Often prescribed for obesity, SGLT2is and GLP-1 RAs have a role in heart failure management. Learn about their mechanisms of action, and how their use extends beyond weight loss to cardioprotective and renal protective properties. Join us with guests Kim Newlin, MSN, ANP, FPCNA, of Sutter Roseville Medical Center in Northern California, and Colleen McIlvennan, PhD, DNP, ANP, FAHA, FHFSA, from the University of Colorado in Denver.
You can earn 0.5 contact hours and .05 pharmacology hours from listening to this podcast episode and completing the course components.
This podcast is supported by independent educational grants from Merck Sharpe and Dohme Co and the Pfizer-Merck Alliance.
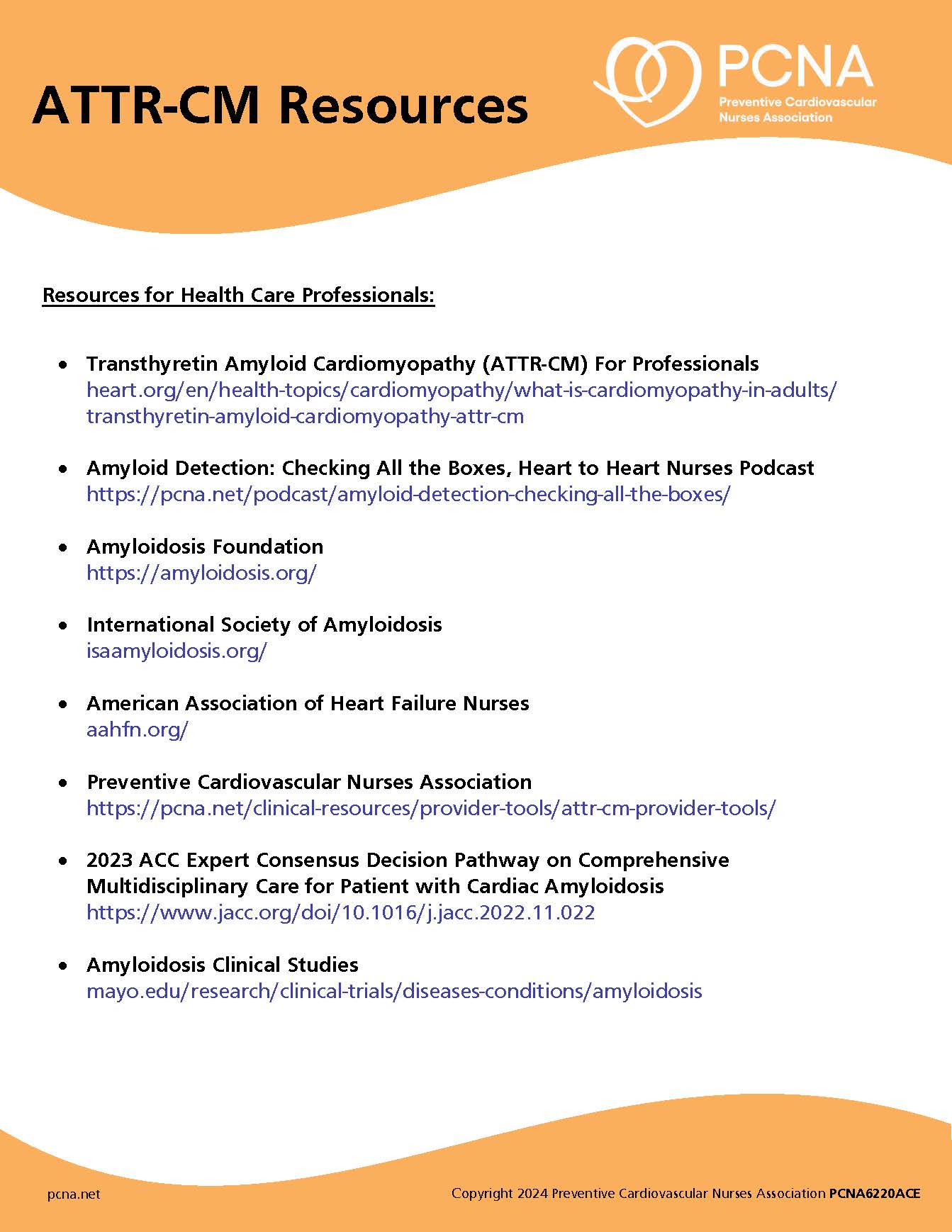
Episode Resources
- 2022 AHA/ACC/HFSA 2022 Guideline for the Management of Heart Failure
- Pocket Guide: Guidelines for Managing CVD Risk in Patients with Diabetes
- Heart Failure Pocket Guide: A Guide to Prevention and Management
- CE course: New and Emerging Treatments for Heart Failure: HFrEF and HFpEF
- SGLT2is in Heart Failure
- SGLT2i in HFpEF: multicenter randomized trial
- Empagliflozin in HFpEF
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): We’d like to welcome our listeners to today’s episode, where we will be discussing the mechanisms of action for SGLT2 inhibitors and GLP-1 RAs. I am your host, Geralyn Warfield.
This particular episode is available for CE contact hours. Please make sure to follow the link in the episode show notes to complete the post-test and access your CE certificate.
Today. I’m really grateful to our guests, Kim Newlin and Colleen McIlvennan. Kim, could you introduce yourself and then we’ll have Colleen do the same?
Kim Newlin (guest): Absolutely. Well, first of all, thank you for having both of us. I always enjoy [00:01:00] doing these podcasts and I always find it, it helps me make sure that I’m on top of my game for this information.
So, I’m glad to be here with Colleen. My name, again, is Kim Newlin. I’m an Adult Nurse Practitioner and a cardiovascular Clinical Nurse Specialist, as well as a Director of Nursing at Sutter Roseville Medical Center in Northern California. So, here I have oversight of our cardiac rehab program. I also see high-risk patients after they’ve been discharged from our hospital with either a diagnosis of heart failure or an acute MI, and just help with managing that transition: getting them set up with the right outpatient resources and also answering a lot of questions about all the new medications they’re often put on when they’re hospitalized.
