Atrial Fibrillation in conjunction with Heart Failure can be a fatal combination. Join Dr. Laura VanBrocklin, DNP, FNP, RN-BC, FPCNA, as she explores these co-morbidities and complicated care plans.
Thank you to the Bristol-Myers Squibb – Pfizer Alliance for supporting this episode.
Episode Resources
- PCNA AFib provider tools
- PCNA heart failure provider tools
- ACC CardioSmart AFib resources
- Heart Rhythm Society
- American Association of Heart Failure Nurses heart failure prevention resources
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to today’s episode, the first of three focused on atrial fibrillation, also called AFib.
This episode will focus on the deadly combination of atrial fibrillation and heart failure. Today’s guest is Laura Van Brocklin. Laura, would you please introduce yourself to our audience?
Laura VanBrocklin (guest): Sure. As Geralyn said, my name is Laura VanBrocklin and I am a DNP. I currently work in electrophysiology at Denver Health. I completed my DNP at the University of Wyoming and got my undergrad at UNH. I’ve been a nurse for about 15 years and in cardiology for about that long, and then I also have been a member of PCNA since [00:01:00] 2011. So, exciting stuff.
Geralyn Warfield (host): Well, we are so excited to have you with us today, Laura, and I’m sure our audience can tell from your introduction that we’ve got a lot to learn from you about this subject.
So, let’s go ahead if you don’t mind, and dive right in. Can you please describe for us how atrial fibrillation again, often referred to as AFib, and heart failure can affect each other?
Laura VanBrocklin (guest): So, I’ll just run through a few quick stats about heart failure in AFib. In 2030, they’re expecting that about 12.1 million Americans will have AFib, and the majority of those being women, as it comes on later in age, and women seem to live longer.
Heart failure; currently we have about 6.2 million people that have heart failure, so as you can tell, it’s likely that these two heart conditions will exist together.
So, AFib is when you have an irregular heart rhythm. [00:02:00] Typically it comes from the left atria, the top chambers of your heart. This is a rhythm that is chaotic, usually happens where the, there’s a transition from the pulmonary veins to the heart muscle cells, and it typically can create fast, erratic rhythms from the top chambers, as I mentioned.
So, this can be completely asymptomatic. People can have no symptoms with this, but in general it can if it has fast heart rates, [which] lead to a weakening of the heart muscle. So, heart failure comes on because of a variety of different issues and problems. One of those being our silent killer, which is high blood pressure and then we have other risk factors, which such as [00:03:00] heart attack, coronary artery disease, remodeling, that type of thing.
So, when they coexist, when AFib and heart failure exist together, as I mentioned, AFib can weaken the heart muscle. Oftentimes with AFib and heart failure, we kind of run into this, which came first, the chicken or the egg? Did heart failure come first and then we had remodeling or changing of the heart muscle? Or did the AFib come first causing high heart rates, leading the heart muscle to become weakened? So, we kind of run into this Catch-22 when someone presents to the emergency room and they have heart failure symptoms, but their EKG shows that they have a rapid, AFib rhythm as well. And so, they really can come together, and we really don’t know which comes first.
And so, I guess today we’ll talk a little bit more about how to recognize what’s going on with each, how to treat each and what it [00:04:00] means when they’re together and what we need to do for both diagnoses.
Geralyn Warfield (host): So as a clinician, I know that you do see patients that present with either AFib or heart failure, or as you’ve just described, some combination thereof. And I’m wondering if you could explain to our audience what presentations you’d see in each of those circumstances. One, with AFib alone. Two, with heart failure alone. And three, when you have a combination of both.
Laura VanBrocklin (guest): So, with AFib, the classic symptom is palpitations or fast heart rate. Some folks will experience lightheadedness, dizziness, shortness of breath. Some folks will have this present after a fall or syncope. So irregular rhythms can be the presentation of this. Unfortunately, one of the presentations can be stroke. If there are no other underlying symptoms beforehand, unfortunately, AFib can sometimes present with, [00:05:00] hey, stroke symptoms of, “I got a change in my speech”, “I’ve got this headache that won’t go away”, vision changes, those types of things. And so, as one of the leading causes of embolic stroke, this is a reason why, this can be a presentation of AFib.
