Hear from Kim Newlin, MSN, ANP, FPCNA, about some of the newest heart failure medications and guidelines. She will also discuss conversations with patients that should occur early in their diagnosis, and cardiac rehabilitation programs for these patients.
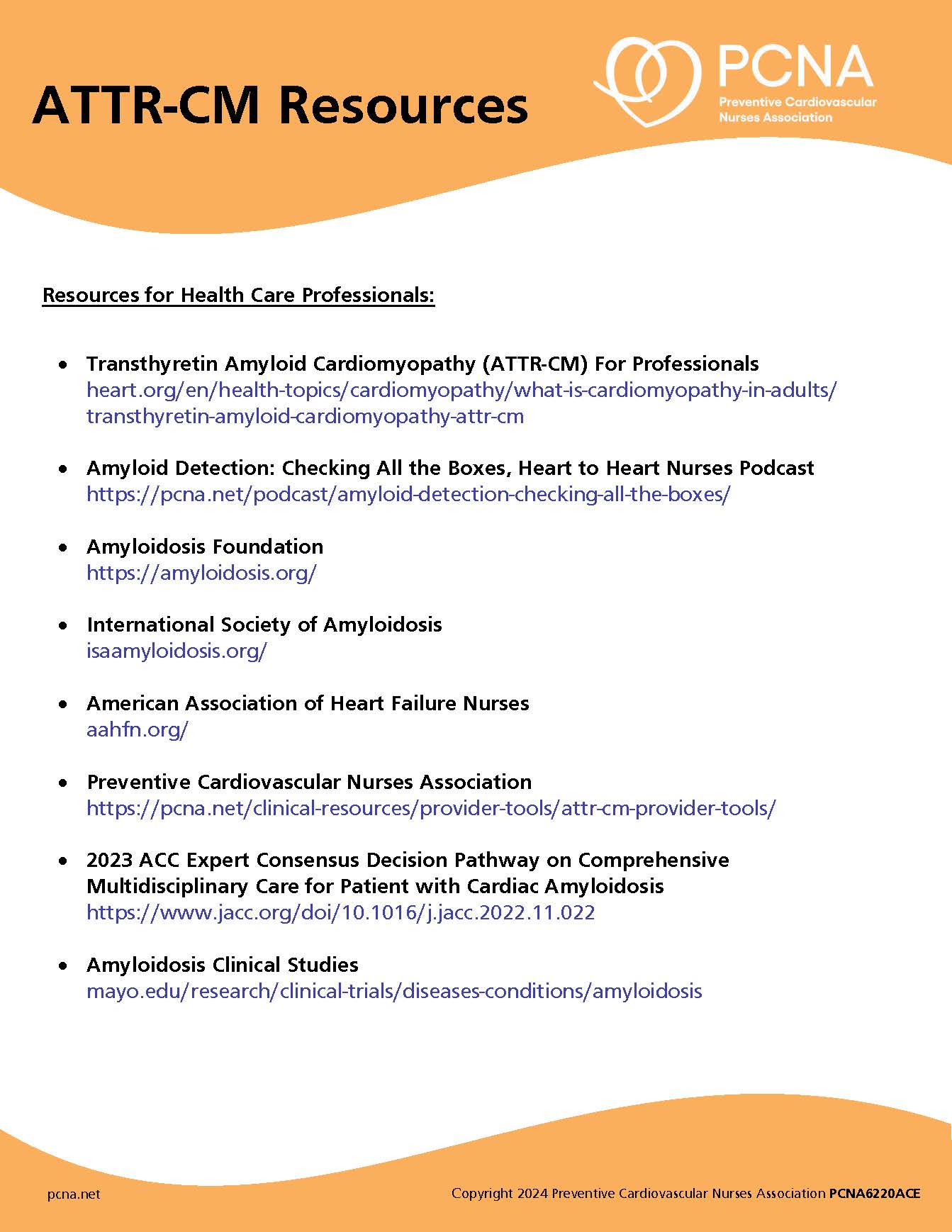
Episode Resources
- PCNA Heart Failure Patient Tools
- PCNA Heart Failure Tools for Health Care Providers
- DAPA-HF Trial
- EMPEROR-Reduced Trial
- CE course Heart Failure: Evidenced-based Pharmacologic Therapies by Kimberly Cuomo, RN, MSN, CRNP, CHFN as part of the 2022 Cardiovascular Nursing Symposium –
- Million Hearts Cardiac Rehab Change Package
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): We are so excited for the opportunity this morning to speak with Kim Newlin and Kim, I’m going to let you introduce yourself, and then we’ll start into our topic, which is heart failure today.