Colleen McIlvennan (guest): Great. Thanks, Geralyn for the introduction, and it’s great to be here with Kim, as always. Thanks for having me. I’m Colleen McIlvennan. I am an Adult Nurse Practitioner and researcher at the University of [00:02:00] Colorado in Denver. I also serve as the section head for advanced practice providers in the entire division of cardiology.
My clinical work is primarily on the inpatient advanced heart failure and transplantation service, and then my research really dovetails nicely with that in focusing on patients and caregiver engagement around treatment options for heart failure.
Geralyn Warfield (host): I am sure that our audience can tell that we have some experts, not just with heart failure, but so many other things, with us today. And so, let’s get started talking a little bit about the two drug classes where we’re going to focus: SGLT2 inhibitors and GLP-1 receptor agonists. So, they’ve been used with patients with type 2 diabetes to treat hyperglycemia, but I’m hoping that the two of you can talk a little bit about the methods of action for these two pharmacotherapies. Colleen, could you start?
Colleen McIlvennan (guest): Yeah. Starting off with the patho, patho [00:03:00] conversation. GLP-1 receptor agonists really work by activating the GLP-1 receptors that are located in the pancreas. This can lead to enhanced insulin release and reduced glucagon release—responses that are both glucose-dependent. And the, the GLP-1 receptor agonists really do have a low risk of hypoglycemia.
Kim Newlin (guest): And as Colleen mentioned, you know, we’re starting off with the sexy stuff here Glucose Cotransporter-2, or SGLT2 inhibitors, function a little bit differently. So, they actually reduce the glucose reabsorption in the renal tubule, so in the kidneys. And, therefore, what they lead to is a reduction in blood glucose, but without actually stimulating an insulin release. So, like Colleen mentioned with the GLP-1s, is that there [00:04:00] is also a, a fairly low risk for hypoglycemia.
