Afib is a progressive disease with various treatment methods to match to your patients’ risk factors and health goals. Stroke prevention is a crucial risk factor to evaluate on the progressive journey of a patient experiencing Afib. Learn more about the assessment and identification of patients with Afib at risk for stroke and next steps in prevention.
Episode Resources
- 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines
- CHA₂DS₂-VASc Score Calculator
- Clinical characteristics comprising the HAS-BLED bleeding risk score
- PCNA AFib Discussion Guide
- PCNA AFib Fibrillation Online Interactive Patient Guide
- PCNA AFib and Stroke Infographic
Thank you to Boston Scientific for their support of this episode.
Geralyn Warfield (00:19)
I’d like to welcome our audience to today’s episode where we’re going to be speaking about atrial fibrillation and the risk of stroke in our patients. And I’m very grateful to our guest, Sarah Mahipala, who is going to be joining us today talking a little bit more about this particular topic. And Sarah, could you introduce yourself to our audience, please?
Sarah (00:36)
Yes, thank you so much for having me. So my name is Sarah Mahipala. I work as an electrophysiology Nurse Practitioner. Right now I’m located in Iowa. Just kind of for background on myself, I initially started at the Cleveland Clinic in bedside nursing as a cardiothoracic ICU nurse. That’s where I figured out that I love cardiology. And as I grew to know more about it, I realized it’s more and more complex as the deeper you dive in.
And later, as I became a nurse practitioner, I wanted to find myself back in cardiology. So now I’m in electrophysiology.
Geralyn Warfield (01:09)
Well, I’m sure our audience recognizes that we have a great deal of expertise with us on our episode today, so thanks so very much for being here. And I also suspect that most of the people that are listening or watching this particular episode are familiar with atrial fibrillation, also known as AFib or AF. But I’m hoping you could start us off talking a little bit more about the pathophysiology of that. Could you do that for us?
Sarah (01:30)
Absolutely, so yes, AFib is one of our most common sustained cardiac arrhythmias. The vast majority of patients that I see in the clinic have AFib, and what happens, and how I explain it to my patients, is you have some pulmonary veins that go from your lungs to your heart. Inside the pulmonary veins, you have one type of tissue lining it. Inside the heart, you have a different type of tissue. As those areas meet, it’s more arrhythmogenic. It’s where AFib wants to start and spread.
So there’s various ways that we treat it, but that’s the initial journey. Factors that would stretch the top of the heart, cause some dilation, increase the pressure are just going to make AFib progress faster. It’s very important as we talk about AFib that we use a language where it’s progressive. Because initially someone will generally note, a few years ago I used to have some palpitations. It was for a few seconds I ignored it. And then maybe a few months later or years later, they’re having some episodes that are a few minutes. Again, progressive nature. Then we go to hours, days, and now we’re stuck out of rhythm. That’s how I generally find someone’s progressive journey with AFib.
Geralyn Warfield (02:39)
And why does AFib increase stroke risk?
Sarah (02:43)
Yeah. So that’s a great question. When we have atrial fibrillation on the left side of our heart, we have a little pocket. It’s called a left atrial appendage. So it’s a finger shaped pocket right on the outside of your heart. It’s a normal feature. It’s not something special about someone that has a fib. We all have it. If you’re in a normal rhythm, blood goes into that pocket, out of the pocket, into the pocket, out of the pocket. When you go into atrial fibrillation and the top of the heart is quivering, blood goes in there and it can pool.
Now anytime blood sits anywhere and wants to clot, that can become dislodged, it can go straight to our brain and cause an ischemic stroke. That’s where we have the stroke possibility from atrial fibrillation. I say possibility because not everybody that has AFib, as it’s a very common arrhythmia, ends up having a stroke.
Geralyn Warfield (03:32)
Well, we are going to take a really quick break and we will be back to continue our discussion on AFib and stroke risk.
Geralyn Warfield
Before the break, you described how AFib can contribute to stroke risk, and are there any particular risk factors that put someone at increased risk?
Sarah (03:47)
Absolutely. So right away when I get a patient that has atrial fibrillation, I’m considering two things. I’m considering whether they could possibly have a stroke or whether they could go on to have heart failure. So when it comes to a stroke, we have a nifty tool that is used most broadly, the CHADS2VASC score. There’s a few other ones out there, but CHADS2VASC is the one that is commonly used.
