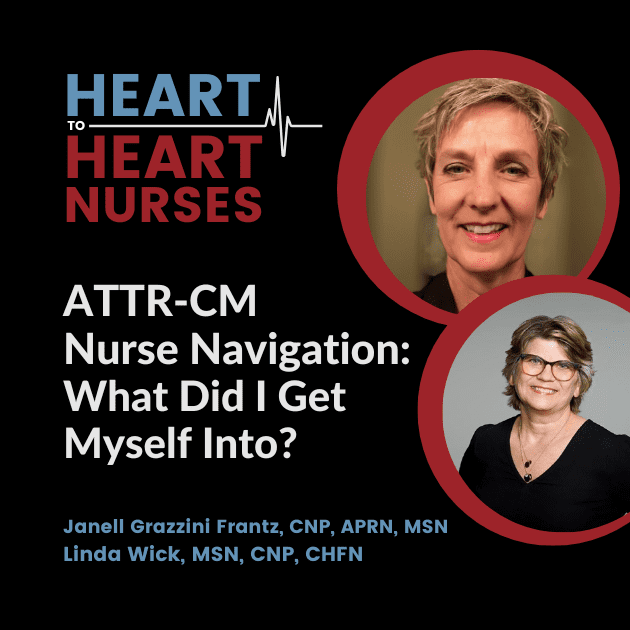
Learn about ATTR-CM symptoms and diagnostics, team-based care and specialists, and the importance of the nurse navigator role (even if that isn’t your specific job title). Guests Janell Grazzini Frantz, CNP, APRN, MSN, and Linda Wick, MSN, CNP, CHFN, chat with moderator Kim Newlin, MSN, ANP, FPCNA for this ATTR-CM Nurse Navigation podcast episode.
This podcast episode is supported by independent educational grants from Pfizer, Inc.
Episode Resources
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management
Moderator: Kim Newlin
[00:00:16] Welcome. I’m your moderator, Kim Newlin, and I’m joined today by Janell Grazzini Frantz and Linda Wick, two nurse practitioners working in different roles but making a difference every day for our patients with transthyretin amyloid cardiomyopathy, also known as the acronym ATTR.
ATTR amyloid cardiomyopathy is a disease of protein misfolding, leading to amyloid fibril deposition in organs and tissues.
Once considered rare, it is increasingly recognized as a cause of heart failure. Today we’re going to discuss ATTR: what it is, working as part of a team to ensure coordinated care and effect change for those patients, and how to help patients and family members successfully navigate health care to reduce symptom progression and improve outcomes.
We encourage you to take advantage of the related resources available online at pcna.net/ATTR. Welcome, Janell and Linda.
I was hoping you could start off with sharing your role in caring for patients with ATTR. I’ll let you go first, Janell.
Speaker 1: Janell Grazzini Frantz
[00:01:25] Thank you, Kim. I’ve been a nurse practitioner for 23 years, specializing in heart failure for 21 years and amyloid for six years. 60% of my practice is amyloid patients—both ATTR and AL.
In my role as a provider, I deal with heart failure and possible amyloid patients. I watch for those red flag symptoms and order the appropriate diagnostic work-up to confirm the diagnosis and assure the type of amyloidosis. I prescribed tafamidis, the only FDA-approved medication for both wild-type and hereditary ATTR amyloid.
I assist with research studies of other treatments for ATTR amyloid and, finally, I manage the patients longitudinally, clinically or in research which includes management and palliation of the symptoms associated with amyloid—mostly congestive heart failure but also including low output heart failure, conduction disease, and arrythmias.
Moderator: Kim Newlin
[00:02:23] Linda, would you like to share?
Speaker 2: Linda Wick
[00:02:25] Thank you, Kim. I’ve been a nurse practitioner for 26 years.
I also have been taking care of heart failure patients for about the past 20 years. However, I don’t deal with amyloid patients to the same degree that Janell does.
I refer them to our amyloid specialists when I see heart failure patients that I suspect have amyloid. My role is actually somewhat administrative, in addition to being a provider, and I lead both ambulatory and acute care nurses across a large healthcare system and set up nurse navigation programs—or we refer to them as chronic disease management programs—one of them being for the heart failure patients that have amyloid.
Moderator: Kim Newlin
[00:03:01] [It] Sounds like you have lots of successes, but what are the biggest challenges that clinicians face in the diagnosis of patients with ATTR? Janell, I’ll let you start.