Heart failure in and of itself kind of presents usually, if you’re going into the emergency room, maybe some increased weight gain, some edema in the lower extremities, shortness of breath, or feeling like you have fluid on your lungs, chest tightness, some folks will describe. Other people won’t be able to lie down because there’s so much fluid on board in their chest that they get shortness of breath and are literally drowning when they lay down.
When these two come together, it’s kind of can be a pretty catastrophic mix because AFib exacerbates heart failure. Heart failure exacerbates AFib. So, then you just push all of these [00:06:00] symptoms together and then multiply them to, “Hey, this came on. Felt like it came on fast. I know I was having shortness of breath a couple weeks ago, but then, all of a sudden now I can’t breathe at all and I feel like my heart is pounding out of my chest. I can’t keep up with myself. I can’t keep up with the activities that I usually do.” And looking back, oftentimes patients will say, “Well, you know, I was having these symptoms maybe a month ago, but I brush them off because they weren’t a big deal.” And so, when it presents together, it kind of escalates at a higher rate than we would expect for somebody with AFib alone.
And AFib alone can sometimes come with absolutely no symptoms for some of our patients. Heart failure as well, together, not very likely that you’ll have somebody come in and be like, “I had no idea I had either of these things.” Does it happen? [00:07:00] Sure. But not quite as common as with either of these diagnoses alone.
Geralyn Warfield (host): We really appreciate you covering all of those types of symptoms that we might see in patients who are experiencing an episode of an AFib, or experiencing heart failure symptoms. And I’d like to hone in just a little bit more on the treatment for AFib. If a patient has AFib and it’s untreated and it’s AFib in isolation, what would be the outcome for that patient versus having a patient that has AFib in heart failure and then leaving that as untreated?
Laura VanBrocklin (guest): Right. So, with AFib alone, as I mentioned, there’s quite a spectrum of how people are affected by AFib. And there are oftentimes that asymptomatic patients are even asymptomatic with high heart rates. And so, they can come in and they’re like, “Oh, I feel great.” You get an EKG on them, and you see that their heart rate [00:08:00] is 135 and just ticking along. And so, AFib is much more likely to have a better outcome if it’s in isolation. And oftentimes we’ll respond really well to medications. We don’t rush to interventions or anything like that in asymptomatic patients with AFib.
And so typically we have time with AFib. For people to make a decision on, “Hey, do I want to start a rate medication”, which we’ll talk about in a little bit. Or “Do I want to start a medication to help me get back into a normal rhythm”. Which we’ll talk about a few of those in a bit as well too. But we have time on our side when we have an asymptomatic patient with AFib alone.
When we have heart failure in AFib, we then have, like I mentioned before, the acceleration of [00:09:00] symptoms potentially of heart failure as well as the increased risk for stroke on top of the baseline risk of stroke with AFib, and so we then get into this more urgent need to get this person into a normal rhythm. And so, this is when we think more adamantly about, “Hey, do we need to, they’re in clinic, do we need to admit them to the hospital because they have swelling in their legs? They have a fast heart rhythm. Their heart rhythm is also 135. They have shortness of breath, and they just don’t look good.” Maybe they’re pale, maybe they’re sitting there huffing and puffing while they’re just doing, just sitting there in clinic. And so, at that point, you’ve run into, “Hey, we need to do something more urgently because this AFib is not well tolerated. This patient is going to have some severe symptoms of heart failure [00:10:00], and already does, and we need to do something sooner rather than later.”
Unfortunately, in later stage, heart failure, AFib is a risk and so can come on with later stage heart failure. If it’s not addressed or found early on, this can lead to more complications, lead to further thickening or weakening of the heart muscle, and just creates a more difficult treatment set and poorer prognosis.
Sometimes this combination can even lead to death, unfortunately,
Geralyn Warfield (host): We’ve been talking with Laura VanBrocklin about the deadly combination of AFib and heart failure. We’re going to take a quick break and be right back.
