Advocacy every day makes a difference from the bedside to the halls of Congress. Nurse voices and stories are critical to ensuring that healthcare policies reflect the needs of healthcare professionals and their patients. Guest Ryan Gough discusses current Congressional bills and the importance of engagement in advocacy actions.
Episode Resources
- Safe Step Act
- MINI Act
- Axios: Trust in Health Decisions [Edelman Trust Barometer] April 29, 2024
- PCNA Advocacy Toolkit
- PACH
- Maintaining Investment in New Innovation Act
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): I’d like to welcome our audience today to an episode where we are going to be talking a little bit more about legislative kind of issues, and I’m going to introduce to you very briefly, Ryan. And could you introduce yourself to our audience please?
Ryan Gough (guest): Yeah, sure. I’m Ryan Gough. I’m the Executive Director of the Partnership to Advanced Cardiovascular Health, or PACH for short.
Geralyn Warfield (host): We are a partner organization with PACH on a number of different things. so,today we’re going to have Ryan talk to us a little bit more about policy and access issues related to cardiovascular care.
Ryan Gough (guest): Sure. So, just to kind of level set, the Partnership to Advanced Cardiovascular Health, or PACH, was started in 2016. And we are at 501(c)4, which makes us [00:01:00] an advocacy coalition. And so, we can actually go out and do advocacy, whereas, you know, a lot of nonprofits, (c)3 nonprofits like PCNA, you can only use so much of your time to advocate.
