Episode Resources
- CHA₂DS₂-VASc Score Calculator
- WATCHMAN LAAC Implant
- WATCHMAN LAAC Implant Patient Screening Form
- Combined Anticoagulation Evaluator
- PCNA AFib Discussion Guide
- PCNA AFib Fibrillation Online Interactive Patient Guide
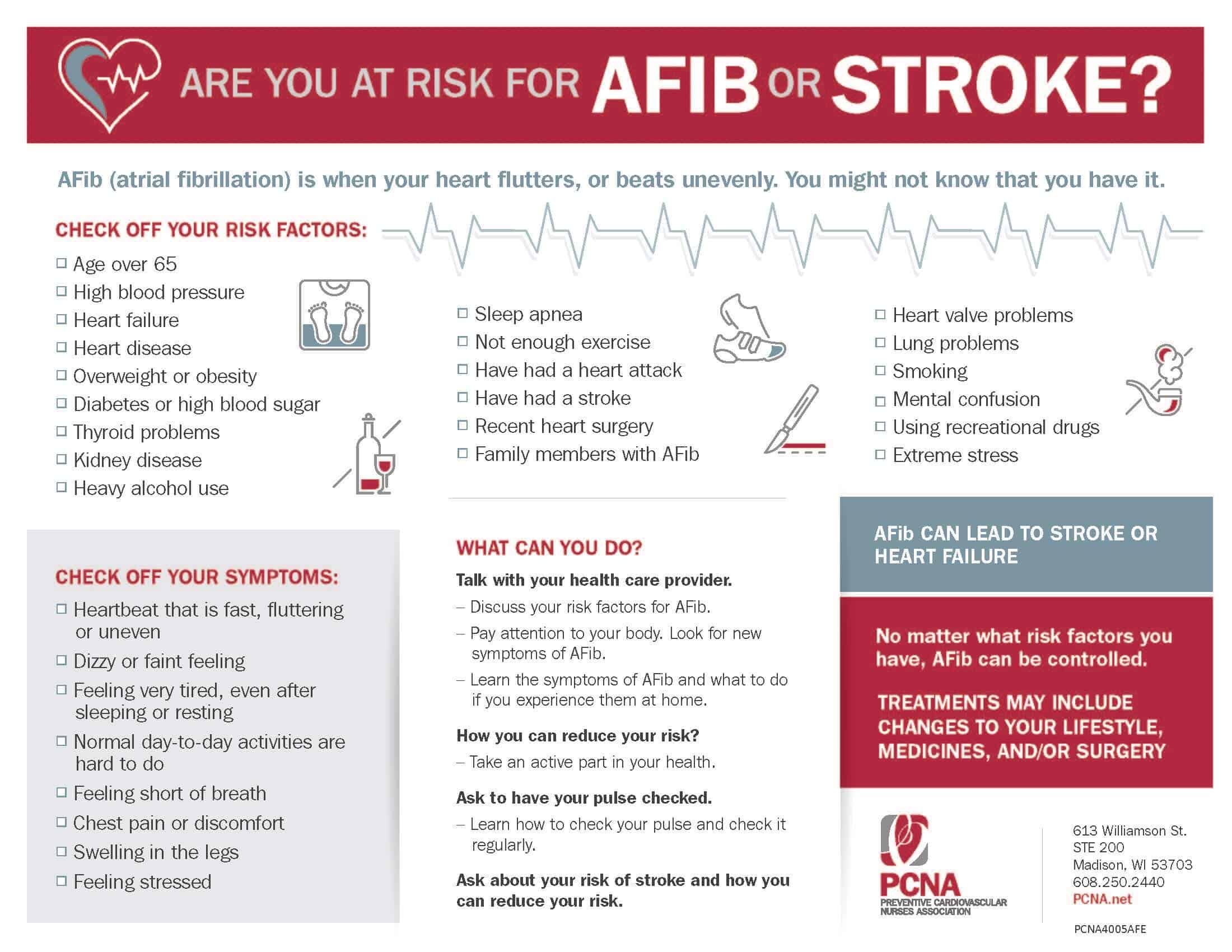
- PCNA AFib and Stroke Infographic
Thank you to Boston Scientific for their support of this episode.
Geralyn Warfield (00:19)
I’d like to welcome our audience to today’s episode where we will be discussing techniques for the prevention of AFib and stroke. We have a great guest with us today. And Rachel, could you introduce yourself to our audience, please?
Rachel Haagensen (00:31)
Hi, good morning. Thanks for having me. I am Rachel Haagensen. I’m a cardiology PA at Mayo Clinic in Rochester, Minnesota. I’ve been a PA for 11 years and with the last two and a half years in the outpatient structural practice with my primary focus in the left atrial appendage occlusion clinic.