[Leave this gap here]
Geralyn Warfield (host): We’d like to welcome back our audience to our discussion with Laura VanBrocklin about AFib and heart failure. Laura, I’m hoping you could review for our audience the evidence-based medications [00:11:00] that assist in treating heart failure.
Laura VanBrocklin (guest): Sure. Yeah. So, our go-to medications for a long time have been the ACE inhibitor or ARB to help out with heart failure and keep this stress on the muscle low. We’ve got our beta blocker, usually Metoprolol Succinate is what we go for, because that medication has been proven to reduce mortality in patients. And so that’s definitely our go-to beta-blocker.
We often have to choose a different beta blocker like Carvedilol depending on somebody’s lung disease and that type of thing. We’ve got Aldosterone antagonists, which are your Spironolactone. For African American patients we also choose Hydralazine and Isosorbide, which is evidence-based to help improve their outcomes as well.
Then we’ve got our diuretics. We [00:12:00] also have, more recently, the ARBs and the ARNIs. And then we also have our new and improved diabetic medications that somehow help with heart failure. And so, we absolutely love adding those to the group as well, especially because heart failure doesn’t typically run alone. It’s great if we can treat diabetes and heart failure together.
So, these are the main medications that we look at for making sure that we have best volume control for patients so they’re not having volume overload. We control the stressors on their hearts, prevent remodeling, and all of those things in heart failure.
And so, of course, all of these are used as tolerated, so we have to get to the point where, “Hey, this is as much as this patient can take of metoprolol, because if we don’t, then their heart rate tanks into the toilet or this is as much as they can tolerate of their ACE because of their blood pressure.”
And same [00:13:00] with the ARNIs to help out with the blood pressures and heart rates. We still have to monitor those and only put them on doses that are tolerable to them. So, there are these groups of medications and families that we use try to adjust as much as we can. The evidence-based has been around for a long time for the majority of these meds. And even the newer ones have been used in other countries for an extended period of time for us to have really good evidence that, “Hey, in heart failure, this is what we need to do to prevent worsening of disease and symptoms.”
Geralyn Warfield (host): That was a great overview Laura, and I feel like our audience has come away with the laundry list, I guess I would call it, of medications that can be used for heart failure.
If we could pivot just a little bit and talk about what those medications might look like in treating AFib and also, since we’ve talked about how AFib and heart failure sometimes go hand in hand, [00:14:00] either the AFib causing the heart failure, perhaps the heart failure causing the AFib, what kind of interactions in treatments would we see if we’re combining our heart failure and AFib medications?
Laura Van Brocklin (guest): So, the medications that help us out with controlling rate are typically beta blockers and calcium channel blockers are where we start. And so those medications help out by lowering the heart rate and making sure that those rates don’t get quite as high. So if you have somebody come into your clinic and, you put them at elevated Chads VASc, you put them on a blood thinner, and then you say, “Hey, how fast is their rate going? Do they have any lung disease? Could we trial a beta blocker to help bring down this rate a little bit if they’re not too symptomatic with the AFib?”
And it’s definitely something that can start in a primary care office, general cardiology, and typically in EP we also start [00:15:00] with these medications as a first line for folks who are relatively asymptomatic. They aren’t usually currently in heart failure, but if they are, and not already on a beta blocker, it’s a great time to start Metoprolol Succinate and get them on some rate control and also get them on guideline-directed medical therapy for their heart failure.
And the calcium channel blockers we don’t typically use in heart failure as they’re not one of the meds that are on the guideline-directed medical therapy for the heart failure. But it is something you can consider if they’ve already been on it or if the beta blockers aren’t working you could consider, “Hey, how can I finagle their heart failure medications to be able to get in a calcium channel blocker as well?”
Rhythm medications that we typically use would be sodium channel blockers or potassium channel blockers. And so, these rhythm medications are meant to keep you in a normal rhythm. If they’re not keeping you in a normal rhythm, they’re not [00:16:00] a good medication for you. But these are medications that would typically either be started with an EP or cardiologist as or in the hospital setting, because some of them do need monitoring prior to being able to take these outside of the hospital.
So, the sodium channel blockers would be things like Flecainide. Propafenone or Quinidine. Then we have the potassium channel blockers, which are your Amiodarone, your Sotalol, and your Dofetilide. And these medications can range in how much they cost for different people, and they range in who can take each medication.
