Addressing hypertension at the local and global levels requires using validated tools, following the data, and working with patients and policymakers alike. Guest Yvonne Commodore-Mensah, PhD, MHS, RN, FAAN, FAHA, FPCNA describes strategies for clinical practice as well as legislative advocacy for addressing this global healthcare crisis.
Episode Resources
- Validated blood pressure monitors: validatebp.org
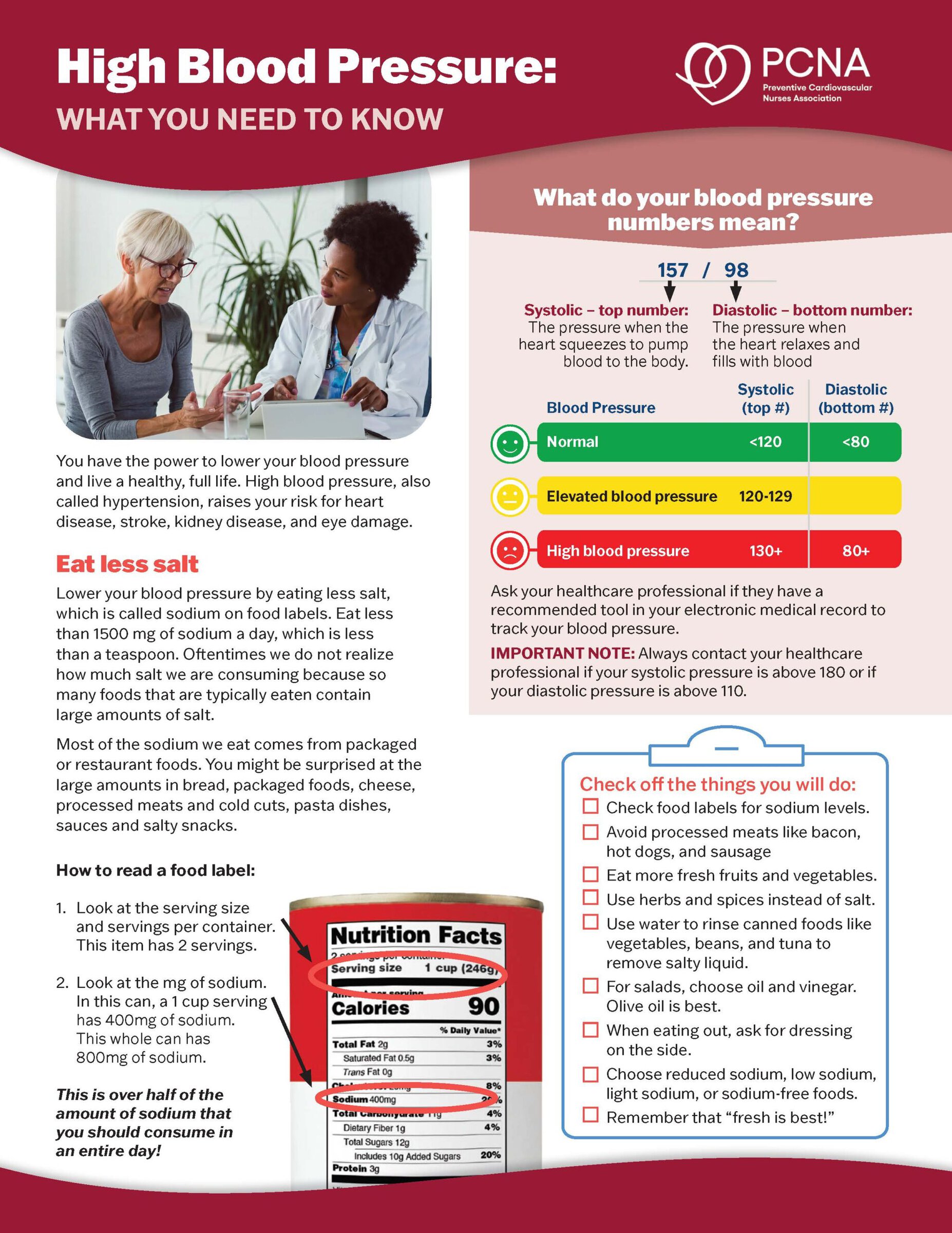
- PCNA patient education blood pressure resources
- High Blood Pressure: What you need to know (sheet in English & Spanish)
- Blood Pressure: How do you measure up? (Booklet in English & Spanish)
Yvonne Commodore Mensah 2025 podcast episode transcript
[00:00:00] I’m Erin Ferranti, board president for PCNA, and I’d like to welcome you to this episode of the Heart to Heart Nurses Podcast. PCNA is the proud home of cardiovascular nurses and one of the leading figures in the fight against cardiovascular disease. We have the resources you need for your day-to-day practice or to follow your passion to new areas of learning and growth.
