One in two U.S. adults has an elevated blood pressure, and for those that have hypertension, only one in four have it controlled. Guest Janet Wright, MD, FACC, describes the critical role nurses play in detection and management, strategies, and resources to help healthcare professionals and patients partner on accurate blood pressure monitoring.
Episode Resources
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to today’s episode where we are very enthusiastically welcoming Dr. Janet Wright. Janet, could you please introduce yourself to us?
Janet Wright (guest): Yes, Geralyn, it’s a pleasure to join you today. I’m Janet Wright. I’m the Director of the Division for Heart Disease and Stroke Prevention at the Centers for Disease Control and Prevention.
Geralyn Warfield (host): Well, we have a very specific thing to discuss today, and that is hypertension. And I’m hoping you could discuss for us just a little bit about the current state, and the trends, in hypertension detection and control.
Janet Wright (guest): Yes, Geralyn, and I’m, I will tell you, I come with a warning label. I’m rabid about hypertension detection and control, and the reason [00:01:00] I’m rabid is that it affects one in two adults in the United States. One in two of us over the age of 18 has an elevated blood pressure.
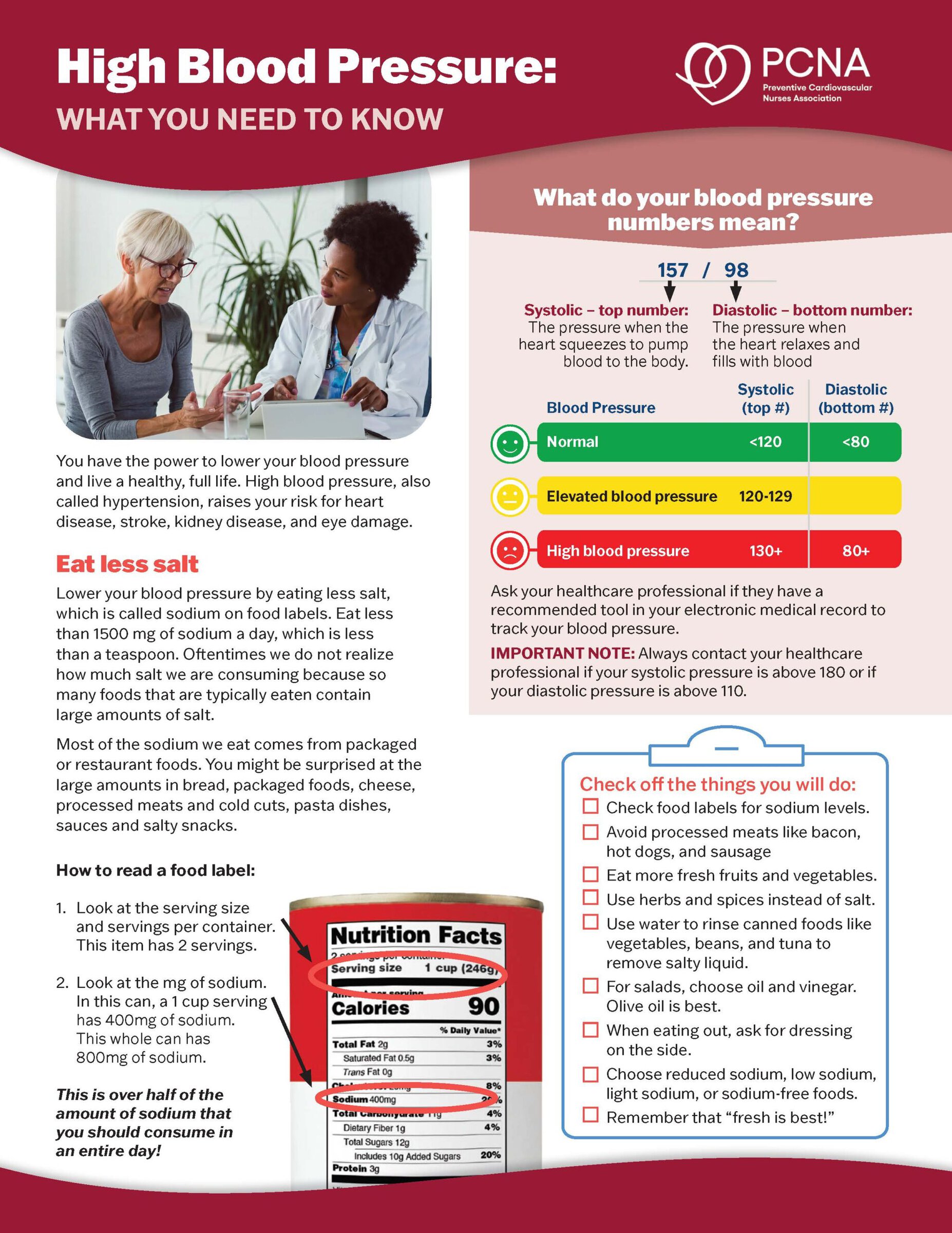
And that elevation, diagnosis, or definition of hypertension, by most guidelines, is a blood pressure that’s over 130 on the top and over 80 on the bottom. There are some guidelines that say it’s over 140 and over 90. We won’t quibble about that. We all know that lower is better, as long as that’s okay for the individual person.