So, some medications are limited by cardiovascular disease. Such as Flecainide. If you have any coronary artery blockage or had a stent in the past, or if you had an abnormal stress test, we’re not putting you on Flecainide. Unfortunately, in heart failure, a lot of these medications are not [00:17:00] indicated. So, our go-to’s in heart failure are typically Amiodarone and Sotalol, and those two medications, Amiodarone, can be used in anybody, but long term has some buildup of medication. So can affect liver function, can affect how your eyes are doing, can affect buildup in your lungs, which can make shortness of breath worse. And so, this medication we typically will use short term pretty comfortably, but over a year we would say, “Hey, we want to get you on a, either a different antiarrhythmic or we want to get you to have an ablation done as well.”
Sotalol, we can use that when folks with heart failure, but typically we don’t use it in folks with an EF that’s under 40 to 45. And so, it’s useful for some of our patients, but not all of our patients.
Most recent research would tell us that if you have a LVF or [00:18:00] left ventricular ejection fraction of less than 35, we do not want you to try these medications without an ablation. Best outcomes are to have an ablation done and try to keep you in a normal rhythm. Oftentimes we do an ablation, and medication to promote your heart to stay in a normal rhythm. And then typically, if your heart failure is caused by the AFib or the rapid ventricular rate AFib, typically Amiodarone and an ablation can keep you out of that rhythm and increase your ejection fraction from below 35. Not necessarily back to completely normal for all people, but it can improve how their heart failure’s doing and can change how your symptoms are treating you as well. And typically, if your ejection fraction improves, there [00:19:00] is the chance that you can come off the antiarrhythmic medication.
With these medications, with ablation, these are not things that take away your risk for stroke. So oftentimes patients will say, “Hey, I’m in a normal rhythm. I don’t have to be on my warfarin anymore. Right?” Or they will say, “I had my ablation when can I stop taking my Warfarin or my DOAC?”. So, if you have a Chads VASc of two or higher, you are always at risk of having a stroke no matter what we do to prevent you from going into an irregular rhythm. The likelihood that if you live long enough, you’ll go back to AFib, is very high, even with ablation.