Kim Newlin (guest): Thank you. Thank you for having me this morning. My name’s Kim Newlin. I am a cardiovascular nurse practitioner and clinical nurse specialist with Sutter Health. More specifically, at Sutter Roseville Medical Center in Northern California. I’ve been there 19 years and held a number of positions. Probably my favorite positions right now are I run our transition of care program for high-risk cardiac and pulmonary patients. And within that we have cardiac and pulmonary rehab.
And I also run a clinic for high-risk cardiac patients [00:01:00] coming out of the hospital. It started with heart failure back in 2011, and we’ve added on other high-risk cardiac patients since then. And I have had the opportunity to spend an hour with them after they’ve been hospitalized to really go over medications, treatment options, a lot of the content I’ll actually be discussing today in our podcast. I’ve also had the honor of being a PCNA member for over 20 years and on the board for the last nine years.
Geralyn Warfield (host): Well, we are again, so grateful to you for taking time with us today. So, let’s dive right in and talk a little bit about what’s new in the world of heart failure medications and/or some of the guidelines.
Kim Newlin (guest): Yeah. Excellent. It’s, it’s actually a pretty exciting time for heart failure, which was not the case when I first started. We had a few medications and treatments that we could use back in 2010, 2011, but really, we started to see, about five years ago, in the updated guidelines in 2017, came into the scene were the [00:02:00] ARNIs, or sacubitril-valsartan, and ivabradine or Corlanor®, which, which really added some new treatment options to reduce mortality and morbidity in our heart failure patients.
What’s been great this year and in the last year or so, we now have the addition of the SGLT2 inhibitors. So, the DAPA-HF and the EMPEROR-Reduced trials really proved that the addition of these medications to some of our traditional heart failure medications helps these patients live free from cardiovascular death and reduce their chances of being admitted to the hospital.
So, we had a fantastic speaker at our [Cardiovascular Nursing] symposium this year. Kimberly Cuomo did a fantastic job in providing an overview of the newer guidelines and really what the treatment options are. So, I’ve seen it in the literature called “the fantastic four” which is a, a great description. And that’s really the, the addition of an ARNI, a beta blocker [00:03:00] which has been in our armamentarium for a long time. also, the aldosterone receptor antagonists, and they now [are] adding the SGLT2 inhibitors.
And what we’re seeing is if you use these four drugs, there was an analysis done in 2020, which showed that if you took a 55-year-old patient with heart failure, you use these four drugs. it provided 8.3 years free from cardiovascular death and 6.3 additional years of survival, which is, which are astounding numbers and things we didn’t see with some of our traditional therapies. And that’s when compared to using just our original ACE inhibitor and beta blocker alone.
So that’s, that’s what we’re really looking at now is, we, you know, we originally had the beta blocker and the ACE inhibitor, but we’re adding in or replacing the ACE with an ARNI, really making sure we’re getting in the aldosterone antagonists, which, were sometimes just added in less consistently in the past, and then now the SGLT [00:04:00] two inhibitors. And so, what we’re seeing is if you can add these on early and titrate them up and get them to the highest dose, you’re seeing really good benefit in reduction in heart failure admissions.
And so, before we would sometimes wait or go slower in our titration up, and now the literature and what they’re studying really shows that starting early after the heart failure acute admission and, and working quickly every other week or so to, to get them to the maximum doses is where you’re going to see the best benefit.
Geralyn Warfield (host): So, let me ask a related question. And that is, as you are working as a clinician with these patients, are there strategies that you are using to ensure that the patients understand the application of all four of these medications, because I can imagine that in their mind, they’re thinking, “Oh my goodness, here’s yet something else they’re asking me to take.”
Kim Newlin (guest): Yes. Yeah. And so, it’s, you know, we often add on these medications that seem to be indicated for something else. So, it [00:05:00] adds another layer of complexity.
