The bidirectional relationship between cardiac and renal systems means that any dysfunction can cause a cascade of health issues. Learn about team-based care strategies for nurses and other professionals to monitor and manage patients with these conditions from guests Andrew Bzowyckyj, PharmD, BCPS, CDCES, FAPhA, FADCES, and Serina Gbaba, DNP, MBA, FNP-BC.
Episode Resources
- PCNA CKM tools and resources
- IPEC core competencies (Interprofessional Education Collaborative)
- CVD in CKD: Pathophysiological Insights and Therapeutic Options
- Social Determinants of CVD, Circulation Research Volume 130, Number 5
Thank you to Novo Nordisk for their support of this episode.
[00:00:00] I’m Erin Ferranti, board president for PCNA, and I’d like to welcome you to this episode of the Heart to Heart Nurses Podcast. PCNA is the proud home of cardiovascular nurses and one of the leading figures in the fight against cardiovascular disease. We have the resources you need for your day-to-day practice or to follow your passion to new areas of learning and growth.
Geralyn Warfield (host): (00:19)
I’d like to welcome our audience to today’s episode where we are going to be focused on CKM or Cardio-Kidney-Metabolic Syndrome. And I’d like to introduce our guests to you. Andrew Bzowyckyj, would you like to introduce yourself first, please?
Andrew Bzowyckyj (guest): (00:32)
Yeah. Hey everyone. Thanks for having me. My name is Andrew Bzowyckyj. I’m a Senior Scientific Director at the National Kidney Foundation. Part of my role is to design and develop educational programming for patients and professionals.
And just for the audience, my background, I’m a clinical pharmacist and a diabetes care and education specialist, by background from primary care and endocrinology. So, I bring that experience with interprofessional practice and in education. And I look forward to talking with you all today.
Geralyn Warfield (host): (00:57)
Sounds wonderful. Serina, how about you?
Serina Gbaba (guest): (00:59)
Hi, my name is Serina Gbaba. I’m a cardiology nurse practitioner. My patient population involves patients with heart failure, renal disease, and they also have cardiomyopathies.
Geralyn Warfield (host): (01:18)
Well, thank you both so very much for being here today. I’m really grateful to you for sharing your expertise with our audience.
In order for us to get started, maybe we can level set a little bit, Andrew, in terms of that relationship between kidney and cardiac dysfunction. Could you talk about that for us, please?
Andrew Bzowyckyj (guest): (01:34)
Absolutely, and that is not an easy question to start off with, but probably a good background that our audience, I’m sure, very well knows.
So, the heart and the kidney, they work best when they’re in sync. They need to work together, they need to be on the same page.
And then you’ve got the vasculature that’s kind of that conduit between the two, plus all of the other things that are going on in the body. So, you’ve got the heart, you’ve got the kidneys, and they need to really be on the same page.
Obviously, the heart sets the tone and so it helps with rate. It helps with force, kind of keeping the blood flowing, keeping the blood moving.
And then the kidneys are kind of reacting to that to help balance the salt, balance the fluids, the leveraging renin, aldosterone, all of those factors come into play.
What I think is important to remember, and oftentimes we forget when we get into our specialty silos, is it’s still one body. So, all of these things need to be working in that person’s …whatever is happening inside the body, need to treat the person and not necessarily one organ or the other.
With kidney dysfunction, and I’m sure Serina is going to go into way more detail than I possibly could, but we get into accumulation of fluids and toxins, albuminuria, I think is a huge thing. Even in the absence of reduced eGFR, we see some of the earliest kidney disease comes with albuminuria before people are even thinking, CKD is not even on their radar.
And then obviously in a more advanced stages, you get vascular calcification, phosphate, disbalances, all of those types of things.
On the cardiac side, so cardiac dysfunction, obviously you get circulatory perfusion problems, the blood’s not getting to where needs to go. You’re sending mixed signals to the kidneys, so that leads to kind of more fluid accumulation, you know, everyone’s kind of picking up on the vibes that the other organ is sending, and so that obviously can lead to significant dysfunction.