And it basically triages someone’s likelihood of having a stroke statistically. So that is going to assign points based on whether they have high blood pressure, whether they have heart failure, are they diabetic? Have they had a previous stroke or TIA? Do they have any kind of vascular disease? What is their age? Are they greater than 65? Are they greater than 75? Are they a female? All of these paint a picture as far as how likely it could be for someone to have a stroke.
I like to tell my patients, it’s not that you have AFib where you’re going to have a stroke. It’s the company that atrial fibrillation keeps that makes it more likely for you to go on and to have a stroke.
Geralyn Warfield (04:52)
So it sounds like that CHADS VASC score is a great tool for our health care professionals to be using in order to assess that risk. Is that accurate?
Sarah (05:00)
Yes, absolutely.
Geralyn Warfield (05:01)
And so you also talked about the progression of AFib and does the type of AFib that a person has have an impact on their risk of stroke?
Sarah (05:10)
That’s a great question. So, to classify atrial fibrillation, initially, we would say if someone has a small amount of atrial fibrillation, they don’t stay out of rhythm for more than two weeks at one time, they have paroxysmal. Then we go on and when it’s more persistent in nature, surprise, it’s called persistent atrial fibrillation. They’ve been out of rhythm now for a stretch longer than two weeks. We even have long standing persistent or it can be a year and then permanent where we don’t even worry about getting them back into rhythm. A common myth is
If it stops on its own, the stroke risk is lower. That’s untrue. It doesn’t matter, as you saw from the company that atrial fibrillation keeps, that is what is predictive of your stroke risk. It’s not the length of time that you’re out of rhythm.
Geralyn Warfield (05:55)
So we know that nurses work in a variety of settings and they have different roles, in fact a multitude of roles when working with these patients that have AFib. So I’m hoping you could address for us what kind of strategies would you suggest to help nurses to have the most impact when they are trying to help these patients reduce their stroke risk?
Sarah (06:14)
Absolutely. So nurses play such a vital role to educate our patients, to help them to understand our diagnosis, to understand why we’re taking different meds, why we don’t substitute certain other meds for the meds that were actually prescribed. So it’s key to help break down the AFib in simple terms. Calm their fears regarding their arrhythmia. They’re not going to die from it. It can be miserable. We have a lot of treatment options out there.
We want to increase their quality of life, right? Help set some expectations as far as the progressive nature, okay? It’s common for people to be shocked that their AFib is back, you know? Even when I’m in the hospital setting, as I’m talking to different staff in the hospital, they’ll be, you know, rapidly paging like, the patient’s back, you know, an AFib and they have atrial fibrillation. They can go in and out of it. It’s not a crisis. Their strategy is to help keep them in rhythm. So continue to use that language so that it’s helpful for us as we talk to them. Another thing is always encourage lifestyle changes. We want to slow the progression of atrial fibrillation. It’s going to get worse when individuals are gaining weight, when they are using alcohol, nicotine, when they have untreated high blood pressure, if they’re not treating their sleep apnea and we know that they have it, if they’re not exercising. So we still want to encourage them to do different lifestyle changes. Now, the second thing that would be really helpful is whenever we are talking to them about a blood thinner and we talked about the CHADS2 VASC score, there are some individuals that are placed on a blood thinner because their risk factors are high enough. But not everybody needs a blood thinner. There are times where we stop it because actually the risk factors for bleeding are too high and the risk factors for a stroke aren’t adequate. So if we have a man who has one risk factor, he has high blood pressure, he’s 40 years old, at certain scenarios, he doesn’t need to be in a long-term blood thinner yet. It’s okay. Then there’s plenty of other times where the risk factors are quite high, right? And we need to keep them on that blood thinner.
Another hard thing to do is people, you know, their bodies are constantly changing, their lab values are changing. So keeping us in check as far as their kidney function. So if we notice that someone’s kidney function is starting to slow down, we might not need to give them as much Eliquis®. We might not need to give them as much as a Xarelto®. So help to keep us informed if something has drastically changed so we can reassess to make sure that they have what they need.