And the trends are not good. For a number of decades, we’ve seen a rise in the blood pressure control rate, but over the last five to eight years, we’ve seen a slippage in that control rate.
Another thing that’s important to keep in mind is, we have, for years, used a standard of office measurement of blood pressure to diagnose hypertension. And what we’ve [00:02:00] learned from numerous studies, randomized control trials, and meta-analyses and systematic reviews, is that the most accurate way to diagnose hypertension is through home monitoring.
And so, when, when I say that one in two of us has hypertension, it’s probably an underestimate.
We know that of those people—120 million of us with high blood pressure—only one in four of us has that blood pressure under control. So, think about that. That’s three out of four people with high blood pressure out of control. This in a situation where we really do know how to control hypertension, it’s just not happening everywhere for everyone.
Geralyn Warfield (host): Do you think one of the reasons it’s not diagnosed as frequently is that it is an unseen, unfelt type of disease state that people don’t recognize? Obviously if you injure yourself, if you fall [00:03:00] off a bike, for example, it’s an obvious injury. But this is an example of a disease state where it’s not quite so obvious.
Janet Wright (guest): You make an excellent point. And as you know, hypertension is often called a silent killer because with each beat of the heart, that elevated pressure is hammering the walls of the artery, and the arteries. And those are the arteries in the brain, in the kidney, during pregnancy.
And so, we know that those uncontrolled pressures, over time, if we think about a life course approach, with each beat of the heart that uncontrolled pressure is doing extraordinary harm throughout all the organs in the body.
One reason is, high blood pressure typically does not cause a person to feel differently.
A second reason is, we’re dealing with a very dynamic situation. All of us who have practiced, taken care of people, know that blood pressure, [00:04:00] if repeated, often changes. It may go up a little bit or go down a little bit. But in the busy flux of an office, it’s not always possible to take multiple pressures.
And really, the important thing is an individual is not in their normal environment when they’re in an office setting, a clinical setting.
And so, again, evidence has shown that in order to get a really good read on someone’s blood pressure, we need to look at a pattern of readings. Ideally taken over several weeks’ time. Once in the morning, once, twice in the morning, once in the afternoon, to, to find out if the pressures in the office are reflective of that person’s real blood pressure.
Geralyn Warfield (host): And I know there’s been a lot of discussion about how to effectively take a blood pressure reading. And so, I suspect both in the clinical setting and at home, that you might see some diversity in those readings, just based on whether or not someone has been, for example, you [00:05:00] know, taking their bike, maybe they rode their bike to your office and now they’re immediately in the exam room and they’ve got an elevated pressure, or perhaps we don’t have their arm resting in the right position. Would you say that that’s adding to some of the complexity of this?
Janet Wright (guest): Absolutely. You know, we’ve learned from places that are high performers in blood pressure control, that technique, technique, technique—it’s important to have. Have it posted on the walls, and also to make sure that individuals, patients who are coming in, know what the proper technique is. So: both feet flat on the floor, sitting in a chair that has a back on it, having the arm at heart level and resting on something, not hanging loose, not talking, and ideally having rested for about five minutes before taking the readings. And that should be augmented with readings from home. [00:06:00]
Geralyn Warfield (host): I have noticed when I have gone to the provider’s office over the last five to 10 years, there really is an unequal application of those very important standards that you’ve just described. So, even when I’m a patient in another clinician’s room, I’m very aware of what I am supposed to be doing. So, I uncross my legs, I put my arm out. I’m trying not to talk—even though when you go to the provider, there’s a lot of questions to ask. And so, there are, there are a lot of things going on, so I appreciate that sometimes we don’t even recognize that we haven’t used the proper technique.
Janet Wright (guest): Yes, you remind me of a story from, again, a high performer, someone who was a Million Hearts champion and achieved 80% blood pressure control for the entire population they were being, that were, they were caring for. Said it, it felt a little bit like what they say about the Golden Gate Bridge, that when painters are finished with it, they just turn around and start over and go back the other way. And that was the training that’s necessary to preserve [00:07:00] fidelity to those good blood pressure techniques.
