An estimated 8.5 million adults over the age of 40 have PAD, yet up to half have no symptoms. Guest Lola Coke, PhD, ACNS-BC, FAHA, FPCNA, FAAN, describes how the disease disproportionately impacts individuals who are Black, Latinx, and Native American, and how clinician awareness can make a positive difference in effective diagnosis and management.
Episode Resources
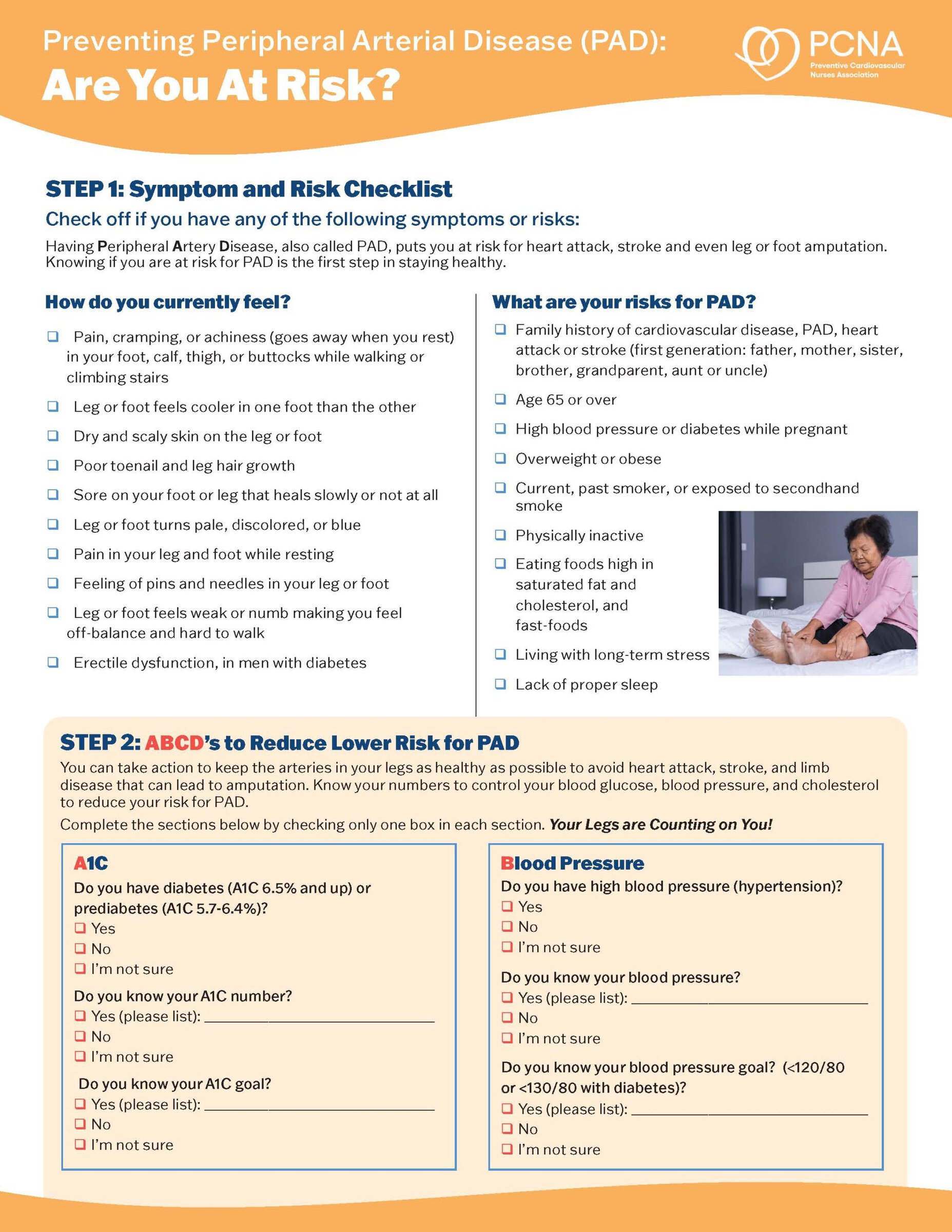
- PAD patient education tool: Step on Up – Peripheral Artery Disease
- PAD Screening Toolkit and Activity Program
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to today’s episode where we are speaking with Dr. Lola Coke. Lola, could you introduce yourself please?