So, what the model really is, is we give a platform for the Preventive Cardiovascular Nurses Association, the American Society for Preventive Cardiology, the Hypertrophic Cardiomyopathy Association, you name it, to advocate and take your perspectives and understanding of what’s going on in the nursing community, and the clinician community, and the patient community, and take that to Congress, take that to state insurance commissioners, take that to state legislators, when there are issues that are impacting access to care for heart patients.
So, our mission is really to, honestly, find the voices of clinicians and patients and put them in the middle of the policy conversation. And I think that, I mean, it’s our belief that, that is [00:02:00] not done enough.
And so, we’re really grateful that PCNA has been such a fantastic partner to us. Anytime we call the PCNA, and I say to Sue [Koob] or the leadership, you know, “I need a nurse that can talk about this issue in this state,” and she says, “We’ve got that person.”
And those testimonies are just incredibly powerful when it comes to advocacy.
So, yeah, happy to talk about some things that we think are kind of top of mind from a policy and access perspective for cardiovascular patients.
So, you know, I would probably, bucket our issue set into two things.
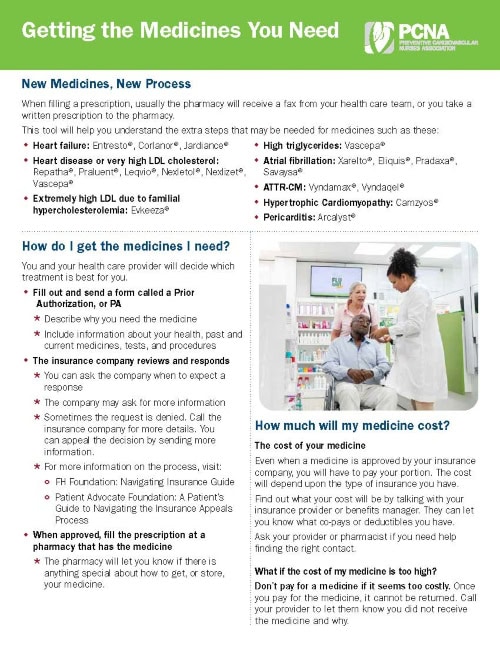
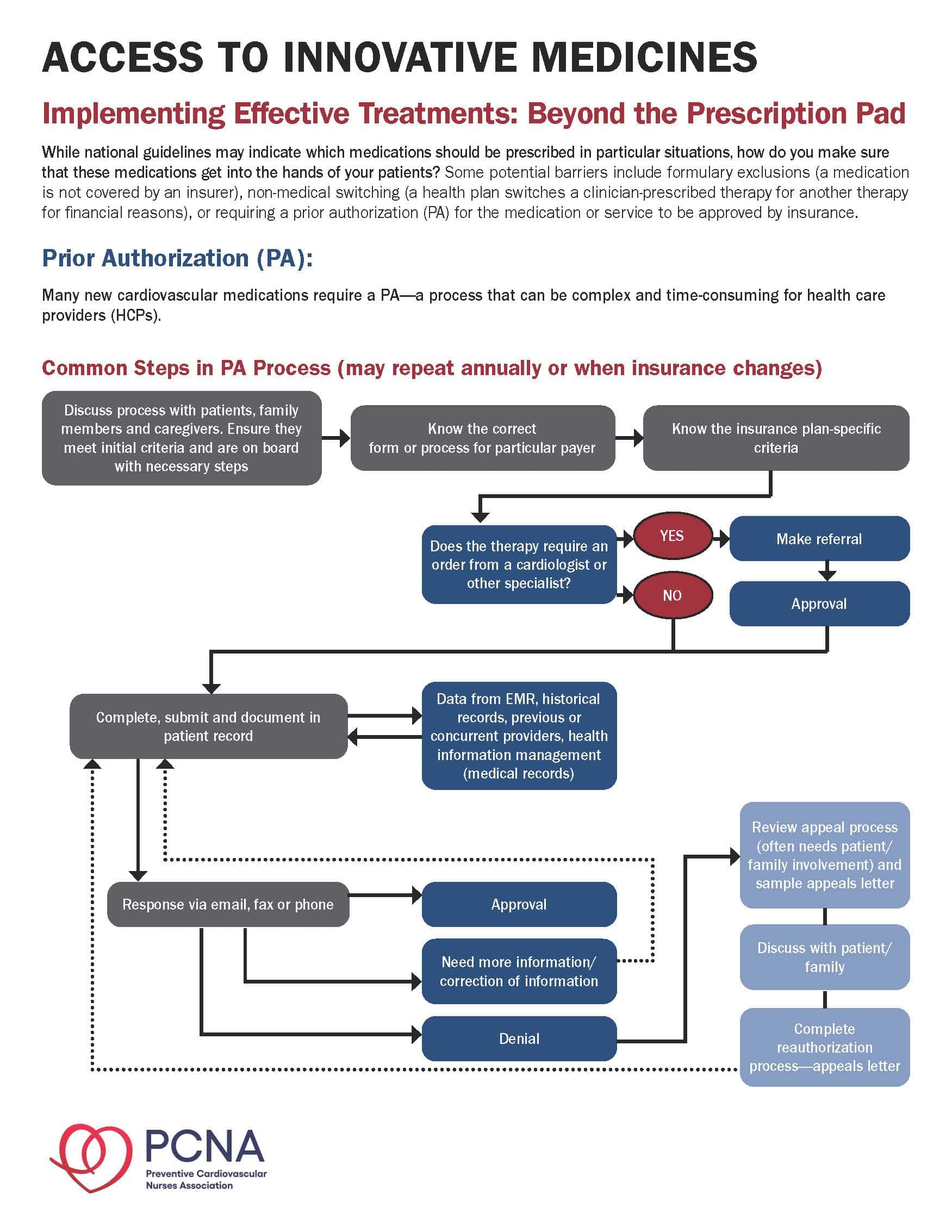
One is utilization management. Because really what we’re talking about when we talk about access to care for heart patients is what’s getting between the patient and the prescriber in the clinic? And a lot of times today, and I’m sure a lot of your listeners would relate to this, that has to do with utilization management. So, when we’re talking UM, we’re talking about prior [00:03:00] authorization policies, non-medical switching, step therapy protocols, copay accumulator programs, and there’s a host of other issues.
And so, it’s important to know that these kind of UM issues, there are regulations around them. Sometimes they’re dealt with on the federal level, sometimes they’re dealt with on the state level.
