select an accurate device because not all devices are created equal. And so, we have a critical role in terms of measuring blood pressure accurately.
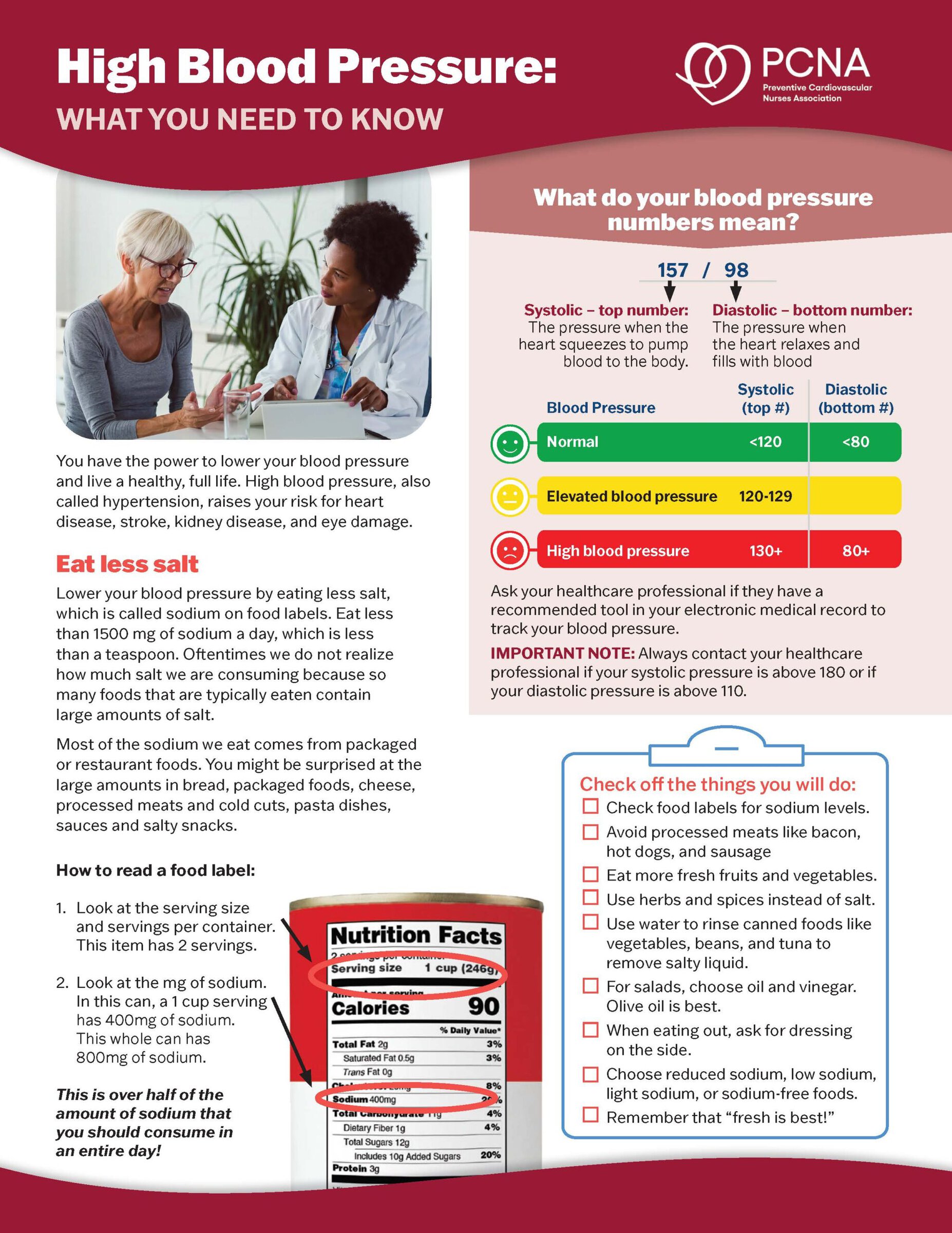
And so, beyond measuring it accurately, educating patients about what to do with those numbers, what do those numbers mean? So, when we provide counseling on, for instance, self-measured blood pressure monitoring, we need to stress the importance of sharing those blood pressure readings with a clinical team. Right?
And so there are a number of ways to do that. There are some health systems that provide patient portals that patients can enter their blood pressure readings. Sometimes patients actually take the devices with them to, for their office visit so that the [00:13:00] clinician can assess or look at trends in the blood pressure values to really inform the need to adjust their medications, for instance, to promote blood pressure control.