Lola Coke (guest): Yes, I’m Dr. Lola Coke. I’m an Associate Professor and Cardiovascular Clinical Nurse Specialist. And I actually teach at Grand Valley State University and am the Director of Strategic Initiatives there currently.
Geralyn Warfield (host): We have an exceptional expert of this topic that we’re going to discuss today, and that is about peripheral arterial disease, or PAD. And Lola, could you start off telling our audience a little bit about why we should even bother talking about this?
Lola Coke (guest): Sure. Well, PAD is a very passionate topic to my heart. You know, we all know that cardiovascular disease is the number one killer in the United [00:01:00] States. People often only consider their heart, though, when they’re thinking of cardiovascular disease. However, the entire cardiovascular system is intertwined, and individuals need to think about their blood vessel health, too.
Peripheral arterial disease, or PAD, is a cardiovascular disease that affects largely the blood vessels in the lower extremities. Individuals are more likely to know about heart disease and stroke versus PAD, which is why this podcast is so important today.
It is estimated that 8.5 million adults, both men and women, over the age of 40, have PAD, and 20-50% of those have no symptoms.
10 to 35% do experience a symptom: leg fatigue, which is cramping or pain called claudication. But this is simply overlooked often as being deconditioned, or as a normal part of aging in those older [00:02:00] adults. The mortality of the disease is high as well, with the likelihood of death five years after diagnosis.
It really is a silent condition that continues to get worse. Without symptoms. So, we need to educate providers and the public about this disease.
Geralyn Warfield (host): So, one of the other topics that is something that many of our listeners are thinking a lot about anymore is the health disparities that many of our patients face.
And I’m wondering if there are disparities in PAD?
Lola Coke (guest): Absolutely. There’s a lot of work being done across the nation that is addressing the disparities of peripheral arterial disease. The group of people most affected are African Americans. Latinx and Native Americans are also affected too. They’re disproportionately affected, as compared to whites.
We see this geographically as well, across the nation with patients [00:03:00] more likely to have PAD in the South, but also in areas where there’s dense African American or Latina populations or Native American populations, such as on reservations. An example would be Los Angeles County in, in California.
If they’re in a rural area, there’s often limited access to care. And so, in these areas, patients are not able to access care and then they, they sort of suffer in silence, as I, as I said before, it’s the silent killer.
And so, we need to really take a look at those heavily densely populated areas where African Americans and Latinx and Native Americans live.
When diagnosed their PAD has often progressed to ischemic limb disease where there is vessel and muscle damage to the lower extremities caused by blood clots or calcification in the vessels that has obstructed blood flow and it often requires limb amputations. Black [00:04:00] Americans, this is a disparity statistic, are four times more likely to be undertreated and need limb amputations than whites.
Limb amputations create quality of life and immobility issues, and compound an individual’s existing comorbid conditions as these disparate populations are often diabetic and they also have chronic high blood pressure or hypertension.
Geralyn Warfield (host): We’ve been talking about PAD and we’re going to take a quick break.
Geralyn Warfield (host): We’re back with Dr. Lola Coke, speaking about PAD, or peripheral arterial disease. And I understand, like many of our cardiovascular diseases this, this is a progressive disease. And as you’ve stated earlier, oftentimes it goes undiagnosed because there, there’s no symptomology for us to see. There’s nothing that the patient recognizes, or their family member recognizes.
So, what can we do for our patients with PAD?
