Cardiovascular-Kidney-Metabolic (CKM) Syndrome leads to poor health outcomes and is affecting individuals at younger and younger ages. The PREVENT calculator helps identify individuals earlier in the disease progression, allowing time for interventions that may lead to a regression of the stages of CKM. Guest Chiadi Ndumele, MD, PhD, also describes shared decision-making, and value- and volume-based care models.
Episode Resources
[00:00:00] I’m Erin Ferranti, board president for PCNA, and I’d like to welcome you to this episode of the Heart to Heart Nurses Podcast. PCNA is the proud home of cardiovascular nurses and one of the leading figures in the fight against cardiovascular disease. We have the resources you need for your day-to-day practice or to follow your passion to new areas of learning and growth.
Geralyn Warfield (host): (00:20)
I’d like to welcome our audience to today’s episode where we’re talking with Chiadi Ndumele. Chiadi, could you introduce yourself to us?
Chiadi Ndumele (guest): (00:26)
Of course. Thank you so much for having me.
So, I’m Chadi Ndumele. I am an Associate Professor of Medicine and Epidemiology at Johns Hopkins University. I’m a cardiologist as well as an epidemiologist. And I also direct obesity and cardiometabolic research there. And I was very excited to be here [at the 2025 PCNA Cardiovascular Nursing Symposium] today to speak about cardiovascular kidney metabolic syndrome and how we need to be thinking about that in clinical care.
Geralyn Warfield (host): (00:53)
Well, I know that you have been speaking at today’s [April 2025] PCNA Cardiovascular Nursing Symposium, and it was actually kind of tough to get him away from the audience because they had a lot of questions for you after the presentation. So, we’re so excited that we can share your expertise with our podcast audience as well.
So, could you please describe for us what CKM is and why we really should care about it?
Chiadi Ndumele (guest): (01:08)
Yeah, think it’s a really good question and it really, first of all, reflects where our society is going from a public health and a clinical standpoint.
I would say historically, when we think about cardiovascular prevention, we focused a lot on cholesterol—appropriately We think about high blood pressure—appropriately. Smoking. And those have been very, very important and we’ve made a lot of gains over time from that emphasis.
What we’ve seen over the last few decades, last 2 to 3 decades in particular, 3 decades, is a striking rise in the proportion of individuals for whom conditions like obesity, and diabetes, and chronic kidney disease, are their primary determinant of cardiovascular risk.
It doesn’t mean that high blood pressure, and high cholesterol, and smoking are not important, but we’re seeing those as the isolated factors kind of diminishing over time. And we see a rise in these other conditions.
So, that just means we’re ending up seeing these more complex patients with this multiplex of very interrelated conditions that are driving cardiovascular risk.
Now the reason we really need to care about this is because this leads to premature mortality. So, when we see these conditions occurring by themselves, but even more so when they occur together, we see a big impact on cardiovascular mortality.
And we also see this kind of born disproportionately in the population. We see this among people with more adverse social determinants of health. We’re seeing the pipeline of CKM syndrome substantial among our youth because we see historic levels of overweight, obesity, and diabetes in those populations as well.
So, we describe CKM syndrome, the American Heart Association put out a Presidential Advisory and a Scientific Statement on this in fall of 2023, describing it as a health disorder reflecting these connections among diabetes, kidney disease, obesity, and cardiovascular disease that leads to poor health outcomes.
And we describe this along a spectrum. So, there’s some individuals who are in the spectrum because they have these risk factors and are at risk for developing cardiovascular disease. But there’s also individuals who have existing cardiovascular disease, who have obesity and diabetes and chronic kidney disease and hypertension, where we need to make these other considerations and how we approach their care to kind of optimize their outcomes.
So that’s kind of what it is and really more and more of why we should care.
And there’s just a lot of unique challenges that are represented by having patients now with multi-system disease in terms of things like fragmented care, and seeing multiple providers, and challenges with navigating that. Highlight the underpinnings of social determinants and you know how intensely related to all these conditions and their complications that is.
But as I’m sure we’ll get into, we also have a lot of opportunity now. So, we also know that we understand this interplay, we understand it’s not a coincidence when we see our patient with obesity, diabetes, kidney disease, and heart failure, like there’s a reason for that. It’s all interrelated. And we have more and more tools in our arsenal to actually address those.