I think who started it can change from patient to patient. So, sometimes it starts in the heart and kind of moves down to the kidneys. Sometimes it’s back the other way. And, obviously you’ve got acute, chronic, acute on chronic, which again, think Serina can speak to a lot better than I.
But one of the last things I wanted to emphasize was to kind of connect that to that cardiovascular-kidney-metabolic syndrome, which is kind of the newer terminology, evolving from cardio-renal syndrome, is the heart and the kidneys, as I mentioned before, don’t exist in a bubble. And so, there’s a magnitude of factors that are kind of surrounding and affecting the entire environment. That’s where you get into metabolism, obesity, diabetes, systemic inflammation, all of that is kind of that wraparound. And so, it’s kind of cool to see that come into the fold here in this new paradigm.
Geralyn Warfield (host): (03:58)
Thanks so much, Andrew.
Serina, the way Andrew described it, the image that popped into my head was that almost of a spiderweb, where when you tug just gently on one of those web components, it really impacts the rest of the body. So, could you talk to us a little bit more about those interconnections and maybe even parts of the body that we would be surprised impacts this cardio-renal or cardio-kidney-metabolic syndrome?
Serina Gbaba (guest): (04:21)
Sure, thank you. So, there are officially five types of cardio-renal-metabolic syndromes.
The 1st one is acute heart failure resulting in acute kidney injury.
And now the 2nd type would be chronic heart failure resulting in chronic kidney disease.
And you also have the 3rd type with acute kidney injury resulting in acute cardiac dysfunction such as heart failure.
You also have [4th] primary chronic kidney disease resulting in cardiac dysfunction.
And the 5th type is a systemic disease like diabetes or sepsis causing cardiac-renal dysfunction.
As Andrew already stated, a dysfunctional heart can lead to a dysfunctional kidney. So, I will describe the 1st type of cardio-renal syndrome, where you have acute heart failure resulting in acute kidney injury.
And how the mechanism of how that happens is, you have with acute heart failure, you have a decrease in cardiac output. So, the decrease in cardiac output leads to a decreased perfusion of the kidneys, which results in acute kidney injury.
And with the decreased cardiac output, which activates the kidney to release renin. Renin activates the renin angiotensin-aldosterone system, RAS. RAS, in turn, activates the antidiuretic hormone, which results in water retention and sodium retention. This increase in fluid volume, increases blood pressure afterload, which in turn decreases cardiac output, which leads to what? Acute kidney injury.
Additionally, RAS causes vasoconstriction, which results in a decreased perfusion of the kidney, which again exacerbates the acute kidney injury.
The decreased cardiac output also activates the sympathetic nervous system. And this activation causes vasoconstriction, which decreases renal perfusion, further worsening acute kidney injury.
So, in addition to that, how do we treat acute heart failure? We usually use diuretics to decrease pulmonary and vascular edema. And what happens with that? It can result in hypertension, decreased preload, leading to lower renal perfusion, further worsening renal function.
So, as you can see with this Type 1cardio-renal syndrome, the acute heart failure, leads to the acute kidney injury.
Then you have, on the other hand, like Andrew stated, a dysfunctional kidney can result in cardiovascular dysfunction.
So, I will describe the 4th type of cardiorenal syndrome where you have chronic kidney disease resulting in cardiovascular dysfunction. So, the mechanism of how that happens is, you have a patient with chronic kidney disease. Chronic kidney disease has low glomerular filtration rate, eGFR, which activates the RAS. I’ve already described that RAS causes vasoconstriction and fluid retention, which results in hypertension.
So, with chronic kidney disease, you have chronic hypertension, which can cause cardiac remodeling and left ventricular hypertrophy, which in turn can lead to cardiac dysfunction.
In addition to that, with chronic kidney disease, you have low erythropoietin levels resulting in anemia. Anemia can result in cardiac ischemia because of the demand-supply mismatch.