There are some off-target effects, too, that have been proposed, and so there’s some thoughts—and we’ll get into this a little bit, when we talk about why these medications may be used for other things besides diabetes, but it, it looks like these SGLT2 inhibitors also may have an effect on the sodium hydrogen exchangers in both, or in all of them: the heart, the kidney, and inflammatory cells, which may influence major adverse cardiovascular events, heart failure, and kidney outcomes.
Also, some thoughts that maybe the—and the research is continuing on with these medications to better understand them—but they also may have effects on the sodium, calcium, and potassium channels in the myocardium. So again, they may have some impact on just heart function, myocardial function, and rhythm stability. that are just independent of [00:05:00] just that sodium glucose code transporter inhibitor function.
Colleen McIlvennan (guest): Yeah. Thanks, Kim. I, I think just to second what has been said, it’s just, I, I think it’s so interesting, especially when we talk about, specifically SGLT2 inhibitors and how they originally developed as diabetes medications, and now really, still, trying to fully understand their mechanisms and the benefits they have outside of glucose-lowering.
Kim Newlin (guest): Yeah. So, we’ll have to follow up with another podcast.
Geralyn Warfield (host): So, for our listeners who are super-excited about physiology, biochemistry and everything that they thought this podcast was going to be about, we’re going to actually shift gears just a little bit and talk about the importance of this information for cardiovascular nurses and other cardiovascular professionals.
It used to be that these kinds of drugs were used specifically in the management of [00:06:00] diabetes, which wasn’t necessarily under the umbrella of what a cardiology clinic or folks working in cardiology were doing, but they would, at that point, perhaps have referred to an endocrinology kind of practice or somebody who is focused on the diabetes. But we’re finding out that they actually have applications in cardiovascular and primary care clinic settings. Kim, could you expound a little bit more about that and why our listeners might be interested in this?
Kim Newlin (guest): Yeah. Yeah, absolutely. And I think for those of us who’ve been in the cardiology space, you know, maybe for a short or even a long time, I think we’ve all been developing those skills of explaining why patients are on certain medications, right? We’ve all had that, “Well, why am I on a statin if my cholesterol’s not high?” or “Why have I, am I on a beta blocker if my blood pressure is not high?” Right? So, we’ve, we’ve kind of developed that skill in explaining why something may be not necessarily what it looks like it’s indicated for, or when [00:07:00] they get their medication, what it may default to saying it’s for.
But you know, this is, this is definitely a space where, where these medications will continue to be used for, for a number of things within both, maybe the cardiovascular, as well as the, the renal space. And I think as we continue to see a rise in diabetes, unfortunately, we just know that there’s, there’s not enough endocrinologists to see everybody. So, all of us, all clinicians really, need to be comfortable working with patients who have diabetes or, and/or managing insulin, but also with patients who are, you know, maybe benefit from these other medications that we consider, not really off-label, but we’re just, you know, we’re so thinking that these are diabetes medications.
And there continues to be mounting evidence that the use of these medications have multiple benefits for our patients. And, you know, [00:08:00] part, part of the challenge is we in, in heart failure, who’ve been in it long enough, know that for many years, there were no changes in the guidelines for heart failure. And now we have all these new medications. Plus, we have, you know, the SGLT2s and the GLP-1s which have multiple indications. So, I think we’re all still trying to, to adapt to heart failure being a moving target, which I think we, we got used to it not being that way. So, it’s a good thing though.
So, to just expand on it a little bit, we’ve had, you know, lots of really good analysis of several randomized, double-blind placebo-controlled trials. Some of them, you know, have, have fun names—you know, EMPA-REG Outcome, EMPEROR-Preserved, CANVAS, DECLARE, CREDENCE—but, but what those studies really helped us look at is going back and, you know, looking at the data for those people we were trying to really control blood sugar, we actually saw that these medications decreased the risk of [00:09:00] hospitalizations for heart failure or of death from cardiovascular causes.