Geralyn Warfield (host): (04:38)
So, you really capably described what this syndrome is, how it affects individuals. Does it have its underpinnings in inflammatory responses to all of these diseases?
Chiadi Ndumele (guest): (04:51)
Yeah, so that’s a very good question and it’s central to what we should be thinking about here.
So first, it’s important to kind of acknowledge that the underpinnings of so much of this are excessive dysfunctional adipose tissue. So that rise in overweight, obesity, and the kind of downstream consequence of this, are really a lot of what’s responsible for this interplay.
The primary mechanisms that lead to all of this multi-system compromise actually starts with inflammation and insulin resistance. Those two things are very closely interrelated. Oxidative stress kind of goes along with that. And there’s a lot of kind of microvascular and macrovascular dysfunction that’s part of that. All these things really contribute to these multi-system challenges we’re seeing.
So, inflammation is very important if you look at inflammatory markers, things like cytokines, acute phase reactants, even adipokines that are released from adipocytes, and inflammatory cells in adipose tissue, those are kind of key predictors and determinants and drivers of what’s happening from that standpoint.
In the CKM syndrome construct, and we could talk about the staging in a little bit, but we do think about what’s enhancing your risk along this, we talk about risk enhancing factors, and among them, inflammatory markers, or having a chronic inflammatory condition, are kind of key measures that we think about from that standpoint.
Geralyn Warfield (host): (06:27)
So, let’s talk a little bit about that progression of disease, or progression of the syndrome. And like many activities that we see people being involved in, this is not necessarily linear. It can regress, it can move forward at different paces. Could you talk a little bit about that, what that looks like?
Chiadi Ndumele (guest): (06:45)
So, I mean what we’ve done is take a very—and I was part of, the chair of, the science advisory group that developed the staging framework—we took a very complex thing that could have risk in multiple different axes and dimensions and we’ve kind of put it on one kind of continuum.
So, some aspects of that are artificial but I think clinically useful for how we kind of conceptualize this. And it does reflect how people typically progress. So you’re absolutely right.
So there’s a spectrum that we reflect in there.
And it starts with stage 0 which is not actually part of CKM syndrome, is those individuals who don’t have these risk factors and are at ideal cardiovascular health. And we want to keep them in that area as long as possible so we want to pay attention to that and also be looking for the emergence of these risk factors at some intervals.
Stage 1 is people who have excess and/or dysfunctional adipose tissue, so that’s really reflecting people who have overweight or obesity, excess abdominal waist circumference.
But there are also individuals, there’s a subset of individuals who start to develop inflammation and insulin resistance even in the absence of overt high weight. So, we want to reflect those individuals as well. And we look for impaired glucose tolerance in people even with some normal weight would be meeting that criteria.
Stage 2 is the metabolic risk factors that are often downstream of the excess and dysfunctional adipose tissue: hypertension, diabetes, hypertriglyceridemia, and then also chronic kidney disease at moderate- to high-risk levels, which we know is so interrelated to that.
And then stage 3 is people with subclinical cardiovascular disease, either subclinical heart failure, subclinical atherosclerotic cardiovascular disease, or risk equivalents.
So, we’ve dveloped a new risk calculator as part of this, that’s called the PREVENT calculator. So high predicted risk with that is kind of a risk equivalent for subclinical cardiovascular disease. And then similarly, individuals who have very high-risk chronic kidney disease are also at similarly high risk.
That’s just important because those are the individuals who are really the most, have the most impending risk of progressing to stage 4, which is clinical cardiovascular disease. So having things like heart failure, or stroke, or coronary artery disease, as well as AFib and, peripheral artery disease, overlapping with metabolic risk factors and/or chronic kidney disease.
And you’re absolutely right. I think there’s a few things that can happen with this. A lot of these conditions go unrecognized at the earlier stages, so we can actually get a more systematic identification of these conditions, support prevention along that spectrum to prevent progression to worsening stages, to importantly, promote regression.
So, I think for patients, particularly with subclinical heart dysfunction or metabolic risk factors or early chronic kidney disease and excess weight, we can actually go backwards in terms of these stages with our substantial lifestyle change, substantial weight loss. So that’s an important piece there as well. So, you don’t have to just move in one direction. We can be trying to promote moving backwards.