Additionally, with chronic kidney disease, you also have low vitamin D levels. And Andrew mentioned that earlier. So, through a cascade of events, you end up having increased serum calcium and phosphate, which causes calcification of coronary arteries, increasing risk of ischemia, which is a cardiovascular dysfunction.
Additionally, with chronic kidney disease, you also have electrolyte imbalance such as hypokalemia, which can cause arrhythmias, which is a cardiovascular dysfunction.
So, as you can see, we have a situation where chronic kidney disease results in cardiovascular dysfunction. So, one system that’s dysfunctional affects the others.
And those are two mechanisms. Like I said earlier, there are five types. I just described two of them.
Geralyn Warfield (host): (09:28)
Well, I am so grateful to you both for spending time helping us understand those delicate connections. That just a slight change in one of those factors can really cause a cascade of events that might be very serious very quickly, depending upon what’s occurring.
So, as we think about nursing strategies, as we are identifying and managing these patients, what are some things that you could suggest for nurses who are involved in this kind of care?
What strategies would you offer them? And maybe, Serina, you could get started with that and then we’ll switch it over to Andrew to answer, his opportunity.
Serina Gbaba (guest): (10:04)
Okay, absolutely. So, nursing strategies for monitoring and managing patients with overlapping heart and kidney conditions involves monitoring for early signs of complications through frequent assessments.
I can’t overestimate the role of nurses because they’re at the bedside, they’re interacting with the patient during a 12-hour shift. So, one thing that we’ll be assessing for is fluid overload, fluid volume status. Is there peripheral edema? Pulmonary edema? There will be, especially for night shift, I know for nurses, that do daily weights. That’s crucial for providers to determine if the patient is losing fluid volume by comparing the daily weight.
Also, intake and output. Measuring accurately intake and output. That is so, so important.
And they also are critical to help monitor for declining renal function, such as monitoring lab results for declining creatinine. They are the first to see the lab results. At the beginning of the shift, you’re looking at your labs and you notice creatinine levels declining or creatinine increasing, rather, and GFR declining. That’s a sign of declining renal function.
As well as looking for electrolyte imbalances like hypokalemia in the case of a patient that’s getting diuretics. Also, they might be having hyperkalemia because of worsening renal function.
Vital signs: is blood pressure increasing? Is it too low because of overdiuresis? And again, like I said, intake and output.
There’s also nursing therapeutic interventions. You have medications that are prescribed by providers. Administering those medications, monitoring for side effects like hypotension, as I mentioned earlier, and declining renal function.
Also, nurses implement strict fluid restrictions, right? And ensuring that there are signs on the door, or wherever they put the signs, so that all team members are aware that this patient has fluid restriction, keeping strict intake and output like I mentioned earlier.
And I can’t even underestimate the role of nurses in educating patients and family on maintaining a low-sodium diet. And that’s so important for euvolemic status. Especially on discharge.
Or sometimes even having the hospital. I remember times where I would see patients bring it in, families bring in a bag of chips for a patient. I’m like, “My goodness!” especially they have heart failure exacerbation, they don’t need a bag of chips, you know. But just educating family members and on the diet.
Being culturally sensitive, realizing if this patient is from a particular culture, these are the high-sodium foods that they eat.
Monitoring for signs of hypervolemia, such as weight gain, edema, shortness of breath. Teaching family members about the daily weights at home and monitoring for edema, shortness of breath.
Really promoting self-management, which as we know that is evidence-based to empower patients in self-care and in self-efficacy. That is so important.
I had this patient, I remember, who kept coming in for readmission for CHF exacerbation. And I went to him, I said, “So, you know, do you cook with salt?”
He said, “No, I don’t cook with salt.”
I said, “OK, do you eat smoked turkey?”
He said, “Oh yeah.”
I’m like, “Do you eat, do you eat SPAM?”
“Oh yes, I do. I love SPAM.”
“How about bacon and ham?”
“Mmm hmm. But I don’t cook with salt.”