And also, we’re seeing the positive effect in patients with heart failure, with reduced ejection fraction, right? That class of patients with heart failure, who we really have felt our hands have been tied and haven’t seen medications really improve outcomes.
So again, this reduction in cardiovascular death and hospitalization was whether patients had diabetes or didn’t have diabetes. So that really came out in the EMPEROR-Preserved trial. So, also in addition to slowing progression of renal disease, and getting more information about that, which, which I think we’ll just continue to see more support for, these medications being used kind of across our cardiovascular spectrum.
Colleen McIlvennan (guest): Kim, I, I just—thanks for the very detailed overview. I, I think one thing I’d like to add is just how much I really think the introduction of [00:10:00] specifically, again, I’ll say SGLT2 inhibitors, in, as part of quadruple therapy for patients with EF less than 40%, I think it has strengthened our relationships and collaborations with endocrine, and co-managing patients who have type 2 diabetes. And I, I have found that to be really a great collaboration. Certainly, there’s, there’s been some territorial issues back and forth, but learning to work together to manage these patients who often do have these comorbid conditions, or are at risk of these comorbid conditions, has been really great going forward. And I think only is going to get better, as we, as we see the vast effects that these medications can have on patients.
Kim Newlin (guest): Yeah. Yeah. And I think, you know, we’ve, we’ve done and I’m sure you have the same situation in Colorado, but I [00:11:00] feel like the nephrologists are often my best friends, right? So, they’re, they, we’re working with them constantly on that, that balance for the kidney function. So, it is fun to, to develop that relationship with the endocrinologists. We just don’t have that many in this area. So, I wish there were more to collaborate with, but great point.
Geralyn Warfield (host): So, in addition to heart failure management being really a team sport, in terms of all the other professionals with whom we interact every day, there is some research that, some clinical data, that’s shown the cardio-productive aspects of the pharmacotherapies that we’re discussing today. And Colleen, I know you have some more information about how they are used in patients with cardiovascular disease.
Colleen McIlvennan (guest): Yeah, we have seen, really us looking at diabetes and heart failure, the intersection of these two conditions, really at every level. But we have been really focused on, in the past, of the atherosclerotic effects of, [00:12:00] of diabetes and then heart failure. So, as we talked about a little bit earlier in the podcast, these medications have been specifically looked at in diabetes, and the EMPA-REG trial was really the standout trial that unexpectedly demonstrated a 35% relative risk reduction in hospitalizations for patients with heart failure and type 2 diabetes.
These patients all had ASCVD as well. And now we have just seen multiple trials showing effects, as Kim outlined, renal function across LVEF range. And I think has, I don’t think we’ve seen really the pinnacle of, of what affects these drugs can have on patients. The GLP-1s, really the GLP-1 and SGLT2s are not created equal, but I think [00:13:00] we are going to see more and more trials looking at GLP-1s. They should be considered for patients with type 2 diabetes and additional cardiac risk factors, but really have not shown to be effective yet. And I think we need larger trials to look at this, in patients without diabetes.
So, they do aid in weight loss, which I know is a major factor in a lot of our patients and, and has been used for, specifically for weight loss for patients. But SGLT2s still are the preferred line, first-line for patients with heart failure and type 2 diabetes. But I think really an exciting time, it’s really, it’s really great to have medications that are well tolerated, really no dose titration, that, and minimal side effects, that we can offer to patients across LVEF [00:14:00] range for heart failure, with and without diabetes, with SGLT2 inhibitors.
Geralyn Warfield (host): We’ve been speaking with Colleen McIlvennan and Kim Newlin about the use of various pharmacotherapies in heart failure treatment. And we will be taking a quick break and be right back.