Geralyn Warfield (host): I’d like to welcome our audience today to our conversation with Yvonne Commodore-Mensah, and we’re going to be talking about hypertension. Yvonne, before we get started, could you introduce yourself?
Yvonne Commodore Mensah (guest): (00:28) Hi, I’m Yvonne Commodore-Mensah. I’m a professor at the Johns Hopkins School of Nursing and the Johns Hopkins Bloomberg School of Public Health. I’m also honored to be a board member of PCNA.
Geralyn Warfield (host): Well, we are so excited that you’re here to share your time and your expertise with us. And I know that we have probably discussed hypertension previously, and it’s not a problem that seems to be going away, is it?
Yvonne Commodore Mensah (guest): (00:54) Unfortunately not. We know that far too many people in the US and globally have hypertension. For instance, in the US, 1 in 2 adults has a diagnosis of hypertension. But unfortunately, only 1 in 5 adults has their blood pressure controlled to less than 130/80. And this is despite the availability of blood pressure lowering medications that work.
Also, interventions that we know help to achieve blood pressure control, including the use of treatment algorithms, the use of team-based care—meaning how do we engage multidisciplinary teams to work collaboratively to support patients and address their social needs—also address issues surrounding their diet, how to improve their diet to improve blood pressure control, and also measuring their blood pressure at home. That’s one of the proven ways to improve blood pressure control. Some call it home blood pressure monitoring. That’s also effective, but unfortunately, that’s another strategy that’s not adequately implemented.
But we also know that this is a global issue as well.
Unfortunately, 90% of people with uncontrolled blood pressure in low- and middle-income countries also don’t have their blood pressure controlled. So apart from being a local issue, it’s also a global health challenge.
Geralyn Warfield (host): (02:34) I think one of the reasons that this and other cardiovascular diseases are such an issue is that it’s not obvious. You know, if you were to have a skin condition, for example, it’s pretty obvious that that’s an issue. But hypertension is this unseen, unthought about kind of disease. So, what kinds of strategies might clinicians or people working in health care offer or put into practice to help their patients understand how important it is to keep this under control and to be tested regularly?
Yvonne Commodore Mensah (guest): (03:04) I’m so glad you mentioned that. Unfortunately, hypertension is one of those conditions, and many of us say, it’s not sexy (for lack of a better term). People just don’t find the issue of blood pressure control as exciting, and we know that hypertension is a major risk factor for cardiovascular disease and stroke.
There are therapies that work, but unfortunately health systems, for instance, are not prioritizing, ‘How do we examine our data internally to see where we are in terms of blood pressure control? How do we also invest in resources such as perhaps hiring community health workers internally to support patients who don’t have controlled blood pressure?’
For clinicians, we have this term that we call clinical inertia. Unfortunately, when a patient shows up, you measure their blood pressure, their blood pressure is uncontrolled, and they admit to taking their medications as prescribed. Unfortunately, clinicians may be overly optimistic that perhaps, well, maybe the blood pressure’s normal at home, maybe they were anxious, so we make a lot of excuses, unfortunately, and don’t take action.
And with blood pressure control, measuring blood pressure accurately is one of the steps.
The second is acting rapidly when blood pressure control is not achieved. The reality is that there are a lot of patients who go months, if not years, without achieving blood pressure control.
And the last piece is partnering with patients. So, we need to teach clinicians how to better partner with patients, how to engage in what we call shared decision-making to really understand how effective the therapies that are prescribed are. And if they are not effective, how can changes be made? How might clinicians assess and address medication adherence and also barriers to care?
So unfortunately, we know what works, but there’s really a gap in terms of taking the rich evidence base when it comes to blood pressure control and also applying it to our practice on a day-to-day basis. And that’s where implementation science comes in.
We know that it’s a field that is really laser focused on bridging the know-do gap. We know what to do, but we don’t do it. So how do we bridge that gap using implementation science? And I would say nurses, cardiac nurses, are well positioned to really implement all of these strategies into practice and into usual care.
So, if home blood pressure monitoring works, how do you create a protocol for ensuring that patients who are diagnosed with hypertension who don’t have blood pressure control have access to validated blood pressure devices?
But also, how do you close that loop? It’s one thing to measure the blood pressure at home, and it’s another thing for that information to be looped back to the clinician and the healthcare team so that that information can be used to improve blood pressure.
Geralyn Warfield (host): (06:30) And it’s just like anything. Let’s say, for example, your patient comes to you, they have their monitor with them, or they have their data with them. And then for some reason, during the course of the clinical visit, they forget to offer it to the clinician, or the clinician forgets to ask. And then they go home and they’re like, “Well, nobody looked at this. Why is this important?” So, it’s very easy for them to fall off that wagon, if you will.