So, when you look at the beta blocker: originally, you know, people think that’s for heart rate control or blood pressure, but really, it’s to help the heart heal. And now you add in the SGLT2 inhibitors, which really were for diabetes and do help with diabetes, but we’re prescribing it to people who have no diabetes because we know of the improved outcomes.
So, yes, lots of tools and there’s a lot of education needed. I think the, the next trials that people are saying need to be done is how do we add these on and make them affordable for every patient? Because we know our heart failure patients have other medications as well. It’s not just these medications that we’re adding to their list, into their pocketbook.
So, I, I really, and one of the presentations I did here [at the 2022 Cardiovascular Nursing Symposium] was really talking about the importance of health literacy. So, fortunately I have an hour with patients, most people don’t, but where we start is with their understanding of the disease state, as well [00:06:00] as why they have these medications. And that gives me a good kind of, understanding of what they know about the disease, but also what education needs to be provided and information just to make sure they know the importance of staying on these medications. So, us understanding where they are with their understanding, as well as making sure that the education we’re providing is that their level of understanding.
So, the, another important part is using teach-back, which is where you break up the information into chunks. And so, you don’t give a five-minute diatribe of what information they need to know, but you break it up and whether you’re talking about the disease state or the medications, and then you actually have the patient teach it back to you to ensure they understand.
And this is a process where you really put the ownership of, of their understanding on you. So how I usually phrase it is, “I’ve know I’ve said a lot of big words”, or “I know [00:07:00] I’ve given you a lot of information, So to make sure that I’ve done a good job, could you please repeat your understanding of what I’ve shared with you?” And then you just have to give them time and be comfortable with a little bit of silence, but that’s the most effective way I have found, to ensure that they understand.
We also write everything down or provide handouts that have, the information in a clear and easy way to understand and is individualized to them.
You know, something else that we do is, is develop SMART goals. So, SMART goals are goals that are Specific, Measurable, Achievable, Realistic, and Time-based. And so, it’s allowing us to really identify something they want to work on for changing, whether it’s just taking their medications more regularly. or making some changes in diet, or in their physical activity levels. So, there’s a lot of areas of opportunity within heart failure to make some changes. So, using those goals helps provide some specific [00:08:00] information between this visit and maybe the next visit when they come back, and what they can implement.
Another tool that we use is something called shared decision-making, which is a way for us to really, again, make sure that they understand everything around the disease state, but also the treatment options. So, when you get into heart failure, yes, there’s medications and lifestyle changes, but then you’re quickly talking about, do they need a defibrillator? Or do they need, possibly, to be on a transplant list or getting something like a ventricular assist device?
So, we want to start having those discussions really making sure they understand, because if you understand, kind of, what we call the buffet of options. So, when, you know, when you go to a buffet, you know, if you see something really good, you’re going to make a different option or a different choice with, with something on the left side of the buffet versus on the right side of the buffet.
So, it kind of, the same thing is really what are the, all the options that are laid out for you. And that helps with that decision-making process. And there are some great [00:09:00] tools online that we use for shared decision-making, which really take you through the stepwise process and guide the patient through education and understanding risks and benefits as well.
Geralyn Warfield (host): We’ve been talking with Kim Newlin about heart failure, and we’ll be right back.
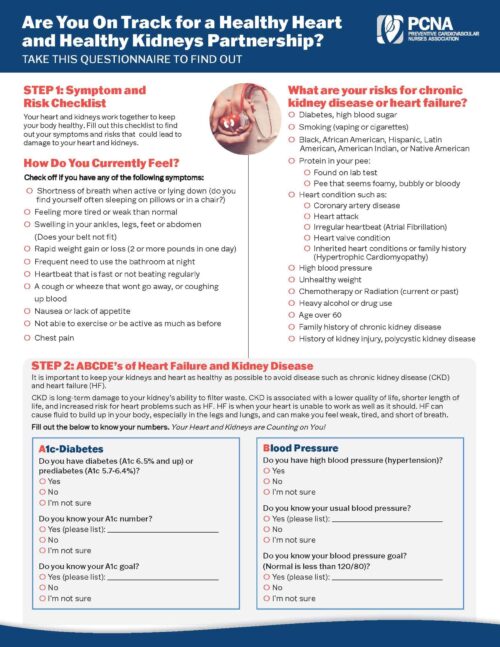
Geralyn Warfield (host): We’re back with Kim Newlin speaking about heart failure, and we know that heart failure can be a complex disease to manage, and it definitely takes a team. And I’m wondering if you could discuss ways to get heart failure patients into cardiac rehab.