Hopefully, in the future that will change and hopefully, in the future, more people might be able to have the left atrial appendage closures as technology improves and as research comes out to support this in the not-as-sick patients as well.
So, I think that’ll be stuff in the future, but currently [00:20:00] you still have that risk for stroke and you still need to be on your blood thinner.
Geralyn Warfield (host): Laura, you have described quite a variety of things when it comes to the treatments that we have for AFib and heart failure. It’s a definitely a delicate balancing act when we’re trying to address both of these situations in our patients. And because they are so complex, both independently and together, I’m wondering if you could point our listeners towards places for them to find guidance on the treatment of AFib and heart failure.
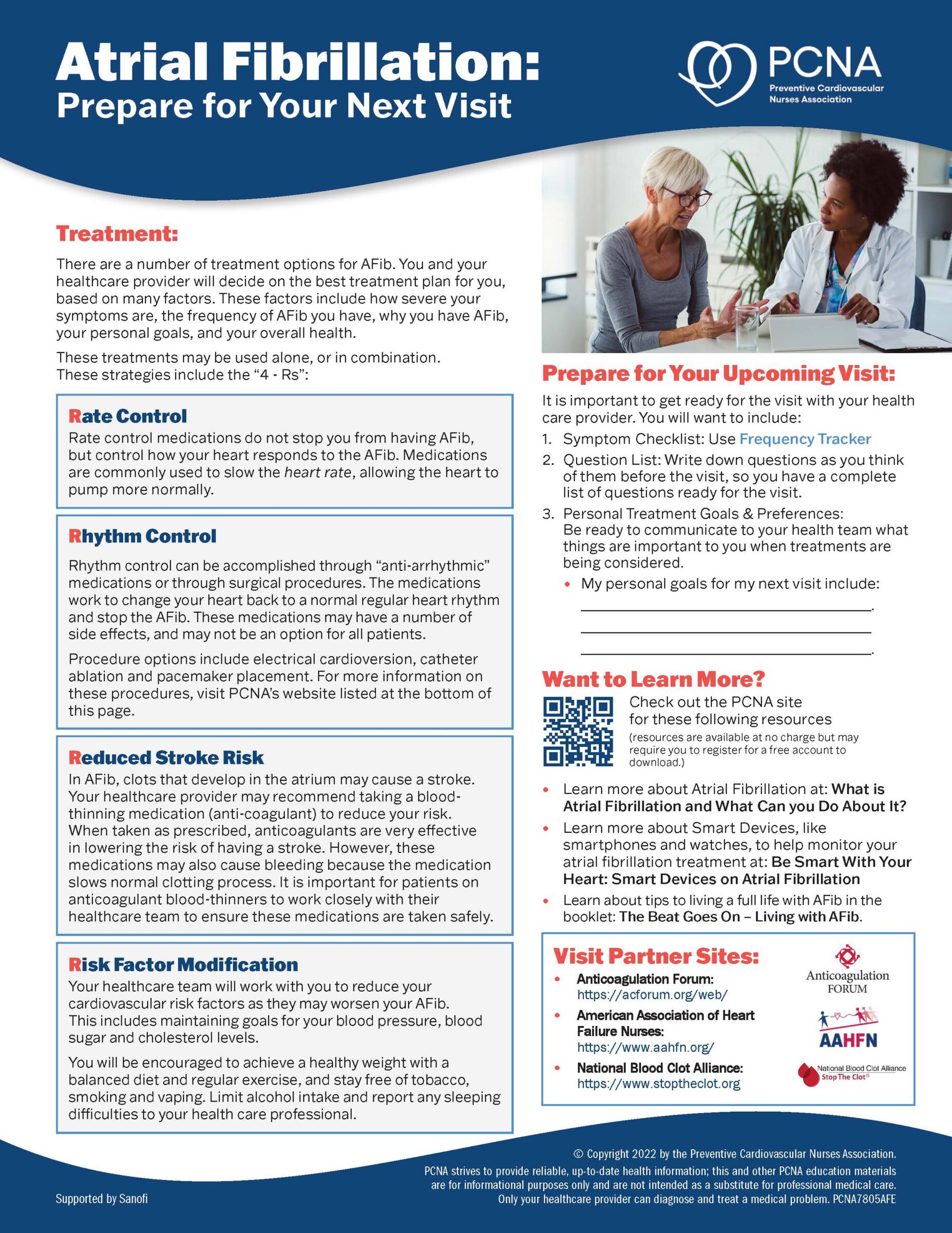
Laura VanBrocklin (guest): Sure. So, there are some great clinician and patient resources through the PCNA and you can get those off the website for sure. So, I obviously plug those and think those are great.
There was a really great infographic on AFib recently from Cardio Smartt from the ACC, and so that’s the American College of Cardiology and they have some great information for clinicians as well [00:21:00] that you can get off of Cardio Smart for AFib
There is the Heart Rhythm Society, they have some great information. Some of it is a little more EP brain oriented. So just to give you a heads up that sometimes it’s definitely more for people who are treating AFib every day potentially. And when I started in EP, half the time I’d be like, “I have no idea what they just said, but I know that I need to give this medication for this.” So definitely a different language in some ways.
And then we have the American Association of Heart Failure Nurses. They are great. They have some great resources as well, more based on the heart failure side of things in AFib, but they can also be a resource for you.
