In patients with heart failure, remote hemodynamic monitoring can identify health changes long before symptoms appear, contributing to slower disease progression, improved patient outcomes, and reduced rehospitalizations. Learn more about current and future technology that can support better patient health, and the role of nurses in patient education and monitoring. Guests: Linda Park, PhD, MS, FNP-BC, FAAN, FAHA, FPCNA, and Eryn Bryant, MSN, APRN-CNP, FPCNA.
Episode Resources
- PCNA Heart Failure Tools
- Tele-HF study
- CHAMPION Trial (CMEMs after CRT): Pulmonary Artery Pressure-Guided Management of Patients With Heart Failure and Reduced Ejection Fraction
- Journal of American College of Cardiology paper, Remote Monitoring and Heart Failure Scientific Statement
- European Society of Cardiology consensus statement
- BMAD trial: Wearable Remote Monitor Reduces Hospital Readmission Risk in HF Patients – American College of Cardiology
- GUIDE-HF trial (CMEMS, Lancet): Haemodynamic-guided management of heart failure (GUIDE-HF): a randomised controlled trial – The Lancet
- ESCAPE trial (using RHC / pulm art pressures to guide therapy during ADHF: Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial
- MONITOR-HF trial (improved QOL and functional status w/ CMEMs): Remote haemodynamic monitoring of pulmonary artery pressures in patients with chronic heart failure (MONITOR-HF): a randomised clinical trial
- MONITOR-HF: Pulmonary artery pressure monitoring in chronic heart failure: effects across clinically relevant subgroups in the MONITOR-HF trial
- MONITOR-HF summary in American College of Cardiology: Remote Hemodynamic Monitoring of Pulmonary Artery Pressures in Patients With Chronic Heart Failure – American College of Cardiology
- HeartLogic: HeartLogic Multisensor Algorithm Identifies Patients During Periods of Significantly Increased Risk of Heart Failure Events
- SCALE-HF-1 Trial (bodyport scale to predict worsening HF trends): Use of a Cardiac Scale to Predict Heart Failure Events: Design of SCALE-HF 1
[00:00:00] I’m Eryn Ferranti, board president for PCNA, and I’d like to welcome you to this episode of the Heart to Heart Nurses Podcast. PCNA is the proud home of cardiovascular nurses and one of the leading figures in the fight against cardiovascular disease. We have the resources you need for your day-to-day practice or to follow your passion to new areas of learning and growth.
Geralyn Warfield (host): (00:19)
I’d like to welcome our audience to today’s episode where we are going to be speaking about heart failure and remote hemodynamic monitoring. I’m joined today by two great guests, and Linda Park and Eryn Bryant are going to share their expertise with us. Linda, could you start us off by introducing yourself, please?
Linda Park (guest): (00:34)
Sure. My name is Linda Park. I am an Associate Professor at the University of California, San Francisco. I also hold a position at the San Francisco VA and work as a nurse practitioner at John Muir Medical Center in the Cath Lab area.
Geralyn Warfield (host): (00:50)
Wonderful. Eryn, how about you?
Eryn Bryant (guest): (00:46)
Hi. Thank you, Geralyn. I’m Eryn Bryant. I’m a nurse practitioner at Ohio State University Wexner Medical Center. I run our Heart and Vascular Transition of Care program for our heart failure population as well as our cardiac surgery population. I also co-founded our Heart Wellness Clinic.
Geralyn Warfield (host): (01:16)
Thank you both so very much. We really appreciate you sharing your time and expertise with us. And let’s go ahead and dive into our topic, again, which is about remote monitoring.
And, Eryn, I’m hoping you can start us off by talking about the importance of earlier effective management and how patient disease progression is affected by that.
Eryn Bryant (guest): (01:33)
Yeah, absolutely. So early detection is critical. The sooner we can spot signs of worsening heart failure, the more options and opportunity we may have to intervene. So remote monitoring is one of those tools that provide increased visibility to spotting these physiologic changes, sometimes days or even weeks before symptoms or weight changes could potentially trigger a patient to reach out to their care team or even present to the emergency room or hospital.
We know that heart failure is not static. It’s a progressive disease. And each hospitalization can accelerate the patient’s decline, increase risk of mortality, diminish quality of life.