And I was like, I said, “You know, all those things that you mentioned, they cause you to retain fluids.”
“My goodness, I have to go empty my fridge because that’s all I have in my fridge!”
So sometimes just asking those questions can help you educate your patients to keep them from coming back to the hospital for, you know, CHF exacerbation. So, nursing’s role is so important in educating patients and their families.
Andrew Bzowyckyj (guest): (14:32)
Yeah, the educational gaps around intrinsic sodium in certain foods is significant. And that’s not a judgment. It’s just things that don’t taste salty can have a lot of salt. And I know baked goods is a huge one. The store-bought baked goods. And then frozen, you know, pre-packaged foods. Again, they don’t taste very salty. But yeah, when you talk with patients and you flip the box over and you look at the label, the jaws drop, you know, the shock is there.
So, man, you hit on so many. So, I don’t really know how to follow up with that, other than that emphasize that this is certainly a very tricky balance. And I think nurses are fantastic at understanding that again, thinking from the perspective of the whole person, in whole-person care.
Keeping your eyes on that perspective is going to be essential. So, you’re the one that’s kind of, as the specialists come by the bedside, and it’s a different rounding team or a different specialist or even a different group from day to day, oftentimes it’s the same nurse or same group of nurses that’s really caring for that patient. So really owning that role, I think, is huge.
One of the things that, so I have some experience from the inpatient pharmacy world, and sometimes there’s a tendency I’ve identified of sacrificing one organ for the other. The cardiology team comes and they do the rounds and they’ve added to, how you mentioned earlier in cardiorenal syndrome, you know, “Let’s diurese and let’s add all of these things and stop all these agents.”
And then the nephrology team comes through and they’re like, “Oh, you know, we’ve got to add this back on, and we’ve got to do this, we’ve got to do this.”
And here I am in the inpatient pharmacy verifying orders. And it’s like, wait a minute, which angle are we going? Are we going this way or are going that way?
And oftentimes, paging the teams is helpful, but then sometimes contacting the floor nurse and asking, what is going on up there? What’s happening? Tell me the story because I’m missing out on part of the story. And I need to know kind of how, as a pharmacist, I can help kind of advise and support the team for the direction we’re wanting to go. But I’m sensing two different directions we’re moving in and help me kind of build the story together.
One other piece I really just wanted to emphasize is just going back to that nurse as a patient advocate role, especially when there’s, there’s multiple specialists. And that’s the inpatient and the outpatient settings too.
I think oftentimes there’s a focus on the inpatient just because things are happening so quickly, hour by hour, but even in the outpatient side, you know, you can have three visits in one day, you can bounce from specialist to specialist, and things change.
Things don’t get picked up at the pharmacy. Transitions of care happen, meds fall off, meds get started.
And so again, that nurse, that longitudinal touch point, is so critical.
And so, I think you touched on many important points. Taking a holistic approach, looking at those labs, those symptoms, those vitals. Oftentimes these things are insidious, non-specific changes. But because you’re seeing this patient so regularly, it can kind of help. You’re kind of finding the things that people are overlooking. And I think that’s huge.
Taking that patient’s story, the patient’s priorities, if their family’s there, their care partners, whoever it may be, kind of filling in the gaps in no offense to any of the other care team members, but there’s just, we’re all stressed for time and we’re all just trying to do the best that we can with the information that you have. And so whatever extra information can be provided, it is extremely important.
And I would hope that it would be well received by the rest of the care team because ultimately at end of the day, we want to help these patients get better.
Serina Gbaba (guest): (17:51)
Absolutely. Mmm hmm
Geralyn Warfield (host): (17:53)
We are going to take a quick break and we will be right back.
Geralyn Warfield (host):
I’d like to welcome back Serina and Andrew to our conversation about Cardio-Kidney-Metabolic Syndrome, CKM, also known as Cardio-Renal Syndrome.
And you started to allude to this, Andrew, right before we broke, and that is how to partner with other key professionals. Obviously, we want to partner with patients, we want to partner with families, but how does that look in practice with our colleagues?