And so, at PACH, like a lot of national groups, we do follow that in Congress, those kinds of issues. But we are also playing Whack-a-Mole in the states. You know, I think that UM, or utilization management, has become really important in the cardiovascular space, especially in the last 10 years or so, because we’ve just seen an explosion in utilization management. I’m sure that a lot of your listeners would feel that and can have a lot of testimony to that fact.
But whether it be, and really the reason that’s the case is because, after a long period of innovation in cardiovascular [00:04:00] therapeutics, there was kind of a lull. And then we saw, especially with the onset of biologic medicines, and genetically targeted therapies, and some other things, these are expensive, difficult, complicated medications. And as a result, we’ve seen a lot of UM placed on those things.
So, one, on the federal side, what I’ll say, the one policy or a piece of legislation that’s moving now that could ease the burden for prescribers is something called the Safe Step Act. It’s moving through Congress right now. It’s been attached to some larger bills that are trying to deal with pharmacy benefit manager reform more generally.
But basically, what the Safe Step Act is trying to address is step therapy. Or some of your listeners may think of it as ‘fail first.’ And so, what happens here is when a patient comes to a prescriber and they decide that a course of therapy for that patient, they try to get it approved by the insurance company.
The insurance [00:05:00] company comes back and says, “Eh. You need to try this cheaper option or this different option before you can go to the more expensive option. We’re going to step you through that first.” And a lot of times that can be inappropriate.
And then you also have these issues where, you know, a patient’s on one specific health plan, they’ve gone through the step therapy protocol, they’ve failed that initial therapy and then got into the one that their prescriber wanted them on, but then they changed jobs. Or something else happens in their life and they have to move to a different insurance plan. And then that insurance plan steps them through that. And there’s just a whole host of issues with that.
So, the Safe Step Act on the federal level would limit that, those kinds of actions. It creates smoother transitions for patients, like 24-hour kind of appeal periods, making it this electronic so that they can just get through the step faster, that kind of thing. And so, that’s one, on the federal level, [00:06:00] something that’s happened from a utilization management perspective.
Geralyn Warfield (host): So, utilization management obviously impacts not only the patient, but also the healthcare professionals. And we’ve noted over the years how much time a clinic office, for example, might be spending on PAs –on prior authorizations—or this whole process.
Is there a way that, if people are interested in this particular topic or any topic that they could consider being involved to share those voices much like you described earlier?
Ryan Gough (guest): Yeah. You know, prior authorization in particular is a tricky one. And there’s a lot of effort that gets done on the state level around prior authorization. I think the most important thing is sharing your testimony on the burden that this place is on your practice. I mean, we talk to, you know, hundreds of clinicians every year, and one of the [00:07:00] trends that we’ve seen, and your listeners will know this, is that you have now multiple office members, staff members, that are just dealing solely with prior authorizations.
And that takes away time from the patients. It takes away time from the clinician. And it’s just a huge burden on the prescriber. So, there are bills that are moving in states on prior authorization reform.
You know, we track those, and we get those out to PCNA. And what I would just say is that if that’s something that you’re really passionate about, if we flag one, you know, please raise your hand. We’ll put you in front of a hearing, or in front of an insurance commissioner.
And also, it’s really important to know, frankly, it’s really important to know the laws of your state. We have found that in some states, that insurance companies that even though a certain prior authorization reform’s been passed in the legislature, that, you know, plans don’t follow the rules sometimes. And that’s when you get the insurance commissioner involved. [00:08:00] And you know, there are required peer-to-peer assessments that are supposed to happen, things like that. And if that’s not happening, there is recourse.
And you should honestly just get in touch with us, and we can help navigate that for you, so you make sure that, honestly, make sure that your patients are getting what they need, you know now, instead of those delays in care.
So, Geralyn, one fact I think that’s really impactful that shows—I don’t know that I would say that your members and your listeners maybe feel this, but don’t know this—there was a study that was actually done between 2014 and 2020 that looked at 12 different disease states, and the increase of utilization management for these disease states.