Geralyn Warfield (host): There’s one other thing about hypertension and communities, if you wouldn’t mind, that I would like to ask. And it has to do with doing community outreach events. I know that you have some experience with those, and I know with our recent pandemic, that has been a challenge and maybe even a challenge and a half, for all providers to try and get out into the community and meet these individuals who might not have a primary care provider, who don’t necessarily know their numbers, who maybe haven’t had a, a blood pressure reading in months, years, decades even. Could you talk just briefly about what it takes to do a successful outreach event?
Yvonne Commodore Mensah (guest): As you highlighted, Geralyn, the COVID-19 pandemic has taught us a number of lessons. One of them is [00:14:00] the need to be in the community to meet people where they are. When it comes to promoting cardiovascular health, I think all clinicians, cardiovascular nurses, physicians, regardless of your profession, we need to be more visible in communities to promote health education, increase awareness of the importance of cardiovascular health. And so, in terms of community outreach, in some of my work, and in working with students and trainees at Johns Hopkins, we’ve learned a number of important lessons when it comes to community outreach.
The first is identifying a community leader who may serve as the gatekeeper, who will, essentially, give you their stamp of approval to conduct the community outreach. And so, reaching out to this person, understanding their [00:15:00] concerns, explaining the purpose of the outreach.
And so, one of the concerns I’ve heard in in my work is often, researchers, clinicians go into communities, they take information, and they leave and there’s never a benefit. So that’s often described as helicopter-type of research: you go in, collect data and leave. I think from the very outset, it has to be clear the purpose of the outreach, and understanding what the needs and concerns are for the community.
I’ll share an example of a community blood pressure screening event that we had two weeks ago where the, there was this gentleman who was walking by and I walked over to him and I said, “We are conducting a free blood pressure screening. Are you interested in understanding your blood pressure?” And he looked at me and said, “Oh, my blood pressure’s fine.”
I said, “Okay, do you mind if we check it anyway?” And we checked his blood pressure [00:16:00] and it was 160/100 and we checked it three times a minute apart. We used an accurate device, a validated device, and he was shocked. And he said, “Well, my blood has always been normal.”
And I asked him, “When was the last time you checked your blood pressure?” And it had been three years. So, a lot can happen in three years.
And this screening event was conducted at a church. So, faith-based settings offer, really, an ideal setting to meet people where they are, and meet people in a setting where they feel like they trust whoever’s in that space. And it’s also convenient for them. And so, for this participant in the screening event, I sat down with him to talk to him about his access to healthcare. And he said he hasn’t seen a doctor in over three years.
Like you said, the COVID-19 pandemic [00:17:00] has really disrupted primary care. So, for someone like him, it’s important to follow up and be linked to care. And so, one of the things we do, and, and to answer your question directly, to the importance of linkage to care.
So, it’s not enough to screen people for hypertension and tell them that they have hypertension, but we have to link them to care and ensure that they see a clinician who will officially diagnose them with hypertension, who will prescribe medications—not only medications, but educate them on the importance of lifestyle modification.
And that’s something we also did during our, our conversation with him, which was to talk about things that he can do, immediately, to improve his blood pressure control in terms of being physically active and changing his diet, limiting his intake of sodium.
So, those are the key elements: preparation, identifying a team, too. So, we have been very fortunate to have [00:18:00] very eager students who are truly passionate cardiovascular nurses who understand the importance of, of health equity and community outreach, who have in many cases volunteered.
So as part of our recent project, and the grant PCNA received from Pfizer, we’ve had the opportunity to engage some of our students in assisting with the blood pressure screening and, but also screening for atrial fibrillation.
And, they’ve noted that really, those experiences really helped to solidify why they chose nursing as a career. The opportunity to teach people, to educate, and interact with people in the community setting. So those are some lessons that I’ve learned so far
Geralyn Warfield (host): So, is there anything that you would like to add that I neglected to ask about already?
Yvonne Commodore Mensah (guest): That’s a great question. I think [00:19:00] as the most trusted profession, nurses really are well positioned to be strong advocates for health equity. I think regardless of the setting that you find yourself in, it’s important for nurses to position themselves to really understand the barriers to, for instance, blood pressure control, cardiovascular health, and really speak up on behalf of patients in the clinical setting, but outside the clinical walls to also advocate for policies that will help to advance cardiovascular health equity.
Geralyn Warfield (host): We have learned so much from you today. It’s been a great honor to spend time with you, Yvonne Commodore Mensah, talking about hypertension and the community, and reaching people where they are. We’ll see you next time. This is your host, Geralyn Warfield.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Hypertension
Published on
April 4, 2023
Listen on:

PhD, MHS, RN, FAAN, FAHA, FPCNA
Related Resources