And then fourth, I think the people who have the highest risk, that stage 3 population, that stage 4 population, we’re going to want to recognize that, think about, holistically, the factors that are contributing to their risk, and then basically treat them most aggressively because they’re the ones at the greatest risk of adverse outcomes.
Geralyn Warfield (host): (10:18)
I appreciate you discussing for us that progression and potential regression that we can have. And you spoke earlier about the fragmentation of care that many of our patients have. Are there ICD codes for this? Are there ways for us to communicate about this more effectively?
Chiadi Ndumele (guest): (10:33)
Coming. So not yet. So, there’s been a hint, the American Heart Association’s announced that in spring of 2026, there’ll be guidelines that will come out for CKM syndrome. So that process is usually kind of the precursor to getting to ICD codes and billing codes that reflect the classes of recommendations that are put out. But I anticipate these kind of stages will be something that could be considered in the future.
And then I think integrating that into our care models is going to be a key part of what we’re going to be doing.
And I think communicating, just like we communicate the stages for some other conditions, here this will have particular relevance. It doesn’t obviate the ability to say, OK, they also have specifically type 2 diabetes with this complication, or they have specifically hypertension. But to recognize that they’re in this stage of this progression, I think is an important part of care discussions with our patients and also for communication across the care team.
Geralyn Warfield (host): (11:38)
We’re going to take a quick break and we will be right back.
Geralyn Warfield (host):
We are back for our discussion on CKM syndrome. One of the things I think we probably could let our audience know a little bit more about is that PREVENT risk calculator. Could you discuss that a little bit more?
Chiadi Ndumele (guest): (11:51)
Thank you for that. We’ve had, risk-based prevention has been an important part of our clinical approach for some time now. We’ve had the pooled cohort equation that’s focused on 10-year risk for atherosclerotic cardiovascular disease. It’s been a very useful tool as we think about that risk.
As we’ve kind of gotten to the CKM syndrome population, there’s a recognition that we had some additional needs. So, first of all, we need to think about not just risk for atherosclerotic cardiovascular disease, but heart failure is a major challenge related to CKM syndrome that’s on the rise and we need to be thinking about risk for that. And put them together in terms of total cardiovascular disease.
So, PREVENT now has actually three outputs: atherosclerotic cardiovascular disease, heart failure, and total cardiovascular disease, the composite of the two of those.
Geralyn Warfield (host): (12:45)
So, you would use this PREVENT tool in lieu of that 10-year ASCVD tool, or would you use them in tandem?
Chiadi Ndumele (guest): (12:51)
Right now, in tandem, because right now the pooled cohort equation is what’s in our clinical guidelines.
But as I mentioned, there’s going to be a new CKM guideline in 2026. There’s also been discussion that there’s going to be a new cholesterol guideline in spring 2026. And there’s also an announcement of a new hypertension guideline coming out later this year [Now available; Aug 2025].
We’ll see what those guidelines do. But if they then put this as a front and center tool, then I think it’ll be make it easier for us to say, we can harmonize that with actual use of this in clinical practice.
So, I think right now it’s a really good way for addressing and estimating risk and discussing risk with our patients.
The other thing that is helpful with the PREVENT update is that it has started predicting risk earlier.
So, we’re seeing earlier and earlier cardiovascular disease. So, now instead of starting at age 40, it starts at age 30. So, 30 to 79. And it looks at not just 10-year risk, but also 30-year risk, which is going to be more relevant for some of our young adults to kind of help understand their longer-term risk based on their risk profile. It actually, and it has some of these CKM syndrome components like hemoglobin A1C, kidney function measures, BMI, with regards to heart failure in the model, so I think that’s helpful as well.
And then finally, it includes a measure of, so it doesn’t include race, but it includes social deprivation index, a measure of social determinants, in the model. And what we’ve seen is that its performance, which is the reason why there was a concern about needing different race-based equations previously, its performance actually works quite well amongst Blacks and whites and Asians and Latinos, so we see good performance across all those groups.
We used to actually see about a two-fold over-prediction with the pooled cohort equation. So, the predicted twice as great as the observed risk. Here we’re seeing a pretty one-to-one in terms of reserved predicted.