And the number one was cardiovascular disease. It saw a 400% increase in utilization management across a number of different therapy classes.
Now that was kind of measured by the number of step therapy protocols and prior authorizations that had kind of been pushed through the system at that [00:09:00] point. But it outpaces every single disease state that they studied, those 12, by like a multiple. It’s incredible. So, this, if you feel this pain, I’m just telling you that it is real. The data bears it out. It’s a huge burden for cardiovascular clinicians and, but there are things we can do about it if we work together.
Geralyn Warfield (host): We’ve been talking about utilization management, or UM, and we will be right back.
Geralyn Warfield (host): We’re back with more discussion about policy issues and we’re here with Ryan Gough from PACH. And Ryan, there’s been a lot of buzz lately about anti-obesity medications, but there have been some struggles along the way and I’m wondering if you could talk from a policy perspective about what you see on the horizon or what’s happening currently.
Ryan Gough (guest): Sure. So, I think the major thing in the anti-obesity space is that, from a policy perspective, there’s been a struggle on Capitol Hill around the Treat and Reduce Obesity Act, or TROA.
And the reason, what [00:10:00] TROA tries to do, is essentially create an avenue so that Medicare Part D can cover these anti-obesity medications. And the reason that that is needed is because when Part D was actually designed, obesity medications were specifically excluded from coverage. And so, as a result of that, there has to actually be legislation that can, has to be passed in order for CMS to be able to cover these.
But since then, as you all, as many of your listeners would know, there’s been some exciting developments in the anti-obesity space. And, in particular, there have been downstream approvals, or additional indications, that have been approved by the FDA.
So, just recently we saw that one of the anti-obesity medications got approval for a cardiovascular benefit. What followed from that, almost immediately, was that CMS said that for cardiovascular benefit they would cover these anti-obesity [00:11:00] medications.
So, I think, honestly, the anti-obesity kind of story in a way, kind of mirrors the PCSK9 story. So, when PCSK9 inhibitors came to the market in the 2015/2016 timeframe, you know, there was a lot of concern among health plans and pharmacy benefit managers that these things were going to flood the market and it was just going to be, everyone was going to be prescribing these and it was going to be like the new statin.
And as a result of that, there was a, I think frankly, an overcorrection from a utilization management standpoint. And almost nobody could get these medications. And that that kind of, the ‘damage’ from that I think has had a long tail, unfortunately. And as a result, I mean there were people that were absolutely appropriate people with, you know, HoFH for instance, that could not get PCSK9 inhibitors.
Anti-obesity medications is somewhat like that. That story is kind of similar in that they have, we [00:12:00] know in an obese population, there’s a high need for these medications. They treat a lot of different comorbidities. There’s, it seems like every day there’s a new study that comes out that shows a new indication or benefit to these medications.
And there’s, as a result, a lot of concern in Congress, at CMS, and at the state level about the hit to the budget, which is normal. I mean that’s reasonable. So, that’s kind of where the tension has been in the last, you know, two or three years.
But I think that from a lot of advocacy, and a lot of education, that people are starting to come around. And they’re realizing that if we get in front of the problem, right, that the downstream effects from obesity, for instance, we can mitigate those.
And the cardiovascular benefit is one of the best examples of that recently.
So, our organization, PACH, actually just put together a letter that we sent to CMS that said, “We’re really grateful that you are covering these [00:13:00] medications for cardiovascular patients. There’s a clear benefit for that. But we also hope that we can get to a place where you’re covering these for all indications for this medication.”
The other thing on the state level I would just mention is that, you know, it’s kind of a patchwork of coverage. There are a few states that Medicaid covers these medications, but one that I would like to point out that’s recent is Mississippi. So, the state of Mississippi, which actually has one of the worst rates of heart disease in the country, recently put the AOMs on formulary, their Medicaid did.
And I think that, I mean, I will tell you from experience that Mississippi is a very restrictive state, and so, that’s very encouraging that the folks there realize the benefit. And I hope that that, you know, bears a good example for the future for a number of other states.