Speaker 1: Janell Grazzini Frantz
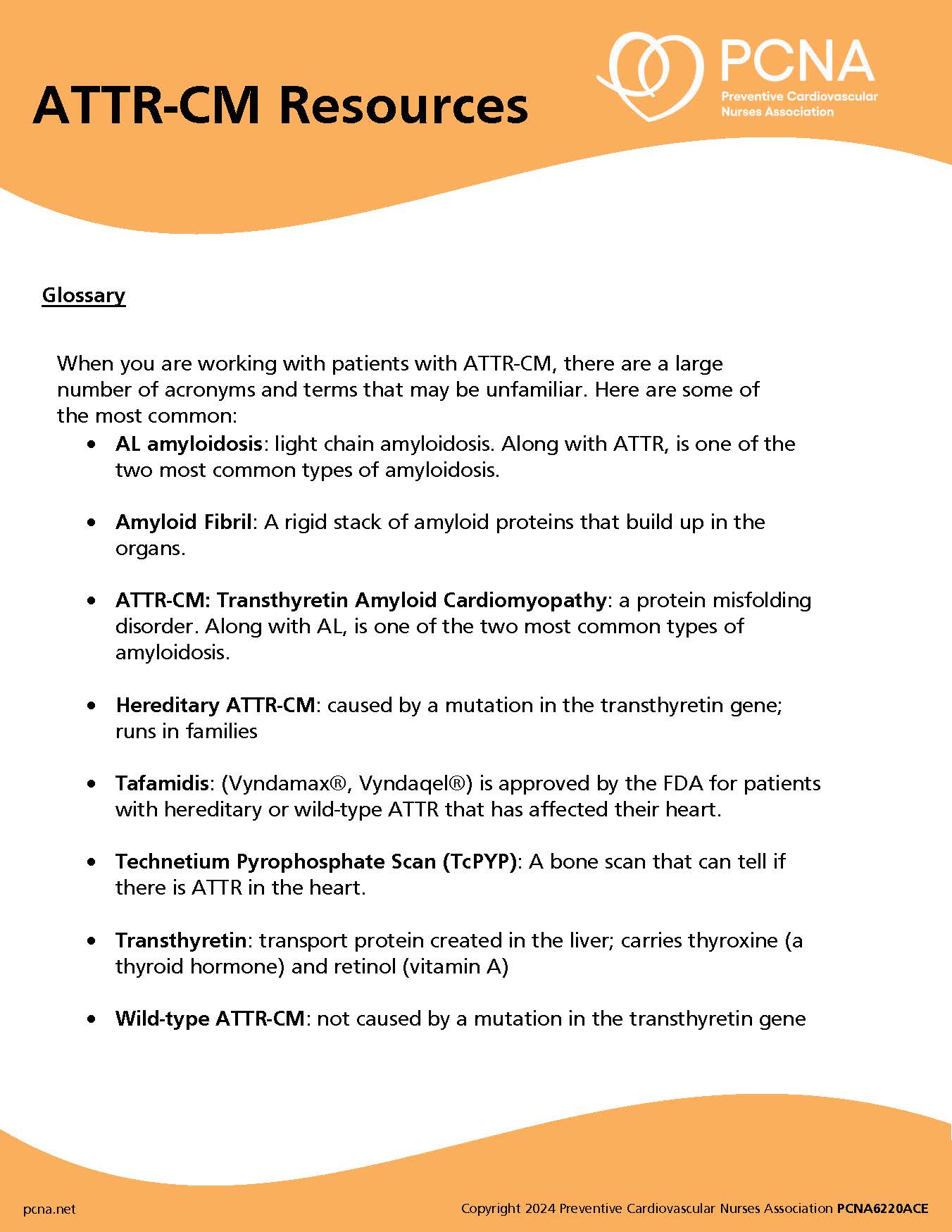
[00:03:10] I think first is beating the drum and educating other providers so that they recognize they might have an amyloid patient in front of them. Red flag symptoms and things I see on the diagnostic testing are:
- increased wall thickness on echocardiogram
- reduced longitudinal strain with apical sparing
- left ventricular hypertrophy on imaging
- normal, low-normal or low voltages on EKG
- AB block
- infiltrative features on EKG
- if you have an MRI, you may see marked extracellular volume expansion
- abnormal nulling time
- or diffuse late gadolinium enhancement.
Patients may have
- atrial fibrillation
- polyneuropathy
- dysautonomia, which includes orthostatic hypotension
- diarrhea, constipation
- and erectile dysfunction.
They may have bilateral or unilateral carpal tunnel syndrome; [00:04:05] bicep tendon rupture. They may have persistently mild elevated troponin levels; and just kind of anyone that they have an unexplained heart failure, especially when you see that thick wall, and the EF is preserved, but they don’t have a history of hypertension.
One other thing to think of is spinal stenosis is an early marker as well.
Moderator: Kim Newlin
[00:04:26] What about lab tests and other testing, Janell?
Speaker 1: Janell Grazzini Frantz
[00:04:29] So, it’s essential that you think about it so that you can start the appropriate work-up. The echocardiogram, and the patient’s own symptoms, will get you started, but you’re not done with that.