So, this I think will end up being an important tool as we think about these new therapies that we have on the horizon, and how we’re going to deploy them to best address people who are at risk for dverse events.
Geralyn Warfield (host): (14:59)
I’m very excited that we’ve had the opportunity to talk about what CKM syndrome is, how it applies to patients of every age basically, how we can move ahead in our prediction for that.
But I think one of the things that our audience probably is most interested in is how this looks in practice. How can we help with care? What can I do tomorrow, after listening to this podcast while I’m walking the dog or doing whatever it is I’m doing? How does that apply? What can I do to make things better for my patients?
Chiadi Ndumele (guest): (15:27)
Yeah, it’s a very good question. And I think, so I will say first of all, the staging and the risk estimation is a good place to start the conversation. Just to kind of help people better understand the spectrum of risk and motivate this concept of optimizing life course prevention, supporting regression for better overall health and outcomes.
So, I think that that’s a good starting point.
I think we have a couple of overarching themes within the care model. So, one is addressing social determinants of health. So that’s basically systematic screening using validated tools for adverse social determinants.
And then, part of the CKM care model will be actually having people on the care team integrating this into our EHRs. but then having people on the care team who can help address these and actually connect people to existing community programs and community resources. To really support all the things that just are central to self-care accessing healthcare, getting to appointments, understanding what you’re taking, getting support for having the lights on in your house, so you can actually do the things that are related to your health. Some of the basics that are really fundamental here.
The second piece is interdisciplinary care. And that’s related to the care fragmentation. That’s so
important here because people have multiple different conditions. They’re often seeing multiple different providers, nurses, maybe a pharmacist, certainly multiple different kinds of doctors and specialists. That can be really hard to navigate and sometimes they’re not all on the same page and sometimes they have a silent approach where things fall through the cracks.
So, we need more coordination.
And there’s two approaches that we talk about. Both of them hinge on what we call CKM coordinators. And the CKM coordinators are likely going to end up being mostly nurses and pharmacists who will play like a central linchpin role in terms of bringing things together. We see this has worked in research studies and we want to implement this in clinical practice.
So, we talk about a value-based model where it’s a more remote interdisciplinary care team support to say, hey, we have a local protocol. We’re here to kind of back up and support, but there’s a protocol we follow for patients where we see confluence of these factors to make sure we’re optimizing their GDMT with support of the CKM coordinators who are helping primary care, supporting that kind of process for patients. So that’s one piece.
Then we talk about a volume-based model, where we’re actually referring patients to subspecialists who are high risk—the A1C of 10, and they’d be seeing an endocrinologist or having existing cardiovascular disease, and you’d see a cardiologist, a high-risk cardiac kidney disease. And that’s good, but we want to basically help patients navigate across that, and understand, and have kind of shared messages across that. So that’s where the CKM coordinator can play a role from that standpoint.
And there’s a recognition that some places will be able to do more value-based, some places will be able to do more volume-based, depending on their density of subspecialists, how they practice, but we want to kind of start putting things in place that reduce some of that care fragmentation.
I just gave this talk and there was a big question about cardiometabolic care models and clinics, these coordinated clinics. I think those are great. We have one at Hopkins, there’s some at other places. They’re a bit more of an investment for health systems, so we’ll see if that’s place people go, but I think for your high-risk patient that has diabetes and kidney disease and cardiovascular disease, and getting hospitalized multiple times a year. Having a model for some places where they can get that shared, coordinated care in a clinic visit is also very attractive. But that’s a little bit more complicated in terms of reimbursements and infrastructure and everything else. So, I think that’s important.
The other piece of this is the kind of what we can do in terms of the medical aspects of our care as well. And I think there’s really two different strategies to consider. Strategy number 1 is to basically support lifestyle change and target goals for our blood pressure, our diabetes, our lipids, our addressing of chronic kidney disease.
And we see there’s an old trial called the Steno-2 trial that showed really dramatic benefits of—this was is before all the fancy drugs were out. Dramatic benefits for cardiovascular rates, and for mortality, with taking that approach in patients with overweight, obesity, diabetes, and albuminuria. So, we know for that CKM population that targeting—just supporting lifestyle, supporting risk factor control, getting things to goal, can be very helpful.