Geralyn Warfield (host): Welcome back to our listeners. My next question for our guests includes what their biggest challenges are for you in your practice related to the use of these pharmacotherapies, the SGLT2 inhibitors and the GLP-1 RAs, with your patients. And maybe Colleen, you could get us started.
Colleen McIlvennan (guest): Yeah. I, I think we have encountered challenges, in our practice specifically, I think number one is cost, which I think, many of the listeners and I’m sure Kim can relate. it wasn’t a matter of these medications being available, since they were already being used for type 2 diabetics, but it was the cost associated [00:15:00] with, with these medications and being recognized for heart failure treatment, not just type 2 diabetes.
The average cash price still remains around about $500 a month, which is cost prohibitive for, I think, almost everyone, but we are seeing more coverage across the board. And again, we see certain insurers prefer one SGLT2 inhibitor versus the other. And again, in GLP-1s, similar cost wise, but seeing more insurance companies recognizing them. For SGLT2s, I think we have the potential to see a generic as soon as 2025, but really no definitive pipeline yet for that. But it is, it remains a major issue for patients.
The, the second thing is actually talking to patients about taking an additional medication. [00:16:00] So, the average patient with heart failure is taking about seven medications. They often have comorbid conditions, such as AFib, requiring anticoagulation, CAD requiring statin and aspirin therapy, so we’re asking them to add yet another medication. But as mentioned earlier, it’s really well-tolerated, for the most part. It’s once a day. and it’s really no dose titration. So, I have found it, easier to, to talk to patients, when, when those check boxes are marked, but it does require a conversation as well as allowing patients to ask questions as to why, why we would recommend it.
We have instituted in our inpatient service, a cost consult, that is an order within our EMR, that triggers a review by a pharmacy technician that can give it us, give [00:17:00] us the price that the patient will pay out of pocket, for either a 30-, 60-, or 90-day supply. And so, we really initiate that cost consult before we prescribe either an SGLT2 or a GLP-1, so that we can talk about out-of-pocket costs with patients instead of them going to a pharmacy, and saying, “I can’t afford $150 a month. I’m not going to pick up this medication.” So, we actually have seen really great patient satisfaction. I think the providers have been satisfied as well, knowing what patients can afford, and what medications they actually can be on. And, we’ve been, we’ve been very successful in that initiative.
Kim Newlin (guest): Yeah. So, I think, you know, Colleen’s experience with the cost consult is, is fantastic. And I, we actually, I was just on a transition of care call, and we have been slowly implementing a transition of care pharmacy [00:18:00] program, and they were talking about copays and saving a patient about $600 in copays a month, just with managing medication.
So if, if you, as a listener are currently not leveraging your pharmacist on the inpatient side to help this process and help reduce sticker shock for those patients when they leave the hospital and go to the, the pharmacy and then see what their copays may, may cost, I, I really, you know, encourage you to explore that just because they are a great resource.
You know, and I think…you know, a lot of these people who come in, especially with a brand-new diagnosis, they, you know, often come in, maybe on an inhaler because someone’s been treating their shortness of breath and thinking they could treat it with an albuterol when it’s really actually heart failure.
And they may then go home on five or six new medications. So, for sure cost is, cost is one. you know, and if they’re [00:19:00] not on one of these medications already, trying to explain why another medication may, may be something that is actually really going to help them and, and explaining that data. So, some people just can’t even imagine taking another pill, right? They already feel like they they’ve replace a meal with their medications. You know, and something I, you know, Colleen’s experience on the inpatient side is, is amazing.
And I do, like I mentioned a couple of other places, so just want to talk a little bit about how we can support our patients, even if we’re not a prescriber. So, I think one is, if you are on the inpatient side and you don’t see these medications on your formulary, maybe there’s that conversation about making sure they’re available, because we know that if patients start the medications in the hospital, they’re more likely to take them. So really pushing to get, you know, kind of the, the four linebackers, or the, the four key, four key medications on for these patients, the quadruple therapy.