Andrew Bzowyckyj (guest): (18:18)
So absolutely, I think team-based care is essential. I’ve seen situations where it works very well. I’ve seen situations where the outcomes were not as great because perhaps the team was not working as well or as effectively as it could be. There’s been situations where there’s just a lot of friction and conflict and kind of putting the patient in the middle of that is sometimes very unfortunate. So, I do think, to do team-based care effectively, it includes—and I would add requires—that patient as an active team member.
And I think in this setting with Cardio-Renal Syndrome specifically, it can be difficult in the acute care setting. So, in that situation, that’s where you look at, again, care partners, family members, having someone else in case the patient needs to be sedated or needs to go for a procedure. It can be really difficult to truly provide, right?
So, when you think about goals of care discussions and you’re facing this acute, decompensated, like things are just happening so quickly moment, you know, can you really kind of gather your thoughts and decide kind of what to do.
And so that’s where that skill set is so huge to try to find a way to leverage patient empowerment in that setting.
I’m a former academic, so recovering academic, I guess. And so, I think of the IPEC core competencies, that’s the Interprofessional Educational Consortium [Collaborative], and I might have gotten that acronym wrong. But the core elements of interprofessional education are communication, roles and responsibilities, teams and teamwork, in values and ethics. And so, the more all of us as healthcare professionals can strive to be achieving these competencies, these domains, is huge.
And I think that speaks to the importance of culture. Culture is not an easy thing to develop. But developing really to doing the work, to build that culture of true clinician empowerment. You talked about patients bringing food from home, but I even think of like maybe the patient’s on the wrong inpatient diet orders and they’re on a regular diet instead of a low-sodium.
And so, being able to kind of speak up professionally. You know, professional courtesy is essential, you know, doing things the right way. When it’s for the patient, it tends to be better received than if it’s for you trying to be, you know, the smart person who’s trying to intervene. And so, when we think about it from the patient’s perspective, what’s best for the patient, that often helps. And having that culture of support, the environment, communication, and then documentation I think is critical.
So, I come from the outpatient setting. One of the things that I think was helpful, was we did kind of problem-oriented documentation. I know each medical record has a different system. And so, I don’t want to get very specific into details, but kind of documenting patient-specific goals of care, like in a centralized place. So, like when you’re working with me, you know, I’m helping you get to a blood pressure goal of X, but the primary care provider is on board. We’re all working from the same blood pressure goal, or the same A1C goal, or the same whatever it may be.
I know the inpatient setting is a little bit different, but still, having a central place, so it’s not buried in a note somewhere. And then this note says this and this note says that, and the patient’s left trying to scramble throughout. So just a few ideas that I’ve seen that I’ve worked. I’m really interested to hear, Serina, what you see in practice.
Serina Gbaba (guest): (21:26)
Yeah, absolutely. Those are great points. And I know, like you mentioned, team-based care is indispensable for managing patients with cardiac-renal disease and to minimize complications. You have, you need, that interdisciplinary collaboration between cardiology, nephrology, primary care, pharmacy, nursing, social work, care management, the family, and everybody working together for that seamless transition of care to minimize complications that will lead to emergency department visits and hospitalizations.
And I think the electronic health record is an indispensable tool in promoting interdisciplinary communication, because it informs team members of what you mentioned, the goals of care and treatment plan. Like for example, when I’m rounding in the hospital and I look for the nephrology notes, what is nephrologist saying? What’s their plan? What are they recommending? And that informs my cardiology treatment plan.
I also look for what the hospitalist is saying, what their goal is, because they’re managing the overall treatment, the global management of the patient’s care. I look for what social work is saying. I look to see if there’s a palliative consult. What the goals of care are.
I look for nursing notes. What is nursing saying? What happened last night, overnight with the patient? So, everybody, and of course you have pharmacy, their notes will be there too, especially if the patient also has atrial fibrillation and they’re on anticoagulation.