And so, trying to get them motivated to do it again the next time is even harder. So, it’s important to have that shared decision-making and to help increase their understanding of why it’s important. But also, as you said, closing that loop and making sure that we do what we’ve asked them to do as well, which is to monitor that. So, thanks for sharing that.
How can nurses get involved in terms of a policy issue when it comes to hypertension?
Yvonne Commodore Mensah (guest): (07:16) That’s another area that I’m really excited about because I think there’s an opportunity to mobilize the four million nurses apart from cardiovascular nurses, just the overall nursing profession.
Because we see the downstream impact of not implementing or developing policies that improve the built environment in people’s neighborhoods, we have patients who have uncontrolled hypertension and don’t have access to healthy foods. And so, when they show up and we’re counseling them about, you know, food is medicine, exercise is medicine, but they live in neighborhoods that are unsafe, right? They live in communities where they don’t have access to healthy foods. We see the downstream impact. We see rates of uncontrolled hypertension. We see the complications of blood pressure control that is not achieved.
And so, that’s an opportunity for us to also be present in the conversations that address developing policies to improve access to healthy foods, access to tools and resources.
I’ll share an example. I had the opportunity to participate in a maternal health equity summit. We had a senator from Maryland who was at one of the sessions where we talked about one of our programs, the Safe Heart Women’s Study, which is funded by the American Heart Association. And the goal of that project is to really increase women’s awareness of heart disease.
But we also went into communities and checked their blood pressure. We checked their cholesterol, their blood sugar levels, and communicated their risk for cardiovascular disease. And so, he came up to us and asked, “So what policies can be developed locally to improve blood pressure control, but also prevent complications during pregnancy?”
And so, we touted the benefits of home blood pressure monitoring, but also support from community health workers. And believe it or not, he took that information and met with his policy advisor, and they drafted a bill and came back to us, asked us to review and provide input. And this bill, as we speak, is going through the process in the Maryland Senate and House side to really be able to make sure that for Medicaid patients who are pregnant or have chronic disease risk factors, that they have access to validated blood pressure devices in order to prevent and control hypertension.
It was really mind-blowing to see that a simple conversation that was had rapidly evolved into the development of a bill that is now going through the process.
And we hope—and this is something that I had the opportunity to partner with community members, but also one of our recent doctoral students who graduated, Dr. Faith Metlock was involved in it. And so, to be able to see the impact, and this is not talking about 10 years down the line or 15 years down the line. We were actively recruiting when we had this conversation with him.
So that’s an example of how nurses, cardiovascular nurses, who have so much rich knowledge of evidence-based practice, how we can engage with our policymakers locally and convey to them what they can do, take the knowledge and translate it into policies that make a difference.
Geralyn Warfield (host): (11:10) That’s a really inspiring story. I’m so appreciative for you for sharing that with our audience.
We are going to take a quick break, and we will be right back.
Geralyn Warfield (host): Welcome back, where we’re talking with Yvonne Commodore Mensah about hypertension management. and there are a lot of different ways that that happens. And, any more, there’s also some ways that we can happen—how this can happen—more readily and more easily with technology. Could you talk a little bit about the intersection of hypertension and technology for us?
Yvonne Commodore Mensah (guest): (11:38) Absolutely. So, we know that one of the challenges to improving blood pressure control is the fact that we have a limited health workforce. There aren’t enough primary care providers to manage the burden of hypertension for our audience? There are over 122 million people in the U.S. who have hypertension. So, we need more health care professionals to work together collaboratively to improve blood pressure control.
But we also know that we need to use tools that exist to improve blood pressure control. One of the tools I would say would be validated blood pressure devices for home blood pressure monitoring.
I would say that for every patient who’s diagnosed with hypertension, they shouldn’t have to wait three months to have their blood pressure measured by a primary care clinician. We need to support them, work with your insurance, to get access to validated blood pressure devices. And I also stress validated because there are a lot of devices—and I see it as a tool, right, that exists. But we need to make sure that our patients are using the right validated tools to achieve blood pressure control.
So validatebp.org is one of the resources. It’s a website that was designed by the American Medical Association that has a list of devices that have been validated, and it has devices that are considered home blood pressure monitoring devices.
There are also what we call clinic blood pressure monitoring devices, but they also have a list of kiosks. So, we know that a lot of community pharmacies may have blood pressure kiosks that people use to measure their blood pressure, but unfortunately not all of them are considered validated. So that resource has a listing of devices that are considered validated and in terms of accuracy, there’s greater confidence in accuracy.