Lola Coke (guest): So, first of all, early detection is. Is key. And we need to think about not [00:05:00] just cardiologists or neurologists—people who work in the field of cardiovascular disease—but in primary care, family practice, and even in OB-GYN areas where women are seeking their healthcare from those providers. All providers need to approach patients, and learn their social determinants of health, and provide tailored solutions that will minimize PAD if it’s detected.
We need to screen in younger populations, especially those younger than 50 years old. The risk factors for PAD include smoking, high cholesterol, obesity, family history, and presence of those comorbid conditions I mentioned earlier, diabetes and hypertension.
Also, individuals are living longer here in the United States, which also compounds the problem. So, we’re seeing this on really both ends of the life continuum—in younger adults, but also in those older adults.
There’s also emerging [00:06:00] research on the effects of mental health on PAD in individuals that experience chronic stress, and are addicted to drugs or alcohol. That’s where those social determinants become very important. You know, what is their living environment? What are the other, you know, risks that they’re taking in coping with their mental health?
Any patient who smokes needs cessation, cessation strategies to stop. We know that smoking increases the risk of PAD threefold over those who do not smoke.
When you’re seeing your patients, all providers should look at foot examinations. “Take your socks off,” tell your patients, and make sure they understand what good foot care is all about. Making sure they’re wearing good shoes, that they check their feet daily when they wash themselves, or take a shower. If there are wounds that are present, that they take good care of those wounds. See someone to help them with effective wound care.
These are [00:07:00] signs often, without any pain or other symptoms, that tell us circulation, that blood flow is starting to become less. And so, it’s vitally important that patients assume and advocate for themselves by checking their feet.
When a provider sees someone with PAD, a good thorough history and examination, along with, you know, the routine lab work such as lipid profile, blood counts, and other lab tests are important to obtain, as well as obtaining a basic, diagnostic ankle brachial index, or ABI. Not all practices know how to do this, and so, there are materials from PCNA that will show you how to set up an ABI examination and how to obtain those measurements, which are simply blood pressures of the upper extremities and the lower extremities So, they can be done in any clinical setting.
In order to do an ABI, you’d get the Doppler blood, blood pressure on both [00:08:00] arms and legs, and you calculate a ratio based on a higher systolic ankle blood pressure that’s measured in two blood pulse areas, the posterior tibial pulse and the dorsalis pedis pulse, and then you divide it by the higher upper arm pressure.
The lower the value of either the right or the left is the overall ABI. It really is a great way in an office practice to determine the extent of obstruction in the blood vessels. A normal ABI value, just for your reference, is 1.0 to 1.4. If we look at values 0.91 to 0.99, now we’re looking at borderline.
And then as those numbers begin to decrease, it’s considered an abnormal level of obstruction that just continues to worsen. So, for example, 0.71 to 0.90 is mild obstruction; 0.41 to 0.70 is moderate obstruction, and when you get down to no value to [00:09:00] 0.40, now you have a severely obstructed individual. That person’s in trouble, needs immediate referral and needs to be treated for their PAD.
Of course, there are other tests, like duplex vascular ultrasound that they can be sent to, to evaluate the patient and angiographic procedures that help to evaluate the patients more comprehensively, if symptomatic.
After the comprehensive physical and exam is made, making sure that the blood pressure and blood glucose are in good control is vital. Looking at their medications and their ability to obtain their medications, are they taking them on time? Talking to them about the importance of those medications is really, really important.
Working with the patient to plan an exercise program. A home exercise walking program is helping them to get to 30 minutes, at least three to five days a week, and at least for 12 weeks. It has to be sustainable over time.
Evaluate the [00:10:00] what the patient eats and plan for diet modification to help them with weight loss if they’re obese.
And be sure the patient, as I said, is taking their medications, that they can obtain their medications.
And lastly, as I mentioned before, you’re going to hear it a second time, have the patient check their feet daily for signs of reduced blood flow.
Geralyn Warfield (host): So, for our patients who are, for whatever reason, seeing a podiatrist maybe to get their nails trimmed, as an example, is a referral sometimes coming from that location as well as from patients and other providers?