But, you know, Geralyn, the cascade of events that occurs, if a clinician does not trust the reading, those, that cascade has a profound impact. So, if you don’t believe that the reading you saw on the chart is an accurate reflection, you are hesitant to change your treatment or to counsel about lifestyle because you don’t trust the reading. And so, we found over time that having that pattern, seeing the rise and fall, making sure that you’re not dealing with either masked or white coat hypertension,the confidence you can, that comes from the patterns of home readings, allow you to proceed with treatment. Or to make you feel confident, the person doesn’t need medication, which is also fabulous.
So, it’s about making sure that accurate, pristine technique [00:08:00] leads to accurate diagnosis.
Geralyn Warfield (host): We are going to take a quick break and we will be right back.
Geralyn Warfield (host): We’re back with Janet Wright, talking about hypertension. And we’ve discussed a little bit about taking an accurate reading, that it is a disease that affects far more people than many of us realize. And I’d like to turn more towards an action item. And what kind of role do clinicians, including PCNA members, have in addressing this issue?
Janet Wright (guest): You know, Geralyn, the, the roles are many. And I think one of the most important things, the most important thing that I think is missing right now, is to convey to an individual the importance of blood pressure control in the crush of a busy office appointment with limited time. And, and usually a reason on that, that patient has come into the office and that is you, you have an imperative to [00:09:00] address that issue.
It is so easy for hypertension to slip into the background For it to become background noise. And nurses in particular can keep that from happening. Because nurses are so trusted, and deserve that trust, they’re even bringing up an elevated pressure as a note of concern, and expressing that concern to a patient, can make the difference.
Because I, I know it’s true for, I think it’s probably true for you, it’s certainly true for me, that multiple times people have told me, “My pressure is elevated. Nobody said anything.” Or, “Nobody even told me it was elevated. They took my pressure and then went down the hall and I never knew what it was.” And so, by using their expertise and their voices to express the importance of hypertension control, will go a long way.
Geralyn Warfield (host): So, there is a lot for us to learn about hypertension, it’s [00:10:00] application for measurement, and management in practice. And I’m hoping you could point us towards some resources to help us learn a little bit more.
Janet Wright (guest): Yes. Well, the first place I would point you is to your home. PCNA has fantastic resources, human and otherwise, all available online through your membership. And so, I would say the first shop at home.
There are additional resources and the good news about hypertension control and I, I honestly feel like I sense, around the country, an authentic commitment to, and investment in, equitable hypertension control. So, organizations like the American Heart Association, American Medical Association.
Certainly, at CDC we have Million Hearts that’s been in hypertension control since its inception in 2012.
And then CDC itself. [00:11:00] We are seeing huge amount of collaboration across the Department of Health and Human Services, through 12 agencies all deeply invested in equitable detection and control. As well as the lifestyle and community-based improvements that can help people get healthy, and stay healthy, and maybe need less medication. So, those are a few.
I, I would actually call out a couple of things for your membership. And one is something called a Hypertension Control Change Package. It is a product of the Quality Improvement Team at CDC and in Million Hearts, and it is a collection of tools and resources that have been used in practices around the country. And we have gleaned them, harvest them through generosity, and organize them in a way that if someone wants to take on a [00:12:00] quality improvement project, they can pick and choose which element is the best fit for their setting and for the population that they serve.
The other resource I would call out is a campaign sponsored by a number of companies in cooperation with Million Hearts, CDC, and the CDC Foundation. It’s called Live to the Beat. It is a campaign directed by and actually informed by, shaped by, Black and African American individuals to help them from wherever they are in their lives, start to take a healthier pathway. All the resources are available on our website and, obviously, at no cost, but there are lots of engaging type activities.
And we know that African Americans suffer a very much higher rate of hypertension, a lower rate of control, and they also [00:13:00] develop hypertension at earlier ages, resulting in a whole slew of largely preventable health outcomes. So, Live to the Beat, Hypertension Control Change Package are two that I would highlight.
Geralyn Warfield (host): We will definitely put the links to those resources in our show notes so that you have access to those. Is there anything else that you’d like to add that we have neglected to discuss thus far?
Janet Wright (guest): You know, I, I appreciate that chance, because one thing that we know, we know, we know a couple things about nurses, sort of writ large. One is this trust aspect—the most trusted health professional. And at a time where misinformation reigns supreme, never ever was your role and your status as a trusted source more valuable.
The other thing that used to be true, is that nurses as a group are not the healthiest of [00:14:00] health professionals. And given how critical you are to health and healthcare, I would ask each nurse listening to make sure that he or she knows your blood pressure, and that you are monitoring it if it’s elevated, and taking steps to control it. Because we need you for the long term.
Geralyn Warfield (host): We have had such a great conversation with Dr. Janet Wright today. Thank you so very much for joining us. This is your host, Geralyn Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Hypertension
Published on
November 7, 2023
Listen on:
MD, FACC
Related Resources