Another tool I would also mention is artificial intelligence. I know in this day and age, there’s a lot of excitement. There’s a lot of potential. But this does not replace the importance of making sure that we’re engaging clinicians, especially nurses, that we have these meaningful conversations with our patients. But I’m excited about the promise of artificial intelligence to also help reduce the workload for nurses so that we can spend more time talking about what gets in the way of controlling your blood pressure, right?
Documentation is one of the biggest challenges. There are tools available, as we speak, that clinicians can use to take notes, that will transcribe the notes, highlight areas that need to be addressed. How can nurses be involved in those processes so that we can also benefit and use these tools to improve efficiency and productivity?
But also, I’m excited about how AI can be used to risk stratify. So, what does that mean? So, we know that there are subpopulations who are disproportionately affected by hypertension. And artificial intelligence has this amazing capability to digest a vast amount of information from different sources. So how do we leverage all of those data sources to identify higher risk groups, individuals who may have other comorbidities that may play some of the higher risk for cardiovascular disease?
How do you also integrate data, individual level data? How do you also then pull in neighborhood level data? So, for instance, with one zip code, you can actually predict the types of resources that are available. There are different indicators. One of them is, for instance, the social deprivation index, right?
So, if someone resides in a neighborhood that has a higher social deprivation index, you have to acknowledge or understand that this is someone who may have greater challenges, right? So how do we use those data to refer them to social services or engage a community health worker to support them to address these social needs, right?
So, that’s another promise of artificial intelligence. But also, the last piece would be we can leverage artificial intelligence to prompt clinicians when blood pressure control is not achieved. There are clinical decision support tools.
Many clinicians don’t like them because there a lot of buttons, a lot of steps, but how can we use this powerful tool to really distill and digest all of the different amounts of information and rank and prioritize what are the top three needs? What are the top three issues that you need to address to improve blood pressure control?
And if a clinician doesn’t take action, how can we use this to send gentle nudges, right? But how can health systems use that information to understand how providers are doing and keep them accountable, right? Because if we don’t act rapidly to control hypertension, the health system is impacted, but as a society, we pay for the downstream consequences, such as heart attacks, strokes, and kidney disease as well.
Geralyn Warfield (host): (17:32) I think the other component of this, that we’re going to lead to next, is patient empowerment.
For example, if a patient understands how an accurate blood pressure is being taken at home, if it’s not happening that way in the clinic because of time, efforts, or whatever the case might be, they could advocate for, “You know, I just sat down, can we wait a minute before we take my blood pressure?” or, “I really have to go to the restroom, can I do that before we take my blood pressure?” so that there’s more accurate readings both at home and in the clinic setting.
Are there other resources that you could think of that might help patients or clinicians in this process? You outlined those artificial intelligence and technology issues beautifully, but is there anything else that we could offer to our audience?
Yvonne Commodore Mensah (guest): (18:14) Well, I’ll say as a board member of PCNA that our organization has done a tremendous job of really mobilizing clinicians to develop clinical resources, patient-facing resources that are evidence-based, right? So, if you go to our website, PCNA.net, and you go to clinician resources, you’ll find a number of patient education tools that you can use to talk about hypertension, the causes, how to manage hypertension, and also other patient-facing tools that you can distribute if you were to be invited to engage in a community health fair.
I know that a lot of communities, especially during Heart Month, look up to cardiovascular nurses and clinicians to come and speak at community events about heart health. Please check out those resources. Don’t reinvent the wheel and create resources. All these tools are available. How do we disseminate them?
And I also love that these resources are available in English and Spanish. And there a lot of resources online as well that may have multiple languages, right? So how do we leverage all of these tools to really empower our communities to make hypertension control a priority.
Geralyn Warfield (host): (19:42) Thank you so very much for that very comprehensive view of hypertension and the importance of the control, and the resources that we can use.
I have one final question for you and that is, what one key takeaway would you like our audience to walk away with?
Yvonne Commodore Mensah (guest): (19:58) That would be that small steps make a big difference. Small steps in the sense of physical activity, right? Some amount of physical activity is better than no physical activity. When it comes to diet, picking one thing. If it’s eliminating some processed foods that are higher in sodium, if that is the one thing you can do, that makes a difference.
So, find that one thing that you know you can do and do well, and that may inspire you to do even more to control hypertension.
Geralyn Warfield (host): (20:36) Yvonne, thank you so very much for being here today. We are so grateful to you for your expertise and for sharing that information.
Yvonne Commodore Mensah (guest): (20:43) Thank you so much for having me.
Geralyn Warfield (host): (20:45) This is Geralyn Warfield, your host, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. Visit PCNA.net for clinical resources, continuing education, and much more.
Topics
- Hypertension
Published on
June 3, 2025
Listen on:

PhD, MHS, RN, FAAN, FAHA, FPCNA
Related Resources