Cardio-kidney metabolic disease is a complex disease with many interconnected and intertwining components. Join podcast guest Melissa Magwire, RN, MSN, CDCES, the program director of the Cardiometabolic Center Alliance as she lays the foundation for understanding the disease.
This episode is supported by Boehringer Ingelheim Pharmaceuticals, Inc.
Episode Resources
Welcome to Heart to Heart Nurses. Brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s Mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): We’d like to welcome our audience to today where we’re going to be speaking about cardio kidney metabolic syndrome, and I’d like to introduce our guest, Melissa Magwire. Melissa, could you tell us a little bit about yourself?
Melissa Magwire (guest): Sure. Hi, Melissa Magwire, I am a clinical nurse specialist in the area of both cardiology and adult endocrinology and a certified diabetes care and education specialist. I work in a Cardiometabolic Center of Excellence, but then I’m also the program director of the Cardiometabolic Center Alliance.
Geralyn Warfield (host): Well, we really appreciate you being here today, and I’d love for us to talk just briefly about the nomenclature about this disease state or series of diseases. Could you address that for our audience [00:01:00] please?
Melissa Magwire (guest): Sure, that’d be great. So, you know, there’s a lot of different ways that we kind of discuss this quote syndrome and we look at is it cardiovascular disease? Is it kidney disease or renal disease? Is it metabolic syndrome? And really the new nomenclature, instead of using the word renal, is kidney. So what’s kind of out there circulating for a couple of different reasons is cardio kidney metabolic syndrome and using the word kidney instead of renal is that to really give patients an idea of what we’re talking about. Because we know as healthcare professionals, we’ve thrown around renal forever. Patients may not know that, but patients know what their kidneys are. So we’re really hoping to adopt and really push that forward with our peers and as we talk to patients to say cardio kidney metabolic.
And I’m sure we’ll talk over this next couple of minutes in the podcast about the American Heart Association’s new definition and Presidential Advisory on the cardio kidney metabolic syndrome.
Geralyn Warfield (host): Well, since you brought it up, would you like to describe that for us?
Melissa Magwire (guest): Yeah, so what the AHA did was they [00:02:00] put out a presidential advisory really talking about this. And what it came down to in a nutshell was really recognizing the interplay or interconnect between cardiovascular disease, kidney disease, metabolic disease, including type two diabetes, MASH or MAFLD, and really trying to look at those as one syndrome instead of in these siloed areas of care where things may get missed. Really, not only as practitioners, but as patients as well. Looking at this as one whole disease state and looking at cardio kidney metabolic syndrome as a health disorder that’s connected to heart disease, kidney disease, diabetes, and obesity, and the poor outcomes that can come with that, if not addressed as a whole syndrome.
Geralyn Warfield (host): And for those of us that are a little less familiar with this, could you describe for us the pathophysiology that we might be discussing here?
Melissa Magwire (guest): Really, when you look at that, it’s, it’s so varied and so complex [00:03:00] and multi-layered, but really if you kind of just take a step back and think about what usually starts, the cascade of all of these is an increased level of adiposity. Frankly put obesity. And we know, especially in the United States, but also worldwide, obesity rates unfortunately are on the rise. And when you have an environment of obesity, we know that leads to increased oxidative stress and inflammation. Inflammation then leads to coronary vascular disease, the RAS blockade, things happening with hypertension, things happening within our liver, things happening within our, the vasculature of our heart, this oxidative stress. And we often like to say in our clinic when we’re working with patients and other providers, so goes the heart so goes the kidney. So you start this whole cascade of things. The formation of obesity then leads to inflammation, leads to metabolic syndrome, leads to type two diabetes. Type two [00:04:00] diabetes and hyperglycemia can further compound the issues in the vascular system. You know the stress, oxidative stress, on the heart, the coronaries can lead to heart failure.