So, it’s really important to be able to read all those notes and tailor and let them inform my treatment plan. So, it’s indispensable to definitely have this collaboration and communication through the EHR. I think it was just genius to have an electronic health record that everybody can go in and see.
In addition to that, one of the things I do when I’m outpatient in clinic and I’m seeing a patient, for example, who I suspect is not able to manage their medications well, I send a message to the primary care provider. “I saw your patient today. It doesn’t seem like he has a handle on his medication. Can you get your social worker at the clinic to contact the patient and have somebody go over the medications with them?” And that helps.
And sometimes I even have the home health nurse sending me a message through the secure electronic health record and saying, “I saw your patient today, edema looks worse. What would you like this patient to do?”
So, that interdisciplinary collaboration and communication is indispensable for these patients because like you said, they can go downhill so quickly and it’s important that everybody is looking out for the better outcomes for this patient and informing the rest of the team about what they’re seeing and what the goals of care are.
Geralyn Warfield (host): (24:47)
So, we have covered a lot of ground in our podcast episode today, and I would like you to both think about what one key takeaway would you like to leave with our audience? So, Serina, I’m actually going to toss it to you first, and then we’ll switch over to Andrew.
Serina Gbaba (guest): (25:02)
Okay, I would say to remember that management of cardiorenal syndrome is a delicate balancing act because you’re trying to balance cardiac output, renal function, fluid volume status. And if you get overzealous in one area, you could injure the other system. So, it’s a delicate balancing act.
And taking into consideration, like Andrew says, it’s holistic. Taking into consideration the entire patient and what’s going on with them.
Also, nursing interventions are critical to management of Cardio-Reno syndrome, whether it is inpatient or outpatient. Their role cannot even be over-emphasized because they are critical to informing the rest of the team about what’s going on with the patient.
Additionally, you need an interdisciplinary collaboration to decrease hospitalizations, emergency department visits, and improving patient outcomes.
Geralyn Warfield (host): (26:10)
Andrew, what would you like to leave our audience with?
Andrew Bzowyckyj (guest): (26:13)
Yeah, this is going to sound extremely cliche, but to everyone in the audience, you all matter. And I know that sounds empty.
But I think what’s so important is you hear so many conversations about scope creep and, “This isn’t in my scope,” or “This isn’t in my license” or, “Why is so and so doing this? You know, that that’s not kind of their role.” But it can also be very easy to get caught up in the day-to-day, you know, “Not my job. I’ve just, I’m going to focus here where, stay in my lane and I’m going to do what I’m doing.”
But the conversations we’ve had just in the last 20 minutes, there’s just so much going on inside the body. So much going on outside the body. We haven’t even talked about social determinants of health. I know Serina talked a little bit about culture and food, but all of those pieces. It’s complicated and it’s messy.
So, the opposite of scope creep is, you know, people kind of being hyper-siloed and not necessarily practicing to the top of their licenses.
So, you for all the nurses out there, for all the other professionals who may be listening, we all have that role to play. And ultimately, we’re all there, kind of advocating for that patient. And I think that’s, it’s easily forgotten in the day-to-day routine. And so hopefully, you know, programs like this helped kind of remind you all that the work you do is hugely impactful. And so embrace that.
Geralyn Warfield (host): (27:31)
Well, thank you, Andrew. Thank you, Serina, so very much for sharing your expertise and giving that boost of confidence there at the very end, Andrew, to let us know that we do make a difference. And we all do contribute to patient health, to patient well-being, to patient outcomes. And that’s very significant. And we tend to forget that that’s really our role. So, thank you for reminding us of that.
I would also like to thank Novo Nordisk for their support of this particular episode.
I would like also to remind the audience this is the 2nd of a 3-part mini-series, there is more information in the other 2 episodes. There’s also more information at pcna.net.
Again, Andrew and Serina, thank you so very much for sharing your expertise with us.