So, with remote monitoring capabilities in this space, the goal is really early identification and then proactive interventions to optimize their medical therapy or volume status, rather than just being reactive and kind of behind the eight ball. And then having to default to escalating to the acute care setting.
So again, hopefully we want to improve the disease trajectory and just give the patient better quality of life.
And then finally, longitudinally following a patient and having better visibility into their disease state and their trends gives us—the care team, our nursing team—the opportunity for ongoing discussion around things like lifestyle modifications and the importance of healthy diet and activity.
And really, again, increase touch points to make sure we’re addressing all of those cardiac risk factors that can also exacerbate heart failure. So, it’s one tool in our toolkit, but it can be a very powerful one.
Geralyn Warfield (host): (03:11)
So, Linda, could you talk a little bit more about those early telemonitoring approaches and how that might be able to improve patient outcomes?
Linda Park (guest):
So, our early telemonitoring approaches only focused on noninvasive methods like patients tracking weights, daily symptoms, vital signs, which are things that we continue to encourage our patients to do. So just want to make sure that we are all clear that those things are very important for patients to continue to do on a daily basis.
But multiple studies show that the efficacy of these traditional approaches alone had no improvement in improving heart failure hospitalization. The major trial we think about is the Tele-HF study that was the largest randomized trial to date that studied patients earlier on between 2006 to 2010. And we found that these telephone-based interventions with telemonitoring over six months did not reduce the primary endpoint of all-cause readmission or death within 180 days compared to usual care.
So, importantly, we do need to consider patient-reported outcomes as an important variable. And they did report improved health status, which is an important consideration.
But this early research led us to innovate. And we have now developed these effective remote monitoring tools that considers current and dynamic data that reflect the true physiology and current status of decompensation. And as Eryn mentioned before, early detection of decompensation is critical and we don’t want to always be behind that eight ball.
We don’t always want to rely on weight gain as the only indicator in symptoms. And we know that typical patients who show up in the hospital for heart failure hospitalization are less than two pounds higher than their average weight. So again, not a good indicator of decompensation.
And I’m gone circle back to what I started with saying that patients are really critical in this partnership of self-monitoring, self-managing self-care, because their partnership is really critical in keeping them healthy and well.
Eryn Bryant (guest): (05:30)
Absolutely, Linda. And I echo what you said about, we want patients to be driving the ship, you know, be the captain of their own healthcare. And so, things like monitoring their weights and blood pressures, understanding, “goodness, my shoes feel a little tighter. I had to go up a belt loop.” Those things are very individualized.
And patients that do closely monitor their health status do communicate regularly with their care team. They do often, and have been dealing with heart failure for some time, they often know their own personal experience. But again, it’s very individualized. Not everybody gains a bunch of weight, but can be very volume, very congested.
Not everybody gets swelling in their feet. Sometimes fluid hides, you know. So, I think that these tools that we’re going to be talking about—and it gives our care teams, it gives us clinicians, just more insight into what’s going on in the body and sometimes much sooner than what patients may even experience.
Geralyn Warfield (host): (06:38)
So, Linda, could you segue then into some of these new or more novel approaches and their demonstrated efficacy when it comes to heart failure management?
Linda Park (guest): (06:47)
Sure. So, we’ve had a good amount of success in developing technologies and sensors over the past 10 years that have really helped the heart failure community to treat our patients better.
So, our audience probably is most familiar with CardioMEMS™, which is the pulmonary artery pressure monitoring system. It’s been on the market since about 2014. It’s an implantable sensor that enables real-time continuous delivery of data on pulmonary artery pressures.
And as a refresher to the pathophysiology behind all this, PA pressures are regulated by the volume of blood and the resistance in the vasculature. And when there is resistance and compromise in the pumping function, as in heart failure, at least to this backup and buildup within the heart chambers, and then an increased pressure extends to the pulmonary circulation, causing these elevated PA pressures, which is the role of the CardioMEMS™.
It detects these fluid build-ups and then informs the management team on the other side. That again, we can get ahead of this instead of relying on the traditional methods, such as the weights that we’ve been talking about.