We know that leads to kidney disease and liver disease. Liver disease is a risk equivalent of cardiovascular disease. We know that kidney disease is a risk equivalent for cardiovascular and poor outcomes. We know that those living with heart failure often develop kidney disease. We know those living with type two diabetes often develop kidney disease and heart failure, and I could go on and on and on about that connection, but that’s really why looking at this as an entire syndrome and starting at the root cause, which is often prevention with obesity and hypertension and those risk factors is really where we want to step in.
Geralyn Warfield (host): Thank you so much for that excellent overview of the interconnectedness, not just of the cardiovascular system and the kidneys, but what causes some of these issues from the outset that can cause some problems [00:05:00] further down the line. I have a question for you and it has to do with, how in clinical practice would you describe this? Let’s say in an electronic medical record or something like that. How would it be characterized there?
Melissa Magwire (guest): Well, you know, there’s nothing official yet, but hoping that people start to use this term cardio kidney metabolic syndrome or cardiometabolic syndrome, but don’t leave out the kidneys. So we are, at least in my clinic, really starting to say CKM syndrome as evidenced by Heart failure, cardiovascular disease, type two diabetes… and listing it out. And we do that for a couple reasons. We do that to be complete in our medical record, but also to train or teach unknowingly, potentially, other providers that are reading those records. And then we use that in our after visit summary as well with our patients so that our patients start to see this interconnectivity. Because you’re right, just to say someone has CKM syndrome, if we’re not quite used to that nomenclature yet as [00:06:00] providers or patients, it really helps to give that definition.
So CKM syndrome as evidenced by diagnosis of ASCVD or recent heart attack and then start listing the things that are in that syndrome, the cardiovascular disease, the metabolic disease, and the kidney issues.
Geralyn Warfield (host): We are going to take a quick break and we will be right back.
Geralyn Warfield (host): We are back with more conversation with Melissa Magwire, speaking about CKM syndrome and the variations that occur within that syndrome. And most specifically in this next section about guideline directed treatments that can be used to prevent or even slow down disease progression. Would you be able to address that for us?
Melissa Magwire (guest): Sure. And you know, at first look it can be really complicated because we know we have pillars of care for heart failure. You know, we have standards of care for those living with ASCVD and type two diabetes. We’re now looking at developing pillars of care for CKD or chronic kidney disease. But really when you [00:07:00] kind of unpack that, we’ve been very fortunate over the last 10 to 15 years to have had all these cardiovascular outcome trials that occurred in the metabolic space. Namely for the treatment of type two diabetes. We found that a majority of those drugs, specifically SGLT2 inhibitors and GLP1 receptor agonists not only lower glycemic burden but are also been found to combat things like MACE and all cause risk for heart failure hospitalizations and the development of heart failure. As well as SGLT2s and treating in heart failure and diabetic kidney disease and chronic kidney disease.
And so really if we start to unpack the guidelines that are out there, there are a multitude of agents that are treating multifaceted comorbid disease that you see in cardio kidney metabolic disease. So if we kind of take a step back and let’s talk about a couple of those SGLT2 [00:08:00] inhibitors I already mentioned.
SGLT2 inhibitors can lower glucose in those living with diabetes. But they also reduce the risk of heart failure or heart failure rehospitalization, and they also help with chronic kidney disease and the further decline of eGFR. So that’s going hit a lot of these risk factors that our patients are living with or conditions they’re already living with.
If we look at GLP1 receptor agonists, we know that those medications lower glucose in those living with type two diabetes, but we also know that they reduce MACE, they reduce obesity. They’ve shown recent improvements in HFpEF with the recent trials that have been out there or preserved ejection fraction.
There’s also some new trials out there. One of them, namely, that just reported out at ADA, called the FLOW trial that showed that GLP1, a specific GLP1 receptor agonist, helped slow the decline of eGFR. So you can see that these two drugs just in themselves hit a lot of the comorbidities and address a lot of the [00:09:00] risk factors.