Also, something I see commonly is when patients are taking baby aspirin instead of taking an actual blood thinner and they, you know, hey, it’s a baby aspirin. I won’t have a stroke. A baby aspirin is not powerful enough to thin the blood in that left atrial appendage to prevent a stroke. So we have to confront those like myths and then, you know, steer them gently back to using their blood thinner. We also don’t need them to be on triple therapy always. So if you start noticing that they are on their blood thinner, Plavix®, aspirin, because people have aspirin over the counter. Sometimes they just add it in there because, hey, it’s supposed to be good for the heart. That might not be what’s recommended. So, you know, flag those people for us to just take a look, make sure that we’re not at an increased risk for bleeding because of the extra anticoagulation that they’re on. There’s also aspects where we notice they’re not taking it as they should, right? Nursing will notice that before I do. Like, hey, I see that they commonly miss a dose. Eliquis® is supposed to be dosed twice a day. Most of time, they’re just taking it once a day. Well, if they’re not taking it adequately, we’re not going to get the results that we hope. So maybe we need to talk about pill packs. Maybe we need to switch to Xarelto® so it’s once a day. Maybe they’re taking their Xarelto®, but they’re not taking it with food. We need food in our stomachs in order to absorb Xarelto®. So lots of communication just around just the simple properties of, are you taking your meds? When are you taking them? What are you taking it with? Ensuring that there’s not other drug interactions. For instance, I really struggle sometimes with when drugs are added on that I’m not aware of. So maybe it’s for seizures, for instance. There can be some seizure drugs that interact with our blood thinners, and there’s really not a great option besides Coumadin®. So even just keep on doing the med check. Keep on reassessing for changes so that we can do our best job keeping them safe.
And then a third way to be helpful would just be attentive to bleeding risks. So there’s another score that we use, it’s called HAS-BLED. And it’s a way that I try to categorize who’s at higher risk for having a bleeding event when they’re on anticoagulation. So we’re looking at whether they have liver abnormalities, if they have kidney function that’s really low, their INRs are all over the place, right? If they’ve had transfusions before. Certainly having hemorrhagic stroke, right? That’s going to be something that we need to talk about. Uncontrolled high blood pressure. Those in and of itself isn’t a reason why I stop a blood thinner, but we need to be careful when things have changed because some of these factors can be modifiable, right? If we have more meds on board, like the baby aspirin, I want to know about that. Maybe they don’t need to take it and I can modify their risks for bleeding.
Fall risk is something to consider, but interestingly, it’s not actually part of that has blood score. There can be a lot of factors to falling, right? We can have low blood pressure. It can be mechanical. We have to ask a lot more questions instead of just saying, man, you’re high risk for falls. We shouldn’t really be on a blood thinner. It’s a conversation opener for a provider.
Other than that, the next is just providing care coordination. Keep the family doctor in the loop. Keep us in the loop. So whether it’s general cardiology, electrophysiology, I like to know when things change. I like to know when someone has had a bleeding event and then if their blood thinner was stopped. Because there’s more that I can offer for them besides their blood thinner as far as their stroke risk.
The earlier I am aware, the sooner I can start making a referral. Start working to make sure we have everything lined up for them. And then certainly some red flag symptoms that I like our nursing staff to be aware of is any new neurological symptoms. We can have a stroke and we can be on a blood thinner. It’s rare to have it happen. But we need to know. Hey, that sounds like a TIA. That sounds like a stroke. Let’s talk about this further. Let’s evaluate. Let’s get the doctors involved, right? Severe high blood pressure. I want to know about that. Any kind of GI bleeding or anemia while they’re on a blood thinner, I want to know about that.
Overall patient empowerment, help the patients know when to call the clinic. What is abnormal? What is normal? And, signs and symptoms of a stroke or bleeding.
Geralyn Warfield (13:15)
So in your clinical setting, what does that referral process look like for this LAAO process?
Sarah (13:22)
Yeah. So, when it comes to deciding, okay, a blood thinner may not be a good long-term solution for your stroke risk. Let’s consider placing a left atrial appendage occlusion device, right? Cause that’s where our stroke risk factors come from, blood in that pocket. Could we seal it off? Could we go in through the groin up to the top of the heart with the catheter seal it off with like an umbrella shaped device that just seals over that pocket.