Lola Coke (guest): Yes, absolutely. And I would say that goes both ways—that if you’re seeing a podiatrist, they would make a referral for further evaluation for peripheral arterial disease. If you’re a provider and you see foot issues like fungal nails, overgrown nails, etc., that they really should be referred to a podiatrist. They can really help take better care of those feet and really help monitor [00:11:00] their feet for PAD.
Geralyn Warfield (host): So, we talked earlier about those disparities for many of our patients. So, what can we do to help close the gap in those disparities in PAD specifically?
Lola Coke (guest): Well, first of all, there’s published guidelines on the diagnosis and treatment of PAD. And all providers, not just cardiovascular care providers, but all providers should be knowledgeable about these.
All providers should be aware of those risk factors. They’re really the same as cardiovascular. And so, those widely, you know, disseminated in the public eye as well as all providers should know those risk factors. They include, again, high cholesterol and smoking, but also family history, obesity, and again, those comorbid conditions that I talked about: diabetes and hypertension.
And I bring those up again just because we really need to get the word out that when you have those risk factors, it’s not just your heart. So, don’t worry about just chest pain, [00:12:00] worry about it, but also, worry about those peripheral issues that can lead to peripheral arterial disease.
Statin therapy for high cholesterol has been shown to be effective. However, in Black Americans or in really in disparate populations, only 20% receive statin therapy compared to whites.
Another medication that can be better utilized is anti-platelet therapies. You know, blood clots can be a factor in peripheral arterial disease, So, antiplatelet therapies reduce the risk of those blood clots in the blood vessels.
In the community, campaigns targeting the disparate populations affected by PAD need to be a priority in, in those communities, and we need to work with churches and barbershops and community clinics to make sure that the information is out there for the public. We have found in, in some, some literature that people aren’t even aware what [00:13:00] PAD is.
PCNA has a great toolkit. They have a community event toolkit and they we have a whole selection of PAD materials for patients and providers that can help you to diagnose, and treat, and educate So, we can get the word out and help our patients really understand this disease process.
Smoking cessation was more accessible years ago. Those programs have been largely cut, especially in larger health systems. We need more smoking cessation resources out there for those people. Our disparate populations often are the ones that are continuing to smoke.
There also needs to be reimbursement. This is an advocacy issue for the ABI for clinics and for doctor’s offices, and also, reimbursement for smoking cessation programs. It’s important that we be reimbursed for the time we spend with our patients. So, advocacy toward that reimbursement would be really [00:14:00] important.
Cardiac rehabilitation offers PAD patients rehab, and so, there needs to be better referrals to cardiac rehab for these patients. Again, oftentimes providers don’t even know that cardiac rehabilitation has a PAD program. So, making sure that we educate providers that it’s available, and then continuing to encourage our patients to attend if they are actually referred.
And lastly, to encourage patients to participate in research about PAD, especially women with PAD, so that we can learn more, especially the younger people as well. This disease starts younger. It’s undetected, it’s asymptomatic. So, helping obtain more information about how this, PAD, affects younger people is vitally, vitally needed.
Geralyn Warfield (host): Well, you have provided a lot of information for us to consider and to apply in clinical practice. Is there anything else that you would like to add that we have yet [00:15:00] to discuss?
Lola Coke (guest): You know, I don’t, I don’t think so. From a, from a clinical perspective, again, I would just say we need to care for our patients in a holistic manner. We need to check their feet (OK, that’s time number three). We need to check their feet, but we also, really need to hear their story and understand the whole impact of the social determinants of health on how it impacts them in their whole lifestyle. And then if PAD comes into the picture, how we can most effectively care for them.
Geralyn Warfield (host): Thank you so very much for being willing to talk with us today about PAD. We are just so grateful to you for all that you have done, in the sphere of PAD as well as everything else. We hope our audience has their clinical takeaways so that they can apply right away.
This is Geralyn Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- PAD
Published on
August 15, 2023
Listen on:

PhD, APRN-BC, CNS, FAHA, FPCNA
Related Resources