Geralyn Warfield (host): That provides a lot of hope for us, that situations like that can change.
Ryan Gough (guest): Yes.
Geralyn Warfield (host): Over time, but you hit the nail on the head when you, [00:14:00] and it’s what you do every day. It’s that advocacy piece that if the people that are in charge don’t hear from the people that are facing these struggles every day, then the message is lost.
Ryan Gough (guest): And can I speak to that? Because actually there was a poll that came out today that I saw from Axios, and it was looking at trust that people have in different institutions. And it was amazing.
So, basically, the poll was looking at if people trusted government, if they trusted healthcare CEOs, healthcare providers, journalists, you name it.
And the number one entity I guess that people trust, at 83%, was healthcare providers. And I think it was at 30% [35%] was journalists. And just above that was government officials. And just above that was healthcare CEOs—and all those were below 50%.
But the point just being that what you just said, there, is that it is so important for the nurse practitioner, the [00:15:00] nurse, the doctor, you name it, to be involved in these conversations, to help these legislators understand, or these bureaucrats understand, what you’re actually facing in the clinic. Because they don’t know necessarily.
And your voices are the most credible ones in the conversation, frankly.
Geralyn Warfield (host): Well, that’s definitely spurring us to action. And if people have questions about how to get involved. I know PCNA has an advocacy toolkit that can happen. We also have some training and things. Do you offer anything specifically for individuals who are interested in learning about advocacy? Or can you point them towards any other resources?
Ryan Gough (guest): Yeah, I mean, you should come to our website, advancecardiohealth.org. And there you’ll find lots of different materials about really just explaining some of these issues.
I mean, as you can imagine, these policy issues are really complicated. Even I struggle with them at times, trying to understand the ins and outs of the law. And I’m not an attorney. So, we have a lot of kind of explainers on those.
And [00:16:00] also on the utilization management side, lots of videos, and one pagers ,and infographics that just kind of say, this is what prior authorization is, this is what non-medical switching is, and this is why this is happening to you. And then that’s the first piece of this, right, is just education.
And then, if you want to get involved, we’ll find ways to plug in.
Geralyn Warfield (host): Perfect. Before I let this great expert leave the table, there’s one other issue that I’d love for you to address, and that has to be the MINI Act. So, speaking of complex, this is definitely one of those things.
Ryan Gough (guest): Yes. So, the MINI Act is the Maintaining Investment in New Innovation Act, which was introduced—it’s a bipartisan bicameral piece of legislation—that was introduced recently to essentially move a specific subset of medicines on negotiation timeline that was promulgated by the Inflation Reduction Act.
So, let’s back up. As part of the Inflation Reduction Act, which was [00:17:00] passed and signed into law by President Biden, the Centers for Medicare and Medicaid Services basically did a restructure on a couple things.
On the one hand, they did some really positive things. They actually put, for the first time, an out-of-pocket cap for seniors at $2,000, which we think is really good for patients.
And they also put in place something that we call a smoothing mechanism, which means that, if you know that you’re going to hit your out-of-pocket cap on your Part D spend for the year, that you don’t have to pay that up front. You can pay it in installments over the course of the year, which is really good for seniors.
As a part of that law also, though, they—Medicare—set up a system by which they can negotiate drug price, right, which creates some complications. So, first of all, they basically bifurcate medicines into two different categories. You have small molecule medicines, and you have biologic [00:18:00] medicines.
Why this matters to cardiovascular medicine is because most cardiovascular meds are small molecules, right?
And the negotiation timeline is such that the small molecule medicines come earlier, come faster. So, what that is going to do from a pharmaceutical R&D perspective, it frankly disincentivizes small molecule development. And we’ve seen this in a lot of announcements in the oncology space, for instance. Pfizer came out recently and, in the press, said, we’re basically divesting from small molecule oncology development. We’re going fully into biologics now.
We looked at this with a research group out of Washington last year to see, you know, would this law really affect cardiovascular R&D?