Geralyn Warfield (host): Can you talk a little bit more specifically about CardioMEMS™? How does a person get one? How does it work?
Linda Park (guest): (08:27)
Yes. It’s available to be implanted in the hospital, so your center has to have access to this. Patients require a right heart cath, and the small device is implanted into their pulmonary artery. It’s about the size of a paperclip. And then patients are sent home with this pillow-shaped external device that they lay on, and then it wirelessly transfers the data over to the heart failure team.
And then on the back end, the clinicians are able to access the data via a web interface and then contact patients as needed based on their data, and titrate medications.
And in terms of the research behind this, the pivotal Champion Trial is the one that we all refer to that studied CardioMEMS™ and demonstrated a 37% reduction in heart failure-related hospitalizations compared to, in the intervention group, compared to standard of care over 15 months.
It had to be validated in the post-approval real world studies because it was done, the CHAMPION trial was done in the COVID era. And those real-world studies continue to show sustained benefits. Some cohorts even showing up to a 57% reduction in heart failure hospitalizations compared to pre-implant rates.
So, the data is really exciting and the meta-analyses that are coming out have also shown benefit in terms of mortality reduction.
Geralyn Warfield (host): (09:32)
So, what kind of patient would we be looking at that might be eligible for this kind of device?
Linda Park (guest): (09:53)
Yes. So, eligibility was previously restricted to NYH class III patients who are very, very sick, but now have been expanded to high-risk NYH class II patients who’ve been recently hospitalized for heart failure in the past year, and/or have elevated natriuretic peptides.
But importantly, we need to consider CardioMEMS™ to be contraindicated, or really take into consideration, those who can’t take anticoagulants or dual anticoagulant therapy for one-month post-implant, as well as patients who have an active infection, history of PE, DVT, congenital heart disease, and those who may have an indwelling mechanical right heart valve. And those who can’t tolerate a right heart cath for some reason. So different considerations.
Geralyn Warfield (host): (10:33)
And Eryn, are there any other novel, non-invasive approaches that support heart failure monitoring that we might talk about?
Eryn Bryant (guest): (10:42)
Absolutely. And as Linda mentioned, I think many of us are familiar with CardioMEMS™ and there’s a lot of exciting data to support using CardioMEMS™ in our heart failure population. But there’s been some exciting and interesting innovation and movement in the non-invasive options that are now out there, and they can be easy for patients and clinicians to use and deploy.
So, in the Journal of American College of Cardiology paper, Remote Monitoring and Heart Failure Scientific Statement [Remote Monitoring for Heart Failure Management at Home], which was published like late 2023, this emphasized that we need scalable, patient-friendly tools that don’t add a lot of complexity.
Technologies that were highlighted included things like wearable patches, bioimpedance scales, kind of home-based sensors, and these things can track patient’s heart rates, heart rhythms, activity, sleep, thoracic impedance, without requiring an implant.
And many of these devices integrate directly with smartphones. So, it makes the patient experience really smooth.
And then more recently in the European Society of Cardiology consensus statement, which was published this year, Remote Monitoring and Heart Failure, that paper described how, again, non-invasive systems are pairing with AI and predictive analytics with those wearable sensors.
So, for example, things like daily weight, blood pressure, or bioimpedance trends can be combined into kind of like risk scores that proactively flag patients who are likely to decompensate.
So, the focus has kind of shifted from just collecting the data, and this large-scale data being sent to the care teams, to actually generating actionable alerts for care teams. So, nurses and advanced practice providers, we’re not drowning in data, instead getting kind of meaningful, timely insights.
Geralyn Warfield (host): (12:35)
Thank you both so much for that overview of some of these technologies that can really support our patients with heart failure. And I’m wondering, Eryn, what this really looks like in your clinic setting.
Eryn Bryant (guest): (12:45)
So, as I mentioned before, I lead our, I’m the clinical lead for our transition of care program. And so that’s for patients that are leaving the hospital and transitioning to home, or home health, or their skilled nursing facility.
And so, we’ve been able to layer on remote hemodynamic monitoring for our heart failure patients as part of their transition of care programming. So, this really allows for more eyes, so to speak, on our patients that are in that critical post-hospitalization phase.