Kim Newlin (guest): Yes, this is, this is also a passion project of mine. I have had the good fortune of being part of the Million Hearts Cardiac Rehab Collaborative, whose mission it is, is to increase cardiac rehab referral. So, we know that only about 20% of eligible patients across the country get referred into cardiac rehab and that’s much lower in patients with heart failure, because that’s actually a newer indication that’s covered by Medicare now.
So, this is again for patients who have an ejection fraction equal to, or less [00:10:00] than, 35%. And that’s where Medicare does provide coverage for these patients. So, there are some great ways to get your patients into cardiac rehab, both at an individual and at a system level, a healthcare system level. Those are actually outlined—there’s a great Million Hearts and AACVPR cardiac rehab change package that’s out there, if you’re really interested in finding out more tools and different approaches.
But something that I recommend, and that we’ve tried to do within our Sutter Health system where we have eight cardiac rehab programs, is really making sure that the ordering clinicians know about who qualifies. So, when heart failure came on board several years ago, it took us a while just for that information to get out to the ordering clinicians that these patients would qualify and benefit.
We, and a few other of our Sutter Health cardiac rehab programs, and I know across the country, many did, was make sure they really were prepared to take these patients. Their [00:11:00] energy level’s different than maybe your type A cardiac or acute AMI patients. So, the, the exercise programs just need to tailor them to these individuals.
And the education’s a little bit different, too, talking to someone who has heart failure versus not having heart failure.
So, we also just had to make sure we knew which programs were in our community. So, knowing where we could refer, if somebody came into our hospital who didn’t live in a near-geographic proximity, we could make sure that they had a referral to a program, maybe up the hill, or in closer to where they live to ensure they would go. So, partnering with those programs in the community, that maybe were not part of our health system and being able to really give those patients the right information, so, they could then get connected. The last thing we want to do is give them outdated phone numbers or give those patients information about programs that don’t exist.
And really, I think an important part is talking to the patients about the [00:12:00] benefits of cardiac rehab and that’s all part of that shared decision-making. So, yes, there’s medications—super important—but the benefit of physical activity and the, the ability of physical activity through cardiac rehab to actually improve that ejection fraction, and help them feel better, and be able to do the things that they want to do, is, is really important because it is a commitment, if it’s two to three days a week, they have to get up and get dressed and get there. And, and that’s a little bit daunting to people who have a new diagnosis, as well.
Geralyn Warfield (host): Are there any other resources that you didn’t mention already that you would like to share with our audience?
Kim Newlin (guest): Yeah. So of course, PCNA has a great heart failure education packet, and includes even a stoplight tool, which you can use with your patients, which helps, those individuals try to make sure they catch symptoms that are developing early on, so, they’re not so sick that they have to go to the hospital.
I also think it’s really important to try to [00:13:00] explain the term heart failure. So, it is probably one of the least favorites terms in our medical community. But I think it’s really important for patients to know that their heart is not failing and that it’s not an inevitable downward trajectory and that there are options and opportunity for that hearts to be healed.
So, we actually changed the name of our heart failure clinic to the heart health clinic. We found that patients literally would not show up because failure was in the name. But I think it’s, I think it’s probably the first place you need to start, because they’re told they have heart failure and then there’s often an overwhelming sense of doom and that there’s nothing they can do. So, an important part in, in education and early education about what heart failure means and what it doesn’t mean.
Geralyn Warfield (host): I can only imagine what it’s like for our patients who hear that for the first time. So, I really appreciate the fact of the renaming of the center into heart health, which is what we are all about.
We’ve been talking with Kim Newlin about heart failure. [00:14:00] I am your host Geralyn Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more
Topics
- Heart Failure
Published on
November 29, 2022
Listen on:

ANP-C, CNS, RN, FPCNA
Related Resources