Geralyn Warfield (00:51)
Well, I suspect our audience recognizes your expertise, and we’re so excited to have you here sharing that with us today. And I’m hoping we can get started with our conversation talking a little bit about pharmacologic and non-pharmacological treatments for AFib and stroke prevention.
Rachel Haagensen (01:05)
Great. Atrial fibrillation has been increasing in prevalence as our population ages and we have more obesity prevalence. And so really we want to focus on lifestyle modifications, weight loss, treating things like hypertension, diabetes. Also rate control, calcium channel blockers or beta blockers are kind of the go-to for a rate control.
Rhythm control, we can use antiarrhythmic agents such as dofetilide, sotalol, amiodarone. We also think about cardioversion to try to restore normal sinus rhythm, particularly if it’s the first episode or if a patient is very symptomatic. And then also catheter ablation to try to control the rhythm and again, restore normal sinus rhythm.
Another primary focus is certainly stroke prevention. Particularly in patients who have an elevated CHADS2 VASC score greater than two in men, greater than three in women, because we know that there’s a high risk of stroke in atrial fibrillation patients. And those strokes tend to be quite debilitating with an increased risk of mortality. So we really want to make sure we’re protecting our patients.
We also know that anticoagulation, which is the primary goal for stroke prevention or primary thing we use for stroke prevention initially, does have a low compliance rate. Many patients have bleeding complications. They don’t want to be on a blood thinner a long time. There’s lots of reasons that we see patients not on blood thinners when that could safely protect them from stroke. So then we think of alternatives for stroke prevention, such as left atrial appendage occlusion procedures.
Geralyn Warfield (02:53)
Well, that was quite a comprehensive overview of all the things that go into considering how best to treat these patients when it comes to rate control, when it comes to rhythm control. And I suspect as a healthcare professional, there are of course, guideline-directed medical practices, but you really have a lot of information to try and wade through and kind of consider, don’t you? And so how does that look in practice when it comes to you working with your colleagues on determining what’s best for each patient?
Rachel Haagensen (03:23)
We always kind of factor in the patient’s stroke risk. What are their symptoms? What we can best do to treat those symptoms and help them feel better. What is their bleeding risk when we think about blood thinners or procedures? And also patient preference and having that discussion openly with the patients about what they want to do, what they’re comfortable pursuing, how aggressive they want to be. So I think it’s also always important to just have that discussion with your patient. Propose all the options and have that joint decision making and doing what’s right for them and what they’re comfortable pursuing as well.
Geralyn Warfield (04:04)
So Rachel, could you talk a little bit more about that CHADS VASC score for us?
Rachel Haagensen (04:09)
Yeah, certainly that’s the score, the risk calculator, that we use to calculate how high the patient’s stroke risk is over a year. And so we give them points for things like congestive heart failure, diabetes, hypertension, if they’ve had a previous stroke or TIA or other thromboembolic event. And, factor in their age, as well as if they’re a female gender.
And so using all those components, get a score and that gives us a percentage of stroke risk each year. It’s sort of a rudimentary tool that we use. One of the best we have actually. It’s not perfect, but it gives us something to go off of to help decide if we think a patient should be on anticoagulation or if we need to consider other things for stroke prevention.
Geralyn Warfield (04:59)
Well, Rachel, we are going to take a quick break and we will be back to talk more about AFib and stroke prevention.
Rachel Haagensen (05:06)
Sounds great.
Geralyn Warfield (05:06)
I’d like to welcome back our audience to our conversation with Rachel about AFib and stroke reduction. And we had a lot of information right before the break about a lot of different techniques. And one of the things that you mentioned was left, I’m looking at my notes, left atrial appendage closure. I wanted to make sure I got that verbiage correct. Could you tell us more about that and what that entails?
Rachel Haagensen (05:29)
Yes, definitely. So left atrial appendage closure or occlusion is a procedure done in the cath lab typically in which a small device is inserted into the opening of the left atrial appendage. As we know that about 90 % of clots in patients with atrial fibrillation tend to form in that little appendage due to the sluggish flow, kind of the pooling of blood, when they’re in atrial fibrillation.
So these procedures, we have two devices that we use, typically the WATHCMAN TM or the AmuletTM, which is a slightly different design. Those devices were created as an alternative to the blood thinner for patients who have a contraindication to long-term anticoagulation or a very high bleeding risk. It is considered invasive. It’s done in the cath lab, typically under general anesthesia or moderate sedation. And that is chosen based on how the procedure is guided, either with transesophageal echo or intracardiac ultrasound.