A few years ago, as we were building out the transition of care program, we were looking for options to augment and build upon our already-established CardioMEMS™ program.
And so, the timing was great because what was presented as a late-breaking trial at ACC 23, I believe, was the BMAD Trial.
So, this trial was an international study over, I believe, 500 recently hospitalized patients. And those patients wore a non-invasive patch called a μCOR, which measured thoracic fluid using radio signals. And this was a randomized patient-blinded trial in that the intervention group, clinicians received—in real time—alerts when the patient’s fluid levels rose. And then in the control group, that data was hidden.
And that trial found that patients whose clinicians saw the alerts had a 38% reduction in 90-day readmissions and they reported better quality of life.
So really, the takeaway from that trial was powerful in that these wearable non-invasive devices can give teams these early warning signs that we need to adjust care before patients kind of spiral back into the hospital.
And again, as I mentioned, that post-acute timeframe is really critical for patients—as well as healthcare systems, because we know that there can be, potentially, financial implications for hospital systems with high heart failure readmission rates.
So again, at our center, we’ve deployed this μCORE device, which is actually called the Heart Failure Management System, or HFMS, as a layer to our interdisciplinary, kind of multi-layered transition of care programming.
And our team will get alerts for those patients wearing the HFMS device if they have elevated thoracic fluid index, or trends that are concerning. And then we can adjust diuretics or adjust medications, do some education, get them sooner appointments. So, it gives us increased visibility.
And then the second part, how we use that HFMS device, that wearable patch, is as almost like a screening for patients who might benefit for more permanent, long-term hemodynamic monitoring from things like CardioMEMS™.
So, for a patient who’s gotten alerts, we’ve made a diuretic adjustment. They’ve been compliant in wearing the patch, or excuse me, been adherent in wearing the patch, that might be a really great patient to consider for CardioMEMS™. So, that goes beyond the 90-day threshold that the HFMS can do.
So, every institution has different resources, but really, as Linda mentioned, not every institution has access to a cath lab or to do right heart caths. So, these patch devices, these non-invasive technologies, can be, you know, really a nice tool for those other heart failure programs.
Linda Park (guest): (16:01)
Eryn, this reminds me why I love cardiology so much. There’s so much that we can do to help our patients. There’s so much discovery all the time. There’s so much innovation. And this discussion is really reminding me of all the things that continue to develop. And hopefully we can continue to help our patients, and reduce readmissions, and improve their quality of life. But this conversation has really struck that excitement again, just for the field of cardiology. It’s just so special to be in this area.
Eryn Bryant (guest): (16:34)
Linda, I totally agree. I love that we’re seeing so much innovation in this space. I think there’s more to come. I think with integration of AI, it’s just only going to get more exciting. And I love building out programs and understanding what we can layer on to really help our patients live well, live vitally, and stay out of the hospital.
I do think it’s important that we are mindful that it’s not a one-size-fits-all. Different systems, again, will have different resources. It’s not a one-size-fits-all for patients either. So, when we’re thinking about incorporating these remote monitoring devices, technologies, hemodynamic monitoring technologies, we think about the right patient for the right intervention. And that’s not just true in this space. I think that’s for everything.
And I also think we think about what infrastructure is needed to ensure that this is really helpful and not burdensome to either the patient or the care team. And I think as part of that, again, keeping in mind the financial burden, both on systems, but as well as the patient. And so, we want to choose things that are high value, for the right patient.
Linda Park (guest): (17:53)
Excellent points. Eryn. I couldn’t agree more.
Geralyn Warfield (host): (18:00)
I’d also like to remind our audience that the information that we’re sharing as part of this podcast is going to be available in the show notes. So, if you would like to follow up on some of those research studies or any of that information, that’s easily available to you. So please just check out those show notes.
We are going to take a quick break, and we will be right back.
Geralyn Warfield (host):
We are back speaking with Eryn Bryant and Linda Park about remote hemodynamic monitoring and how that affects our patients with heart failure, as well as the staff and the teams in our clinic and hospital settings.
So, Eryn, I’m hoping you could address for us what role, or roles, do nurses have in this remote monitoring process?