This is Geralyn Warfield, your host, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. Visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Coronary Artery Disease (CAD)
- Diabetes
- Kidney Disease
- Obesity Management
Published on
November 4, 2025
Listen on:

PharmD, BCPS, CDCES

DNP, MBA, FNP-BC
Related Resources
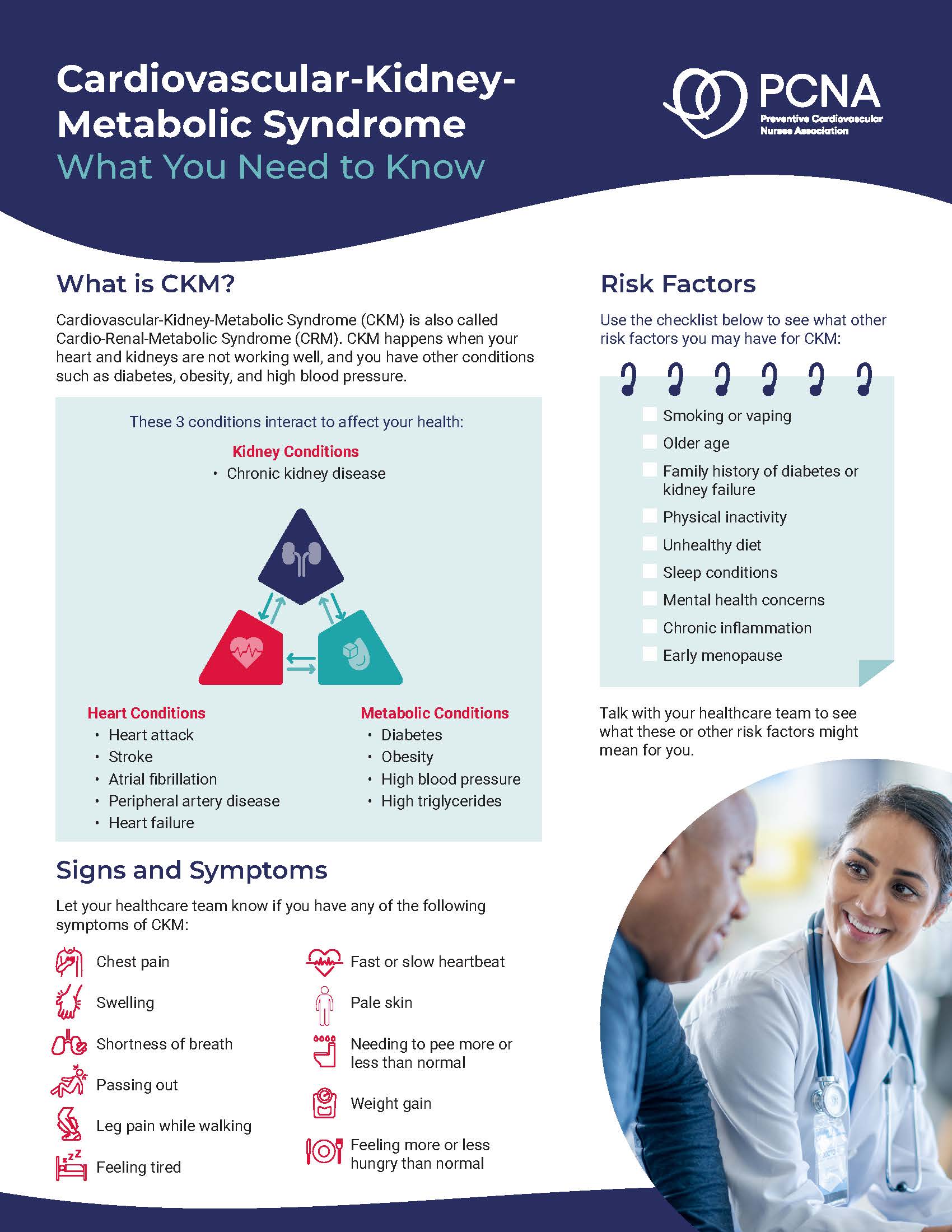
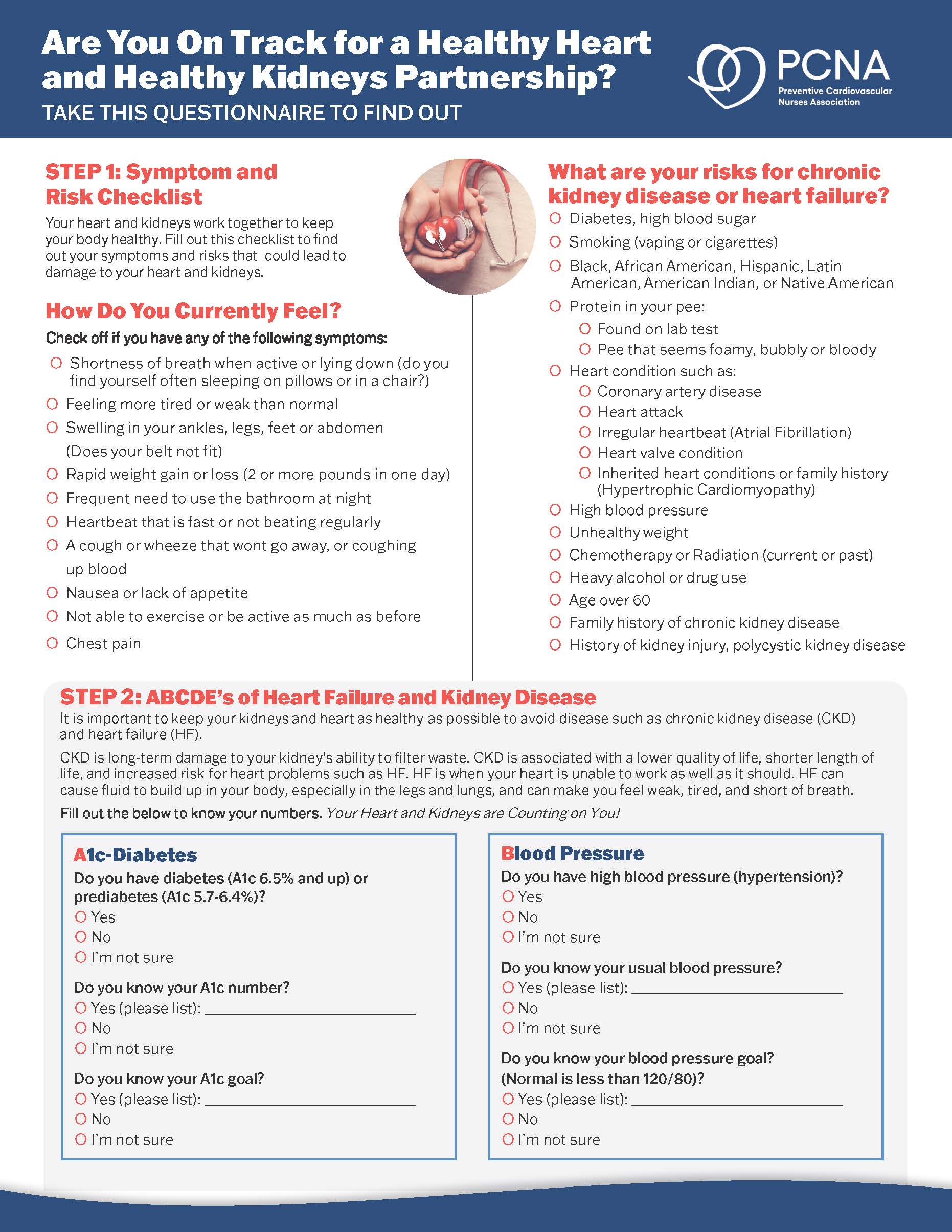
Patient Education Handouts
Cardiovascular-Kidney-Metabolic Syndrome: What You Need to Know
June 26, 2025

Online Interactive Guides
Diabetes and Your Heart: Close Connections Online Interactive Patient Tool
June 12, 2025