It takes about an hour or so, plus a little prep time and wake up time for the patient. They do have a little bit of a bed rest afterwards as they go in through the right femoral vein to insert their catheter. And so we monitor that after the procedure, make sure there’s no bleeding complications. Many patients are able to go home the same day even. I would say 80 % plus of our patients do very well and are able to discharge home that same day.
Geralyn Warfield (07:02)
So I suspect there’s a lot when patients are trying to learn more about AFib, what all the options are, how to prevent stroke. But how does the conversation look when you are talking about this particular procedure? Because there are a lot of considerations for the patient in terms of, you know, what does this look like for me? How is this going to affect my long-term, you know, ability to do my daily activities? So how do you actually work with patients and caregivers to talk about this most effectively?
Rachel Haagensen (07:33)
So I see patients in the consult clinic who’ve been referred to us to directly consider this procedure. And so I usually start the visit with explaining why they were referred. What the referring provider was concerned about as far as long-term anticoagulation and why we might want to consider an alternative for them. Just so they have a full understanding of why they’re coming to us, why it might be beneficial in their situation.
We talk about the risks and the benefits of the procedure versus continuing on blood thinner or even going without blood thinner and kind of what that looks like. We talk about the procedure, what that all entails and what to expect as far as the day of procedure, follow up, medications that we use afterwards. And then just give them lots of time to ask any questions or go through any concerns they might have. Or make sure they have a full understanding of what their options are, and just to make sure everyone’s on the same page and everyone’s feeling comfortable with the choice that’s made.
Geralyn Warfield (08:39)
Thank you so much for covering both the science of what happens with these procedures and also the personal touch that it takes to make sure that patients and their families and caregivers know what’s happening. We’ve talked about a lot of different things thus far today, but I’m hoping you might be able to identify for us what your one key takeaway would be for those people that are listening or watching this particular episode.
Rachel Haagensen (09:02)
Left atrial appendage occlusion is a great alternative to anticoagulation for patients who cannot tolerate long-term anticoagulation or who have a very high bleeding risk and even certainly can consider just for patient preference with a good risk versus benefit discussion.
Geralyn Warfield (09:24)
Rachel, you talked a little bit about the referral that it would take to get a patient into a clinic to have this happen. What does that process typically look like? And are there any tips and techniques you might have for providers who perhaps do not have a facility within their own organization that does these procedures?
Rachel Haagensen (09:43)
So at Mayo, we typically want the referring provider to have had a discussion with the patient and make sure they qualify for the procedure, first of all. And so that means they have to have had atrial fibrillation documented in the past and a CHADS2VASC score of three per CMS guidelines. And so we want to one, just make sure they fit the criteria and that they’re appropriate for the procedure.
And so we find that sometimes we get referrals for patients who maybe a procedure is not in their best interest. They have active cancer or their life expectancy is reduced. And so just kind of thinking through, is it the right thing to consider an invasive procedure for this patient? And if so, then we have an order that sends the patient through a triage process. Our nurses in the heart rhythm clinic review the order they review the patient history to make sure we have all those components. And then if so, it gets sent on to clinic and we order the appropriate testing. We typically do a cardiac CT or TEE prior to make sure the anatomy is suitable to close the appendage as it’s not in every patient. We typically like to have that done close to the time we see the patient rather than in advance because we want to make sure there’s no clot in the appendage before we’re moving forward with procedure. And so sometimes if that’s done too early, we end up repeating. So one tip would be to kind of hold off on the screening anatomy until we get close to seeing the patient.
And for outside providers, I would say just they can go through the same referral process, just
placing that outside referral to an institution. I suspect most institutions will have some sort of triage to review and collect the outside records to make sure we have the documentation needed to ensure the patient has had atrial fibrillation and they would qualify for the procedure.
Geralyn Warfield (11:48)
Thank you so much, Rachel, for the key details about atrial fibrillation and stroke reduction that you’ve provided for our audience today.
And I am so grateful to you for your time for being here with us and sharing your expertise for those of us that are working with patients with these particular disease states and issues, and for how we can help work with them, their families, their caregivers, and our coworkers in moving this process along and providing the best possible outcomes for them. Thank you so much for that. I’d also like to thank Boston Scientific for their support of this episode. You’ll be able to find more information about this particular topic in the show notes, so make sure you check those out for more details and links for other information.
This is Geralyn Warfield, your host, and we will see you next time.
Topics
- Atrial Fibrillation
- Diagnostics and Devices
- Risk Assessment and Management
- Stroke
Published on
December 2, 2025
Listen on:

PA-C, MS
Related Resources
Online Interactive Guides
The Beat Goes On: Living with Atrial Fibrillation Online Interactive Patient Guide
July 30, 2025