In the cardiac rehab [00:20:00] side, this is a great place for education about options. Or if you’re doing, if you’re a nurse in an office or in a place, again, where you’re not prescribing, so we may not be making the actual changes or the prescribing, but what we can do is, if we know about these medications, we know about the data, we can make recommendations, so that, so that those patients can then go back to their ordering providers. And I know our team sent many people into the cardiologist’s office with a good list of questions about certain medications. And I, I know those cardiologists appreciate it from us, but I, but it’s really been good. It’s been good for us to have the patient advocate for it, for themselves. It’s better than them hearing it, that they saw it on a commercial on TV.
Also, I mentioned, I run a post-discharge clinic for high-risk patients. So, I’m often not seeing a patient more than maybe just a couple times. For many years, we ran a support group meeting—kind of before COVID—for these patients, and [00:21:00] we did discuss the medications that they may have seen on TV ads or heard about from friends. And we talked about the new research coming. So I may not have always been the one prescribing it, but we were very much putting the recommendations in front of them, because a lot of times people aren’t having that conversation about what that data is showing.
You know, you get creative and explaining data to different people, but I think it really is just so important that we are having these conversations with both our fellow clinicians, but also with the patients, again, even if you’re not in a space where you may be prescribing the medication.
Geralyn Warfield (host): We have actually covered quite a bit of ground today, and there is probably a series of questions that some of the clinicians that are listening to this podcast might have. What kind of resources might you point them towards so that they could get some additional answers or have some resources at hand? Colleen, could you start?
Colleen McIlvennan (guest): Yeah, I think there, are a lot of great resources. The number one that [00:22:00] I would mention is the new AHA, ACC and HFSA heart failure guidelines that were published in April of 2022. I think there are, it’s laid out very easily to reference and go through for patients with heart failure. It’s available freely online and it’s also available, through any of the journals.
Kim Newlin (guest): Yeah. And I, we’ll again, we’ll post some of these links in the podcast notes. But I also want to make sure you know about the Preventive Cardiovascular Nurses Association website. So, we have educational modules for you, because we know you’re so excited and want to learn more about the pathophysiology and all the medications.
And we also have educational topics for patients. So, there’s, you know, things on there for you, such as the pocket guide for managing cardiovascular risk for people with diabetes, patient tools for people with [00:23:00] diabetes, heart failure, and cardiovascular disease. At their most recent Cardiovascular Nursing Symposium, in the pharmacology sessions, we had a presentation on the impacts of SGLT2s and GLP-1s on CVD, diabetes, and renal function; and there is listed out all the tables and, and a lot more of the research. We also had one on heart failure.
And I, of course, I have to give a shout out to our amazing co-presenter here for this podcast, but Colleen had an excellent presentation for our 2021 heart failure summit. And it was called New and Emerging Treatments for Heart Failure. And as you could hear, I mean, you could hear her explain it in this podcast. You get even more of that information. So really, really great course.
And you can, go onto the website, pcna.net, and get access to some of these courses. There’s probably about 10 courses in the last year and a half about these agents and really making sure you’re getting your patients on the right medication.
Geralyn Warfield (host): It has been delightful spending time with Colleen [00:24:00] McIlvennan and Kim Newlin talking about SGLT2s and GLP-1s and how they’re cardioprotective for card, for our cardiovascular patients—particularly those with heart failure,
This episode is available for CE contact hours. Please make sure you follow the link in the episode show notes, to complete the post-test and access your CE certificate.
We are so grateful to you, our listeners, and to our guests.
This podcast is supported by independent educational grants from Merck Sharpe Dohme Corporation, and the Pfizer-Merck Alliance.
This your host, Geralyn Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Heart Failure
Published on
September 21, 2022
Listen on:
PhD, DNP, ANP, FAHA, FHFSA

ANP-C, CNS, RN, FPCNA
Related Resources