Initially, I like to get all my facts together. To see, okay, what was the event that makes me nervous about having you on a blood thinner? Make sure that’s appropriately documented in my notes. What’s your hemoglobin now? Are you on the blood thinner or was that stopped? Was it GI bleeding and they were able to cauterize the site and now they’re saying it’s okay for us to retry being on a blood thinner. What is our CHADS2 VASC score? Should we even be on a blood thinner or actually are we low risk and we don’t even need to consider long-term blood thinner and therefore that WATCHMAN or left atrial appendage occlusion device?
But once we have that, then I refer. We have a few larger centers locally and we reach out, we send them directly to those centers, but my notes have it triaged so that they can also prioritize who really needs to be seen right away and who can wait a few more weeks and then be evaluated.
Geralyn Warfield (14:45)
I really appreciate you going through all those steps in terms of the referral process. And it’s a great segue for our next episode in this mini series where we’re going to talk more about left atrial appendage occlusion devices. I had to refer to my notes because that’s a lot of words all strung together without that acronym. And so I’d like our audience to check that particular episode out as well. And I have one more question for you today. If you had one quick takeaway for our audience, what would it be for today’s episode?
Sarah (15:01)
Yeah. So, atrial fibrillation is common. Ischemic strokes from AFib are preventable. Our goal is simple, reduce strokes, improve quality of life, and walk alongside patients as partners in their AFib journey.
Geralyn Warfield (15:27)
Well, it has been a delight spending time with you today, Sarah. Thank you so very much for sharing your expertise with our audience. And if you have any more questions or any more information that you would like to get about this particular episode, you can take a look in the show notes, or you can also look at PCNA.net and find even more. Also, another reminder to please check out the second episode in this mini-series. And a thank you to Boston Scientific for their support of this episode. This is your host, Geralyn Warfield, and we will see you next time.
Topics
- Atrial Fibrillation
- Diagnostics and Devices
- Risk Assessment and Management
- Stroke
Published on
December 2, 2025
Listen on:

MSN, RN, CCRN, FNP-C
Related Resources
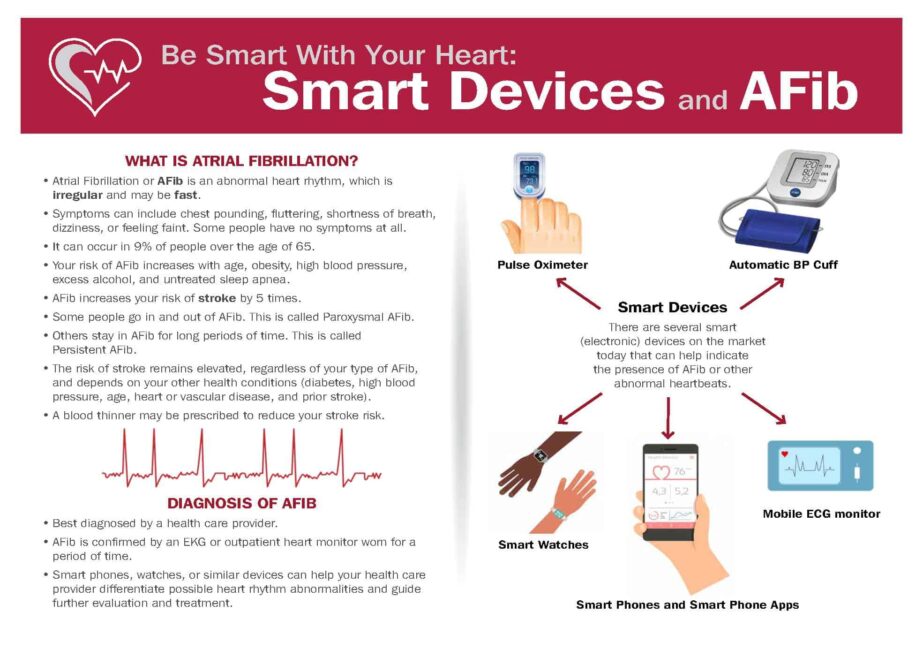
Patient Education Handouts
Be Smart With Your Heart: Smart Devices and Atrial Fibrillation
February 09, 2026

- « Previous
- 1
- 2
- 3
- Next »