Eryn Bryant (guest): (18:38)
Yeah, absolutely. So, nurses are really the backbone, I would say, of remote hemodynamic monitoring programs. And their role can start really with education, helping patients understand how to use a patch, a vest, an implant, why it matters, building trust with patients so that they stay engaged.
And then from there, nurses are often the ones watching all the incoming data, receiving the alerts. They’re on the front lines, looking at fluid trends, blood pressures, other markers of hemodynamic status, and then deciding what’s routine versus what needs escalation, and communicating that between the care team, the clinicians, and the providers and patients.
This work does not happen in isolation. As we all know, medicine’s a team sport, especially in complex chronic disease management. Remote monitoring is most effective as team-based care. Nurses collaborating with advanced practice providers, physicians, pharmacists, social workers, other colleagues to ensure that alerts lead to timely and coordinated interventions.
So many programs are now adopting diuretic escalation protocols that allow nurses to really safely titrate medications, diuretics, understanding orders, or protocol-driven pathways, as long as, again, they align with hospital policies and different state regulations. And that kind of empowerment lets nurses act quickly, when fluid status is trending in the wrong direction or patients are having signs of decompensation, to keep them out of the hospital.
So again, at our institution, under our umbrella of transitions of care program, which effectively is nurse navigation-led with interdisciplinary multi-layered interventions, we’ve built out several remote monitoring pathways for heart failure because we know, again, this is a vulnerable time post-hospitalization.
So, at the screening intake by our nurses, they assess for candidacy if patients may be able to wear HFMs or meet criteria for other remote monitoring or CardioMEMS™ devices.
And then also at our pharmacy telehealth visits, that’s also another moment of screening. Our nurses are the first to be notified for high TFI alerts or if patients are getting monitored in our remote monitoring programs, if there are things turning in the wrong direction. And they’re the ones who escalate that to the care teams and then also communicate the plan back to the patients.
We’ve built out smart phrases within our EHR to kind of guide those escalation pathways. And again, our nurses play an integral part in all of this. And the program is also overseen by advanced practice nursing.
And then, while much of the focus is on clinical outcomes, there’s also an important, as we mentioned, it’s important to think about the financial implications.
So, there’s a reimbursement component to these programs. Nursing and advanced practice nursing services can be tied to remote monitoring, such as reviewing data, making care plans, adjusting medications, conducting telehealth follow-up visits. And all of those can often be billed under chronic care management, remote monitoring codes, as well as transitional care codes depending on, again, the structure of the program.
This ensures that this critical role that nurses and advanced practice nurses play in monitoring and early intervention is supported—and also recognized—both in clinical outcomes, but also financial outcomes.
Linda Park (guest): (22:06)
Eryn, I think those are excellent points. I think this goes back to the idea of shared decision-making with patients and really being realistic about what patients can do and are willing to do at home.
It’s really their autonomy that we are trying to promote in their healthcare maintenance. And if a patient’s really not going to lay on the external pillow to transmit the data, then why are we doing an invasive procedure on them? If they’re not going to wear the patch or they don’t know how to interact with the technology behind it, it really goes nowhere.
So, it’s really being thoughtful, as you said, about the right patient and giving them all the resources to make decisions around what they can realistically use and what will benefit them.
Geralyn Warfield (host): (22:55)
Linda, do you happen to have any thoughts on the future advancements in this space? We have covered a hundred years of technology (or lack thereof) already in terms of what heart failure patients used to face and it was not a very bright future. And now that’s changed quite dramatically, but now we can look ahead to perhaps even better outcomes. So, what does the future of this look like?
Linda Park (guest):
Yes. I think the future is really exciting and bright. There’s so much innovation happening as we said already, especially in the new technologies, the devices, the AI that’s underway.
The current research is, I think, really focused on developing multi-sensor platforms that can monitor additional hemodynamic parameters, and hopefully integrate with already-existing devices that patients might have.
I think Eryn alluded to this before, but the idea of new sensors, even smart socks, using textiles to detect peripheral edema in real time. And then those wearable ultrasound patches that are then also able to monitor cardiac function and hemodynamics at home. Those are really exciting.
And then there’s a compelling idea of the smart pump where implanted device like the CardioMEMS™ is combined with an LVAD, so that the LVAD speed can automatically adjust based on PA pressures.