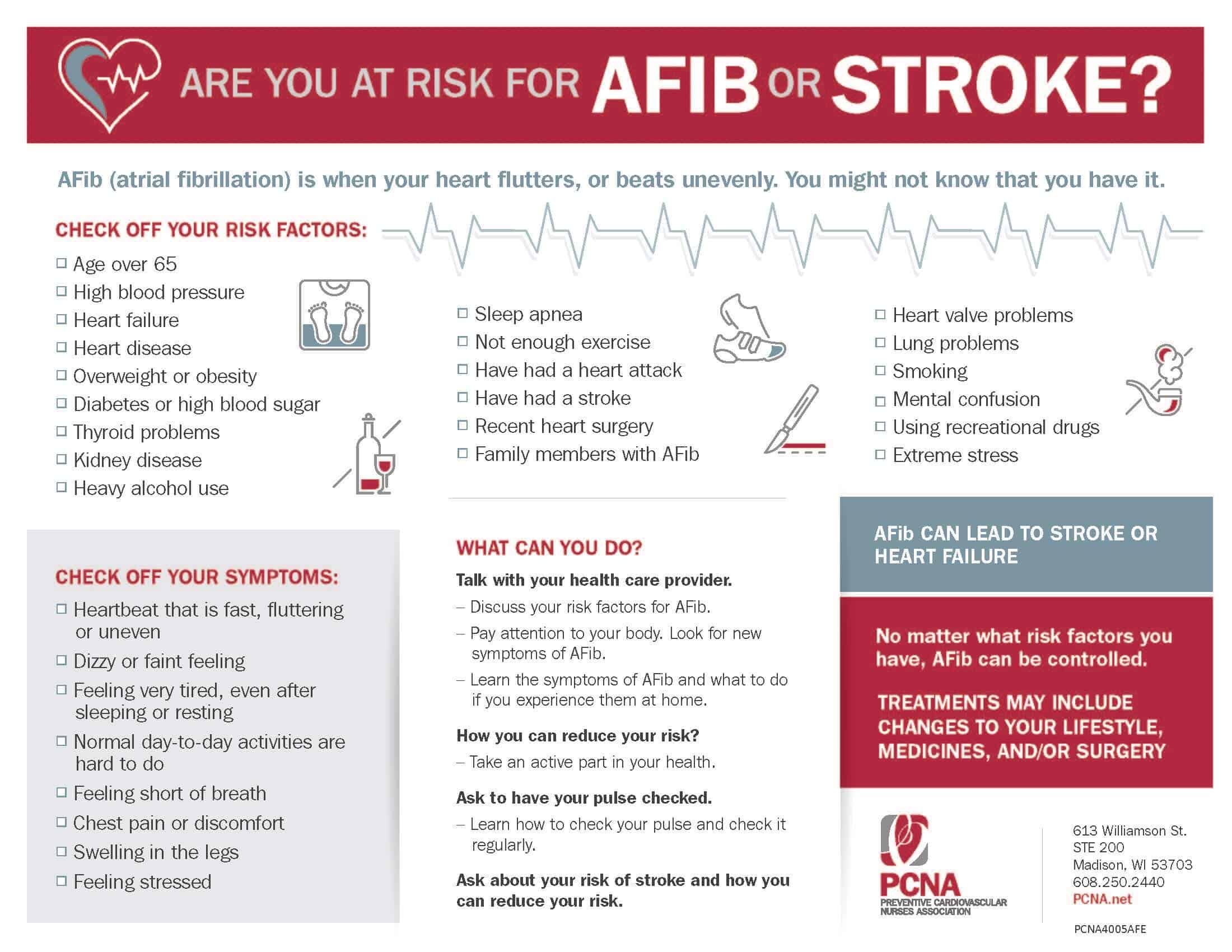
If you’re looking for general information, the CDC has great websites about who has AFib, what the risks for AFib are and that type of thing, if you’re just looking for general information, as well, and typically, I mean, you can [00:22:00] always reach out to look up and see what the most recent information is and studies and that type of thing.
But these would kind of be the groups that I would point you to, to help out find out what the general consensus is on guidelines.
Geralyn Warfield (host): Laura, you have given us such a great in-depth, and timely overview of AFib and heart failure and how guideline-directed medical therapy really involves kind of weighing pros and cons.
We didn’t talk specifically about it, but there’s definitely just a whole amount of shared decision-making with the provider and the patients, and we cannot thank you enough for spending time with us today, sharing your expertise with us.
We’d also like to thank Bristol Myers Squibb – Pfizer Alliance for their unrestricted grant funding, this podcast. This is your host, Gerald Warfield, and we will see you next. [00:23:00]
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Atrial Fibrillation
- Heart Failure
Published on
October 18, 2022
Listen on:
DNP, FNP, RN-BC, FPCNA
Related Resources