Then we also know statins are in a lot of the guidelines for chronic kidney disease, believe it or not. That’s in there as a pillar, but also for ASCVD and those living with type two diabetes. so it’s hitting multiple things. We know that there are other drugs like the RASs inhibitors that should be given to those with type two diabetes and ASCVD.
We also know that that’s a pillar in heart failure. So as I’m kind of laying this out, you can see that a lot of these medications are used across the spectrum in the CKM syndrome. And so really understanding that you’re treating this global disease, I think really helps make that a little bit easier when unpacking what guideline directed medical therapy is for these patients that are living with this.
Geralyn Warfield (host): For our listeners who are interested in finding out more information about CKM syndrome, where would you point them towards?
Melissa Magwire (guest): Oh, I think there’s a lot of really, really good recommendations. But really the American Heart Association’s new presidential advisory really outlines this. And what they do is they [00:10:00] put CKM care in stages from true prevention, primordial prevention, all the way through to stage four, which is somebody who has had an event who is end stage heart failure or end stage CKD, and it very nicely outlines these stages of care. Not only GDMT or guideline directed medical therapy but the behavioral side of it too, and the lifestyle support and the need for weight loss and the need for diet, education and diabetes education. It also highlights the need for coordinated care, which I think, you know, you can tell during this conversation that that care coordination is going to be key to this.
And it also talks about addressing social determinants of health with patients living with this. And the good news is that, you know, it’s the whole lifespan of the patient, whether you’re in that pediatric patient all the way through to adult. So really a good primer on CKM syndrome and what stages and what actions you should take.
Geralyn Warfield (host): I have one more question for you today, Melissa, and that [00:11:00] is if you had one quick takeaway for someone who wanted to know about our conversation today, what would that one takeaway be?
Melissa Magwire (guest): I think that need for coordinated care. And to make it a little bit less overwhelming, is that to really just kind of look at this as a very complex multifaceted disease or syndrome and just knowing that we need to coordinate this for the patients and involve that shared decision making.
But really, I think the key word to me is just education. Educate patients, educate peers, and educate yourself.
Geralyn Warfield (host): Thank you so very much, Melissa, for spending time with us today and improving our knowledge about CKM syndrome and the interdisciplinary nature of both prevention and treatment that’s going to be needed for us to be able to address this ever-growing issue across our populations that we see.
For those of you that are interested in more information, you will find additional resources in the show notes for this [00:12:00] episode. We’d also like to thank Boehringer Ingelheim Pharmaceuticals Inc. for their support of this particular episode. This is your host, Gerald Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources. Continuing education and much more.
Topics
- Diabetes
- Kidney Disease
Published on
August 20, 2024
Listen on:
RN, MSN, CDCES
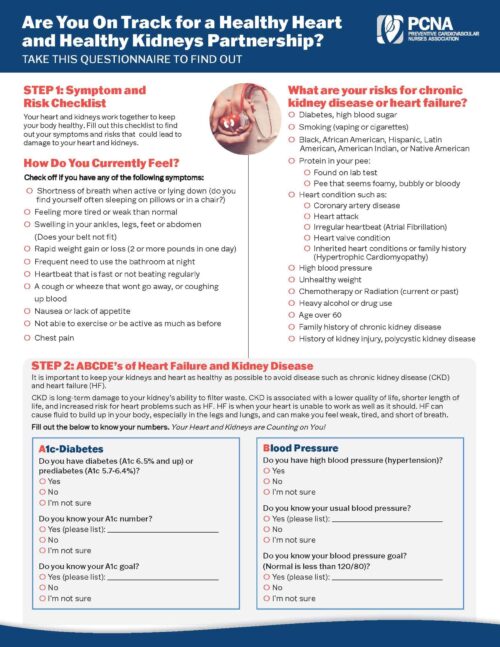
Related Resources
Online Interactive Guides
Diabetes and Your Heart: Close Connections Online Interactive Patient Tool
June 12, 2025
Provider Tools
Guidelines for Managing Cardiovascular Disease Risk in Patients with Diabetes Pocket Guide
January 19, 2025