Health Equity: Cardiovascular Nurses’ Role
Advancing Health Equity
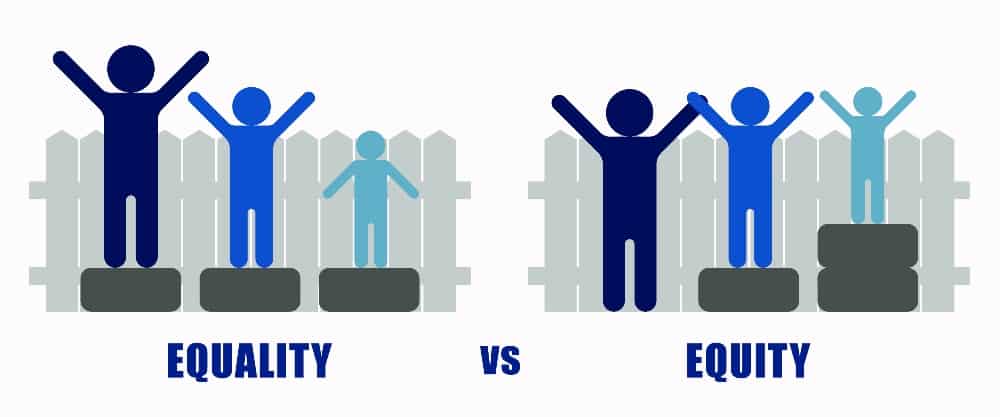
Health equity has been defined as “When every person has a fair opportunity to attain his or her full health potential, and no one is disadvantaged from achieving this potential because of social position or other socially determined circumstances”.1 This is a cause that cardiovascular nurses can support. All nurses are obligated by the American Nurses Association Code of Ethics, to provide fair and equal treatment that respects the “inherent dignity, worth and unique attributes of every person … regardless of the factors contributing to the person’s health status”. 2 The nursing profession is grounded in the principles of community health advocacy and social justice.
There are disparities in the prevalence of cardiovascular disease (CVD) and associated risk factors in the United States and globally. Racial and ethnic minority populations in the United States, particularly Black people, have higher mortality from CVD and a higher prevalence of CVD risk factors such as hypertension, diabetes, and obesity.3,4 Additionally, Black and Indigenous women in the United States also experience the highest cardiovascular-related maternal mortality and morbidity rates.5,6 However, these disparities cannot be attributed to a biological predisposition to CVD and underlying conditions but rather to existing social, economic, and health policies that disproportionately affect racial and ethnic minority populations.7 The COVID-19 pandemic has magnified existing disparities and increased awareness of the impacts of structural and systemic racism in all aspects of society-healthcare, policing, and education.
The recent report of Future of Nursing 2020-2030: Charting a Path to Achieving Health Equity8 has put forward a charge for nurses to advance health equity and highlighted the crucial contributions of nursing to addressing social determinants of health and health equity in the United States. Additionally, this report challenges nurses to advocate for lasting local, state, and federal policy changes that ultimately drive the health of populations.
Roles of Cardiovascular Nurses in Advancing Health Equity
Recognizing the role of structural racism in health care
Cardiovascular nurses should recognize the impact of structural racism on cardiovascular disease risks and outcomes, specifically among individuals who identify as racial and ethnic minorities. Several non-biological factors increase cardiovascular disease risk and include discrimination, marginalization, and racism in health care.7,9 Prior studies have revealed racial and ethnic differences in cardiovascular therapy and invasive procedures in the management of cardiovascular disease, after accounting for potential factors which may explain the disparities in outcomes.10,11 Studies have shown that Blacks are less likely to seek emergent care when experiencing acute myocardial infarction12, which may increase their risk of adverse outcomes.
Assessing and addressing social needs of patients
Cardiovascular nurses can improve health equity from the individual to system level by assessing and addressing social needs. The National Academies of Sciences, Engineering, and Medicine report “Integrating Social Care into the Delivery of Health Care” has prioritized five areas that can facilitate the integration of social care into health care, including adjustment, assistance, alignment, advocacy, and awareness.13 Social needs screening tools such as the Protocol for Responding to and Assessing Patient Assets, Risks, and Experiences (PRAPARE)14 can help cardiovascular nurses and other members of the healthcare team to assess and address social determinants of health.
Advocating for equitable access to healthcare
Cardiovascular nurses should be emboldened to advocate for health care access for people, families, and communities worldwide. In the United States, the Affordable Care Act sought to close gaps in health care access that left millions of Americans without health insurance by expanding Medicaid coverage and the provision of subsidies to persons living in poverty and with low income.15 However since 2017, there has been an uptick in the number of uninsured Americans, rising from 26.7 million in 2016 to 28.9 million in 2019.15 Cardiovascular nurses should support legislation to expand Medicaid coverage, which has been shown to reduce mortality and hypertension and improve diabetes control.16,17 Furthermore, cardiovascular nurses should advocate for healthcare policies that ensure that all people, regardless of their race, ethnicity, gender, socioeconomic background, or ability, have access to high-quality and affordable cardiovascular medications to improve their cardiovascular health.