And then, I’ve also read studies on AI-enabled smartwatches, which many of us already have, with two lead ECG capability that’s being explored to screen for heart failure with reduced ejection fractions.
So, lots of innovation in this space. I think 10 years from now when we redo this podcast, we’ll be talking about a lot of new innovations.
Eryn Bryant (guest): (24:42)
I totally agree. I think, again, just all very exciting. I hope that we can see a moment where these technologies allow patients to have even more control over their own, you know, maybe they can titrate some of their diuretics themselves.
You know, it’s very common that patients check their blood sugars and adjust their insulin based on those readings. And so, in real world, we very often, as providers, will tell our patients, “Hey, if you gain, this is your maintenance diuretic dose, but if you gain X amount of weight or you notice a little swelling, you can take an extra here and there.”
We give them those PRN instructions for dosing, but how cool would it be if they had these sensors and that gave them real-world, real-time information and they had instructions based—from their care team—that, “Hey, if this TFI goes above this reading for this many days, this is how you adjust your medicine.”
I just think that gives people a lot of ownership and control and they feel like they’re in charge of their own body and their own health. And then, you know, I think, and obviously in a safe way, that we can monitor. So, I’m excited for that. I think that it’s coming and I think that it’ll give patients a lot more control.
Geralyn Warfield (host): (26:04)
There is definitely a lot happening in heart failure management and there’s a lot of hope. And I’m hoping that you would, Eryn, start us off talking about your top key takeaway from this episode for our audience. I know it’s hard to synthesize all this great information into kind of a nutshell, but what would you like people to know or walk away with?
Eryn Bryant (guest): (26:22)
Yes, it is hard to do one. But I think if there’s one thing that I would want to leave the audience with, it’s that nurses and advanced practice nurses are absolutely critical, central, to making remote hemodynamic monitoring work.
These technologies, and increasingly AI, do let us safely care for larger volumes of patients who may not otherwise have frequent access to their care teams. They may not be able to come into clinic visits every so often; they may live more remotely.
And then we’re also in a climate that we’re facing a lot of provider shortages. So again, I think nurses are critical in deploying these remote monitoring device technologies and being an integral part of the care team that monitors them. And these are only successful when we have the right interdisciplinary team, clear escalation protocols, and the infrastructure to support it.
And then one more thing is that really this monitoring only matters if we act on it. Again, as Linda mentioned, we should never put a patch on somebody or implant something in a patient unless there’s a plan to review the data, respond to alerts, and intervene when needed. And again, nurses, advanced practice providers are ones that really make this possible, feasible, and they’re critical in building these programs.
Geralyn Warfield (host): (27:43)
Linda, what would your top key takeaway be for our audience?
Linda Park (guest): (27:43)
Thanks, Geralyn. I think we always need to go back to the basics. Successful heart failure remote monitoring is so complex and influenced by so many other factors that are outside of our control.
It’s not just about the patient’s behavior, but it’s an interplay really between the patient and considering who makes up the patient and what their comorbidities might be, what their health literacy might be, their cognitive function, even if they suffer from anxiety or depression, are they going to use the device, their health status, as we said, and then the support systems that are around them, and our healthcare environment, which is where we come in.
And then I don’t know if we’ve talked about this a lot, but just really keeping healthcare access and equity at the forefront of the healthcare environment. Because we don’t want to isolate patients who don’t have access, and then overload patients who do have access. We really want to be equitable in our approach and expand the services and resources to every patient that we can touch. Patients deserve to have that attention and we want them to achieve their best clinical state and live with heart failure in the most manageable way with our support.
So just taking the whole patient into mind. And then all the things that surround the patient, including us that really want to support them.
Geralyn Warfield (host): (29:15)
I would really like to thank our guests, Linda Park and Eryn Bryant, for sharing their expertise, their enthusiasm and the resources that are going to be in the show notes so you can refer to those, with our audience today.
And I would also like to remind our audience that you can find other key resources about heart failure at pcna.net. So, check those out for yourself and for your patients.
I’d also like to thank Abbott for their support of this particular podcast episode.