But we also have a bunch of really exciting therapies. And those CKM therapies are pretty interesting because many of them impact multiple different axes of these at the same time.
So, for example, SGLT2 inhibitors improve kidney outcomes, heart failure outcomes, cardiovascular mortality, and they have modest glycemic benefits. Finerenone is known to be beneficial in diabetic kidney disease and also improves heart failure outcomes as well, some of that related to improving kidney disease events.
And then, the GLP-1 receptor agonists like semaglutide and tirzepatide, and some of the older agents like liraglutide, we see benefits on everything. We see benefits on weight, metabolic risk factors, glycemia, blood pressure, inflammation. We see that recently there was something called a trial called the FLOW Trial that showed benefits on chronic kidney disease, and also mortality in that population. We see cardiovascular events, cardiovascular mortality improved. And the data suggests that the benefits are not all weight-dependent, so we see actually earlier benefits even before we achieve substantial weight loss. So, CKM benefits for those agents as well.
So, I think one of things we want to think about is how we optimally deploy these different therapies, but I think there’s a bunch of different strategies. The key here is that we need systems that support coordinated holistic care, and that we need to be thinking about all of these different, interrelated conditions as we’re basically optimizing both prevention and management for our patients.
Geralyn Warfield (host): (21:34)
The other thing that I think will help benefit the patients is that shared decision-making model that we all are trying to do, in very limited amount of time that we have with them. But I think if they feel empowered in each situation that they might be meeting with their endocrinologist, their cardiologist, maybe the nurse who’s talking about diabetes education, whatever that is, I think that repetition of information from an educational standpoint is really important. If you hear from one provider, you might think about it, but if more than one provider is talking about it, I think that’s much more impactful.
Chiadi Ndumele (guest): (22:06)
I think that’s absolutely the case. I think that first of all, you’re touching on several very important pieces.
One is that we actually need to be reading from the same playbook. So, it needs to not be a diabetes playbook or an endocrinology playbook and a nephrology playbook and a cardiology playbook. We need a common playbook. So, I’m hopeful that some of the efforts that are ongoing will get us closer to that so that we have kind of, we’re all on the same page in terms of the messages we’re giving to patients.
I do think the education piece is important. I think that activation is really important. I think some of that can come through public health efforts and kind of campaigns.
I think also some of that really can come through nurses and this kind of CKM coordinator role as well.
And basically, kind of providing that understanding, like this is what we’re talking about. This is why this is important. And what is, what are your goals? What is it that’s going to matter to you? Is it your quality of life? Is it preventing events? Is it the longevity? Is it just being at home and functional?
And so, kind of understanding, as you said, that shared decision-making model, having that activation, I think that’s going to be a really key goal here.
There’s a bunch of, if you’d like, I could tell a little bit, there’s some longer-term efforts going on for this. I’ll say two things. Number one, as part of the CKM initiative, there is actually a patient advisory group that’s kind of actually alongside, and patients who have these conditions and talking about it from the standpoint of what do we need to see, and hear, and what do we understand from the messages? And what are our priorities?
And I think that that’s really important for informing the overall efforts.
There’s also a broader group that’s providing strategic guidance about how we can implement this into care models, and payers, and health systems, and think about that as well.
And then within the broader science group, there is going to be a big focus on implementation of this care model. So, the AHA has announced a four-year initiative for CKM health implementation across 150 health centers and 15 markets over four years that will basically be trying to apply these care models in the clinical practice there with a focus on getting people certified in CKM health centers. And then also becoming centers of excellence in CKM health.
But that will take starting to do some of these things that we’re talking about to bring people together from a holistic care standpoint, address social determinants, and also start to apply these different therapeutic approaches.
Geralyn Warfield (host): (24:36)
Well, it sounds like a very exciting time to be involved in cardiovascular prevention and management at this time. If you had one key takeaway that you would like to leave with our audience, what would that be?
Chiadi Ndumele (guest): (24:47)
I think the key takeaway is that cardiovascular disease prevention has become more than a single risk factor issue and has become a bit more complex. However, even though that complexity is what’s in front of us, I think we have tools to make more optimal prevention and more optimal management accessible for all of us despite that complexity.