Promoting diversity, equity, and inclusion in nursing
PCNA recognizes the importance of diversity as a critical step towards advancing health equity. Cardiovascular nurses should reflect the rich diversity of the populations they serve. Thus, our organization commits to supporting efforts to recruit and retain nurses from diverse backgrounds into the cardiovascular nursing community. Furthermore, we strive for cultural humility and to deliver care that reflects our patient’s unique perspectives, beliefs, and backgrounds.
The Health Equity Summit
On November 2 and 4, PCNA, in collaboration with the Association of Black Cardiologists, hosted a Health Equity Summit which offered cardiovascular nurses and other health care professionals solutions, provide tools and tips, and outline steps that can be taken at the personal, local, and national level to close the gap in health disparities.
Presentations included the following topics:
- Defining Health Disparities and Inequity: What They Are and Why We Should Care
- Health Disparities and Cardiometabolic Risk Reduction
- Health Disparities and Social Determinants of Health: Community Assessments and Tools
- Systemic Racism and Implicit Bias: Impact on Our Patients and Our Communities
- Preparing a Diverse Nursing Workforce to Meet the Healthcare Needs of a Diverse Population
Visit our continuing education library to view the recordings of these talks.
Leading with the Heart
As the most trusted profession, nurses are well-positioned and morally obligated to be strong advocates for cardiovascular health equity. PCNA commits to social justice and eliminating disparities in cardiovascular health, supported by nurses from diverse backgrounds, through the development of professional and patient education, research, leadership, and advocacy. We will “lead with heart” to ensure that all patients have a fair chance to attain optimal cardiovascular health.
References
- Whitehead M, Dahlgren Gr, Organization WH. Levelling up (part 1): a discussion paper on concepts and principles for tackling social inequities in health. 2006.
- American Nurses Association. Code of Ethics for Nurses with Interpretive Statements.
- Van Dyke M, Greer S, Odom E, et al. Heart Disease Death Rates Among Blacks and Whites Aged >/=35 Years – United States, 1968-2015. MMWR Surveill Summ. Mar 30 2018;67(5):1-11. doi:10.15585/mmwr.ss6705a1
- Virani SS, Alonso A, Aparicio HJ, et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. Feb 23 2021;143(8):e254-e743. doi:10.1161/CIR.0000000000000950
- Petersen EE, Davis NL, Goodman D, et al. Racial/Ethnic Disparities in Pregnancy-Related Deaths – United States, 2007-2016. MMWR Morb Mortal Wkly Rep. Sep 6 2019;68(35):762-765. doi:10.15585/mmwr.mm6835a3
- Ferranti EP, Jones EJ, Bush S, et al. A Call to Action: Cardiovascular-Related Maternal Mortality: Inequities in Black, Indigenous, and Persons of Color. Journal of Cardiovascular Nursing. 2021;36(4):310-311.
- Churchwell K, Elkind Mitchell SV, Benjamin Regina M, et al. Call to Action: Structural Racism as a Fundamental Driver of Health Disparities: A Presidential Advisory From the American Heart Association. Circulation. 2020/12/15 2020;142(24):e454-e468. doi:10.1161/CIR.0000000000000936
- National Academies of Sciences E, and Medicine,. In: Flaubert JL, Le Menestrel S, Williams DR, Wakefield MK, eds. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. 2021.
- Havranek EP, Mujahid MS, Barr DA, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. Sep 1 2015;132(9):873-98. doi:10.1161/CIR.0000000000000228
- Kunin CM, Douthitt S, Dancing J, Anderson J, Moeschberger M. The association between the use of urinary catheters and morbidity and mortality among elderly patients in nursing homes. Am J Epidemiol. Feb 1 1992;135(3):291-301. doi:10.1093/oxfordjournals.aje.a116283
- Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. Aug 26 1993;329(9):621-7. doi:10.1056/NEJM199308263290907
- Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. J Cardiovasc Nurs. Jul-Aug 2007;22(4):326-43. doi:10.1097/01.JCN.0000278963.28619.4a
- National Academies of Sciences E, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation’s Health, . Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. 2019.
- Centers NAoCH. Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE). National Association of Community Health Centers; 2016.
- Tolbert J, Orgera K, Singer N, Damico A. Key facts about the uninsured population. Kaiser Family Foundation. 2019. 2020.
- Cole MB, Kim J-H, Levengood TW, Trivedi AN. Association of Medicaid Expansion With 5-Year Changes in Hypertension and Diabetes Outcomes at Federally Qualified Health Centers. American Medical Association; 2021:e212375-e212375.
- Khatana SAM, Bhatla A, Nathan AS, et al. Association of Medicaid Expansion With Cardiovascular Mortality. JAMA Cardiol. Jul 1 2019;4(7):671-679. doi:10.1001/jamacardio.2019.1651