There’s a pyrophosphate scan, which also is called a PYP, which if that is positive, it’s very sensitive for ATTR, but it doesn’t rule out AL. And, therefore, you must get blood tests, including light chains, serum electrophoresis, a urine electrophoresis—and the electrophoresis must include monoclonal protein, and that’s very important to rule out AL amyloid.
[00:05:02] At Mayo, not infrequently will we have someone referred to us with ATTR amyloid, but the work-up was incomplete, and with further appropriate testing we realize they actually have AL amyloid. Valuable time’s been lost, which increases mortality substantially.
Since we now have treatments for ATTR amyloid, another challenge is educating providers that nailing the diagnosis is essential so that patients can avail themselves to the therapy to slow the progression and improve survival.
Moderator: Kim Newlin
[00:05:30] Thank you, Janell, for the high level of detail with that answer. Linda, what do you have to add?
Speaker 2: Linda Wick
[00:05:35] I think Janell hit the nail on the head when she said beating the drum and education and awareness. Because, as she went through the symptoms, they could also be representative of many other symptoms, and so it is hard to diagnose this based on symptomology alone. And, as Janell alluded to, really paying attention to that thickened wall of the left ventricle when there’s no history of hypertension.
Unfortunately, in heart failure, diastolic dysfunction is often underdiagnosed and underappreciated. And so, as Janell said, we often don’t see these patients referred to a specialty center until late in the game. [00:06:15] And so, the biggest thing for nursing to be aware of is to understand that some of these vague symptoms that just don’t make sense, that you can’t put together, think “amyloid”, and then get the referral and let the experts go through it.
As Janell went through all the work-up that are not something that typical heart failure clinicians do on a regular basis, it really underscores the importance of being referred to a specialist who knows how to work-up amyloid and diagnose it appropriately; and having the meds that we have now makes it even more vital to diagnose these patients early and slow disease progression.
Moderator: Kim Newlin
[00:06:55] As I hear you both talk. I appreciate being able to really put all of those pieces together and think outside the box a lot. Again, a lot of the educational materials on the website can help spell some of that out, if you didn’t memorize it all.
You mentioned people you’re working with, and I’ll toss this question to Linda first, who are your teammates who help the patients navigate the healthcare more successfully, and maybe on the same vein, what teammates do you wish you had, or would you recommend that others look to partner with?
Speaker 2: Linda Wick
[00:07:22] I’m going to talk globally first about heart failure because I think all heart failure patients deserve a team, not just our amyloid patients; amyloid patients have some special needs, of course.
For sure, it takes a team. It takes a village, and so the provider and the nurse navigator are kind of the quarterback of the team, I would say. But we rely heavily on our partners including pharmacology, our palliative care partners, our home care partners, our cardiac rehab partners, our social work partners, as well as our other specialties.
These patients often have renal involvement and so our nephrology partners, and they all need primary care. And so sometimes that’s hard, because these patients are so connected to us in the cardiology clinic and in the chronic disease management programs, they want all their needs at one place.
[00:08:11] But it’s vital that they continue to be connected with their primary care; nephrology, oncology as well are common for this population. The other players play an important role because they can help the patient navigate through their disease progression, where the nurse navigator again is kind of the quarterback and the touch point to make sure that all those pieces get tied together and do the education with the patient.
Moderator: Kim Newlin
[00:08:34] Great, thanks. Janell, what would you like to add?
Speaker 1: Janell Grazzini Frantz
[00:08:36] I agree the nurses are key. The primary cardiologist or the amyloid provider are key. At Mayo, we’ve got, basically, a cardiac amyloid clinic with dedicated physicians that have an interest, nurses that also have an interest and have the education, and me, as the only dedicated amyloid NP.
We also have a monthly interactive meeting with all other people interested in amyloid and that includes hematology, nephrology, neurology, pathology, research, GI if we can get them. Basically, anyone that’s interested. And then we share all sorts of different things from diagnostic challenges, what are we doing in research? Do we have to get a better template out to help people with the diagnostic work-up, things like that.
[00:09:22] I personally rely very heavily on my nurses in the amyloid clinic. They do the initial education for us (although we’re going to reiterate that as we meet with them over and over), they triage the phone calls, arrange the labs, call the patients back, check how they did with recent adjustments, and then they also assist the patients in enrolling and financial assistance for some of the medications.
We have a specialty pharmacy with pharmacists that can assist as well.
I wish we had a social worker on site, and I wish we had palliative medicine in our clinic, but those are easy enough for us to refer to. And then staying hand in hand (because we’re such a big referral site) with the referring physicians, the cardiologists, and their primary team. Because, as Linda said, this takes a team. It takes a village. [00:10:09] This isn’t a one person, one-stop shop. Everyone needs to pitch in because there’s a lot going on to help the patient get through it as easily and feel as well as possible and make sure they’re getting the appropriate therapies.