And what we found through our research is that number one, as I said, most molecules are for [00:19:00] CV are small molecules. You don’t have a ton of biologic medicines, number one.
Number two, the clinical trials for cardiovascular drugs are massive. Even when you compare them to other chronic diseases, they’re far bigger: more sites, more people, they take much longer.
To make it as simple as possible, what that means, essentially, is that the timeline or the length of time to get a drug to market is like this, but your timeline is really like this.
Geralyn Warfield (host): And by the way, for those of you that are listening only, can you describe that one more time?
Ryan Gough (guest): Yeah. So, the timeline for bringing a drug to market and the expense is really big, but the amount of time that you have to actually make a return on the investment before the negotiation process kicks in is really small.
So as a result of that, you’re going to see, I’m afraid that we’re probably going to see divestment in cardiovascular R&D.
Now, we [00:20:00] mentioned MINI, the MINI Act. The reason that we think that MINI is important is that there’re going to be a number of laws that come through Washington that are going to look at trying to change this negotiation timeline for medications. And we’ll take a look at all of them. But in my mind, the most important one is the MINI Act because there are a number of medications that are these genetically targeted technologies—or GTTs for short—that have cardiovascular, you know, benefit.
A really good example of this are cholesterol meds that are on that list. Lp(a)–those medicines are genetically targeted therapies. There’s also some hypertension medications that are genetically targeted therapies. And so, the fear is that frankly, that if we don’t change this timeline for these kind of new, this new kind of technology, that you’re going to snuff it out.
And so, MINI would essentially [00:21:00] reorganize the incentive structure such that these GTTs can come to market.
And so, for your listeners that are familiar with high Lp(a), I mean, you know there’s a lot of promise there. Hypertension, we all know, is a massive problem. And the really interesting thing about GTTs, about these genetically targeted therapies, is that what they can do is essentially go into a specific strand of RNA and turn off the protein synthesis pathway, right?
So, what that does is it gives you new modalities for treatment. So, instead of having to take a pill every single week or every day, you go in and get your cholesterol shot twice a year, or you get your hypertension shot twice a year. Or you get your Lp(a) shot once a year.
So, from an adherence perspective, I’m sure everyone can understand the benefits there, for instance. And we’re just fearful that if we don’t do something about this, that these kinds of new medicines, which are really the future of therapy we think in a lot of ways, are [00:22:00] going to be snuffed out.
Geralyn Warfield (host): So, we’ve covered a lot of ground today, and hopefully our listeners appreciate that these kinds of topics are very complex, much like cardiovascular disease prevention and treatment, mind you. But what’s a key takeaway that you might have our audience take?
Ryan Gough (guest): You’re right, they are. I hope I haven’t overwhelmed everybody with this. But I will say, the key takeaway I would…or the last thing I’d like to really impress upon your listeners is that, you know, these are complex topics.
But at the end of the day, the most powerful voice is the anecdote coming from the clinician.
You know, we can fill in the gaps on what we’re trying to achieve with these really complicated policies and this, you know, complicated language. But really what makes a difference is the patient and the clinician saying, “This is what we’re seeing in the real world.”
You know, one thing I would say to your audience is, I hate honestly that I’m asking you to add [00:23:00] something to your workload. Because so many of your listeners, you know, did not go to nursing school, or go get their PhD, you know, to go have, feel like they have to go do this kind of advocacy work. But I’m, there’s a big piece of me that thinks that your voices are really needed, and frankly, we are not going to be able to change healthcare to be more patient-centered unless your members speak up.
And so, please reach out to PCNA. Please reach out to us. And if there is an opportunity, we hope that you’ll lend your voice to these issues because if we’re going to really create a patient-centered healthcare system, we need your help.
Geralyn Warfield (host): Ryan Gough, thank you so very much for sharing your time and expertise with us today.
This is Geralyn Warfield, your host, and we will see you next time.
Ryan Gough (guest): Thank you.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Advocacy
Published on
June 4, 2024
Listen on:
Related Resources