This is your host, Geralyn Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. Visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Diagnostics and Devices
- Heart Failure
Published on
October 21, 2025
Listen on:

PhD, MS, FNP-BC, FAAN

MSN, NP-C
Related Resources
Online Interactive Guides
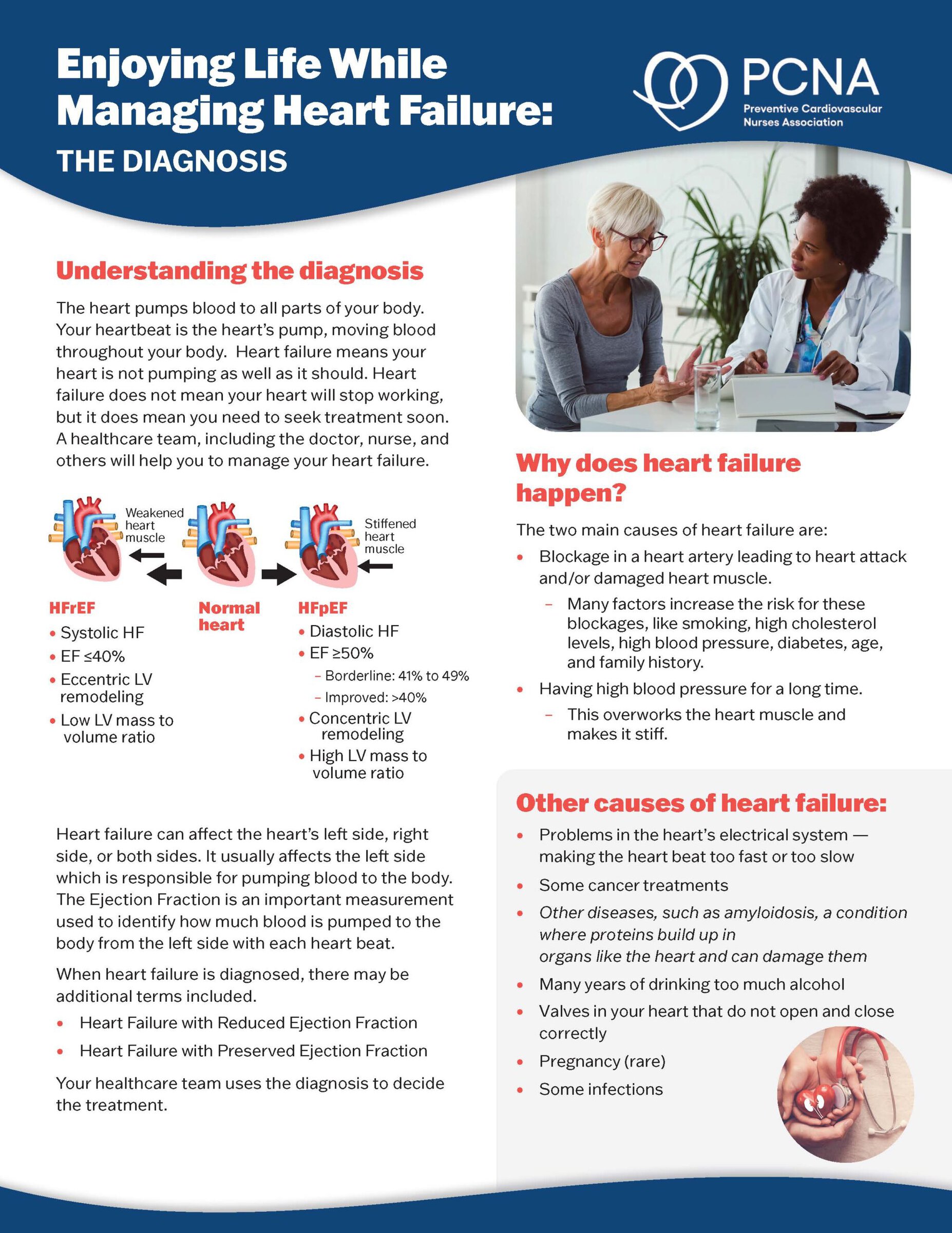
Enjoying Life While Managing Heart Failure Online Patient Interactive Guide
March 12, 2024