Moderator: Kim Newlin
[00:10:22] Having been a heart failure nurse for many years, I agree the foundation of any heart failure team is often the nurse, and it sounds like both of you play a fantastic role, but your teams as well are very helpful.
Again, this is for both of you. What are the biggest challenges you face in helping patients? And if you can share a story about a specific patient you were able to help, maybe highlighting your role as a nurse practitioner or nurse navigator. Janell, do you want to go first?
Speaker 1: Janell Grazzini Frantz
[00:10:47] It really is education for patients and their providers. I think kind of a frustrating and hard thing for me is everybody is like, “Well, this is just a different kind of heart failure.” But I think it’s a more concerning heart failure because this is progressive and will likely shorten their life even if they have cutting-edge treatment. We don’t have a cure yet.
Management needs more finessing. You have to figure out how to get the medication, tafamidis, to the patient, and how are they going to pay for it.
[00:11:13] What’s recommended for standards, say low ejection fraction (beta blockers and ACE inhibitors), are contraindicated and not well tolerated in amyloid patients, and it’s a common mistake, “Well, their ejection fraction is low. I’m going to go ahead and start a beta blocker.” But you want to be careful that you don’t make the patient sicker because these are not going to help the ejection fraction when it’s amyloid.
They can also have a very steep Starling curve where you have to give them diuretic to manage the fluid, but you don’t want to overshoot too far or you’re going to have them pass out.
[00:11:45] Deteriorating renal function will challenge diuretic management, and they might need a higher pulse to augment their cardiac output. This can be especially challenging, knowing how high is enough and how low is too low. I had a patient call me because he goes “You’re the expert. They want to put me on a beta blocker because my pulse is 100 and they think it’s too fast. What do you think?”
And so, I had to pull up his echocardiogram, because my recall was, he had a very poor cardiac index. [00:12:13] Well, his index was only 1.5. Remember it should be 2.5 or above and I said, “I don’t recommend a beta blocker. You need that pulse to generate enough cardiac output for you.” So, I think he was very appreciative.
Moderator: Kim Newlin
[00:12:27] Thank you, Janell, for your great thoughts. Linda, do you have anything else to add?
Speaker 2: Linda Wick
[00:12:31] One of the team members that I forgot to mention, and I know Janell, you have it at Mayo, too, is a geneticist. They [patients] often have to meet with our genetic counselors, and sometimes those workups are paid for, and sometimes they’re not, so that often becomes a challenge for these patients. I think our nurse navigators that work with our amyloid patients, because as Janell said, as their disease progresses and maybe go from what’s typically known as diastolic or preserved ejection fraction to systolic or reduced ejection fraction heart failure, people want to throw things at them that are contraindicated in amyloid. And as our patients go on the web, or their family does, and they’re like, “You should be on these medications.”
[00:13:12] And sometimes they get to the wrong provider who agrees with them, and they do get on these medications and then they get sick quickly and they come into the clinic and they’re in trouble because with the example Janell gave, we’ve just taken away their cardiac output and now they can’t do anything.
And so, I think the education piece is super important as they go through this disease and the nurse navigators are really good at constant follow-up, constantly being available to them to answer those questions/the go-to to person to double check, “Does this really apply to me?”
[00:13:46] The other thing: they oftentimes need frequent labs, as Janell alluded to, especially as we’re playing with their diuretics. It would be really nice if we had a standard dose of diuretic, but we don’t and everybody responds differently, and so sometimes you have to play with that a little bit to get the right dose for that particular person to keep them at their so-called dry weight without putting them in renal failure, and so that requires frequent labs and frequent adjustments.
And again, the nurse navigators, in partnership with the providers, are vital at doing that. This population you don’t just change their diuretic and see them back in a month. You’re checking labs again in a few days. And close follow-up, and so that’s where the nurse navigators are really important in managing these patients and keep them from decompensating quickly.
Speaker 1: Janell Grazzini Frantz
[00:14:29] I agree with that entirely, Linda. These are not, “I’ll see you in three months. Double your diuretic.” Their kidney function is touchy, and I agree the nurses are crucial in keeping track of them. “Did you get your labs today? How [are] you doing?” So, our nurse navigators—they’re my right arm.
Moderator: Kim Newlin
[00:14:46] Thank you so much, Janell and Linda for these great insights and clinical pearls. We’d also like to thank the audience for joining us for “What Did I Get Myself Into? ATTR-CM Nurse Navigation.”
A big thank you to Pfizer, Incorporated for support of this ATTR podcast series. Remember that you can access the podcast series and the related resources at pcna.net/ATTR.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more
Topics
- Cardiomyopathy
Published on
November 1, 2022
Listen on:
CNP, APRN, MSN

MSN, CNP, CHFN
Related Resources

Videos
A Nurse to Nurse Conversation on Hypertrophic Cardiomyopathy and Shared Decision-Making Video
January 19, 2025