I think it’s the public health challenge of our time moving forward, but I think that partnering together, we can make some really substantial progress.
Geralyn Warfield (host): (25:24)
No one could say it any better than that. Thank you so very much for being with us today.
Chiadi Ndumele (guest): (25:28)
Thank you for having me.
Geralyn Warfield (host):
This is Geralyn Warfield your host, and we will see you next time
Thank you for listening to Heart to Heart Nurses. Visit PCNA.net for clinical resources, continuing education, and much more.
Topics
- Atherosclerotic Cardiovascular Disease (ASCVD)
- Diabetes
- Kidney Disease
- Obesity Management
- Pharmacology
- Risk Assessment and Management
Published on
December 16, 2025
Listen on:
MD, PhD, MHS
Related Resources
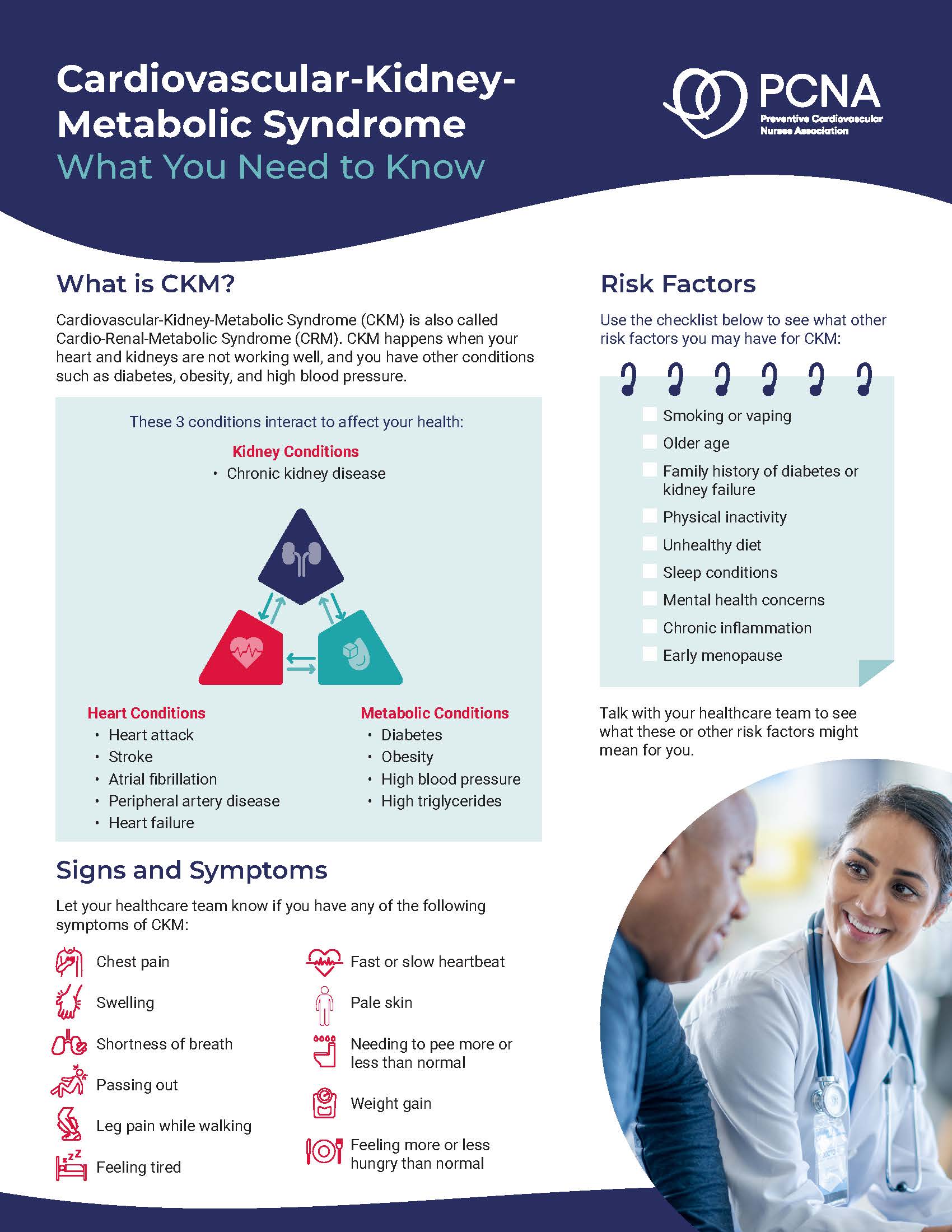
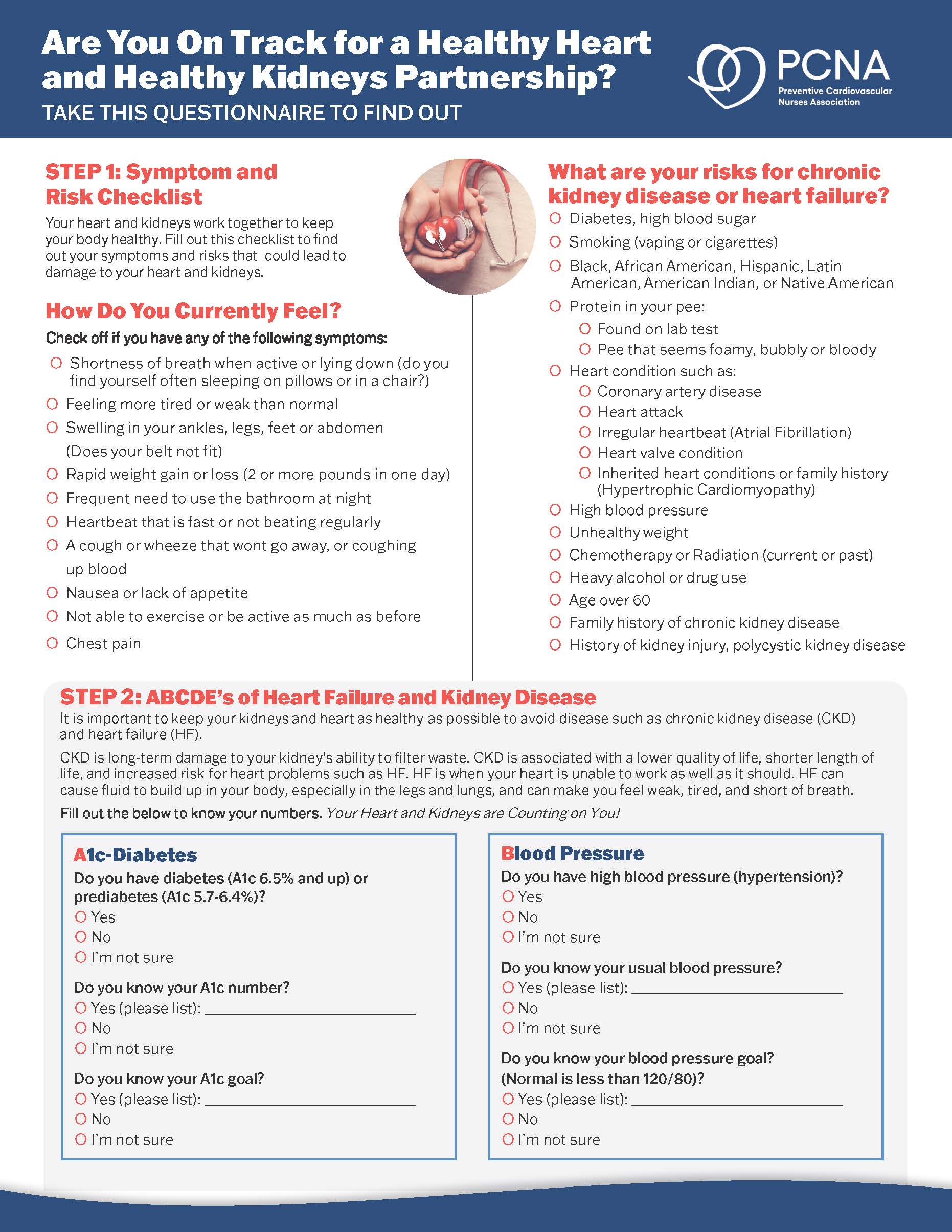
Patient Education Handouts
Cardiovascular-Kidney-Metabolic Syndrome: What You Need to Know
June 26, 2025