Join Dr. Erin Ferranti in part one of this three-part series in partnership with Medical Alley that explores the bi-directional relationship between obesity and cardiovascular disease. In today’s episode, learn about obesity management and how social determinants of health play a role.
Take this short survey to provide feedback on this episode. Thank you in advance!
Thank you to Novo Nordisk for supporting this podcast episode.
Welcome to Heart to Heart Nurses. Brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to today’s episode, the first of a three-part series in partnership with Medical Alley, where we will explore the impacts that obesity has on cardiovascular outcomes.
Today I’m pleased to be joined by Dr. Erin Ferranti. Erin, could you please introduce yourself?
Erin Ferranti (guest): Yes, thank you Geralyn. My name is Erin Ferranti and I’m a public health nurse and nurse scientist.
I’m also a certified diabetes educator and diabetes prevention program coach, and my research focuses on examining cardiometabolic risk factors in at-risk women, both investigating some of the contributing factors to cardiometabolic disease and identifying interventions to help decrease risk factors in disease.
Geralyn Warfield (host): Well, I’m sure our [00:01:00] audience can tell that we have much to learn from Erin, so let’s go ahead and dive in.
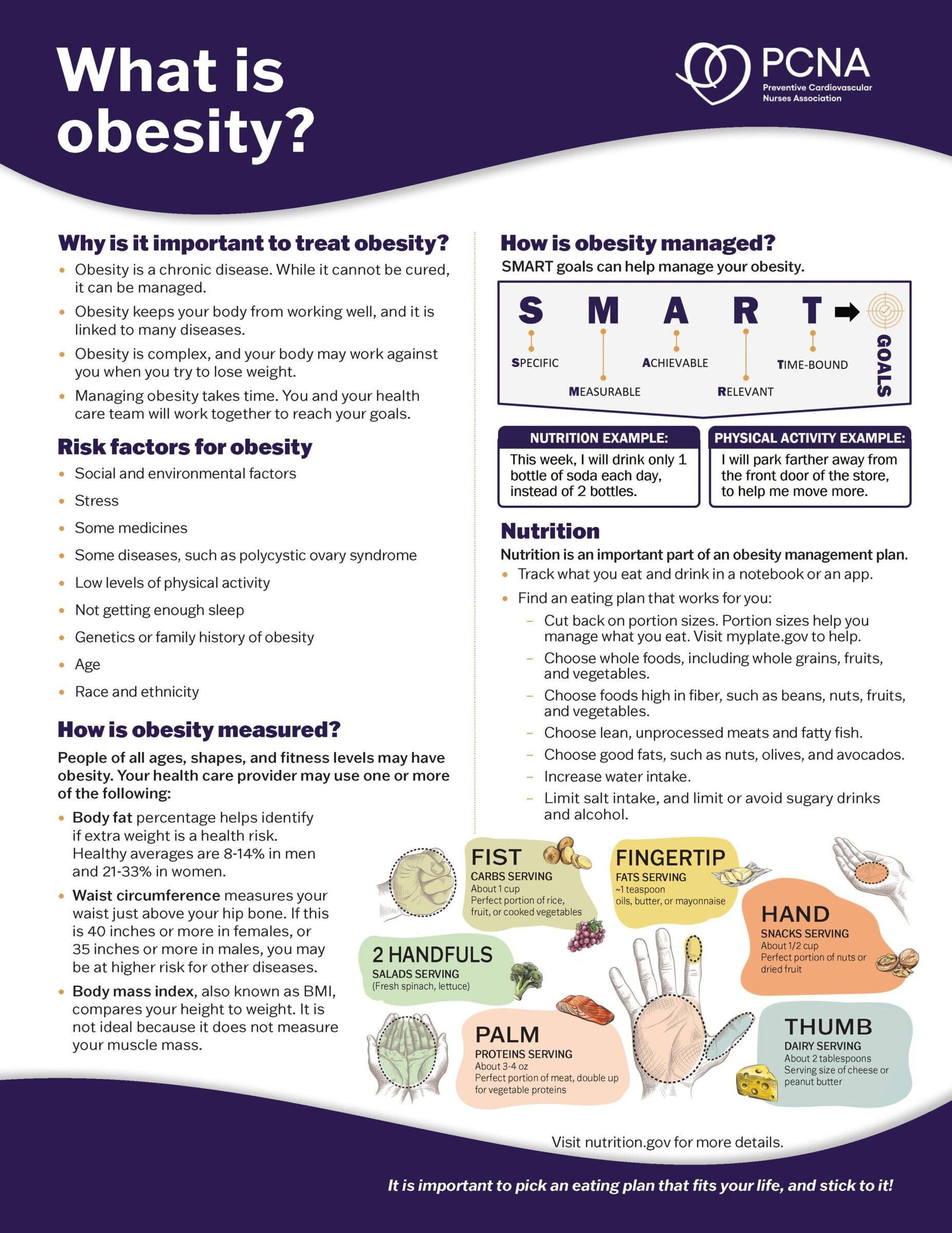
It’s now been a decade since obesity was classified as a chronic disease, one that will require clinical interventions beyond diet and exercise. It’s estimated that over half the global adult population is overweight or obese. Erin, could you please share with us what options are available for weight loss?
Erin Ferranti (guest): Absolutely, and I think I want to begin with saying that one of the big key misunderstandings about obesity is that this is a disease of willpower, but it is much more complex than that and actually has underlying biology that prevents people from losing weight and keeping it off.
So, there are many methods to address obesity and severe obesity, and it’s very person-specific as to what will work best. Some in isolation, some in combination. But the first is, the traditional lifestyle interventions, behavior modification, and increased physical activity.
[00:02:00] Other options include community-based programs like for example, the YMCAs host the Diabetes Prevention Program, which are support groups designed to decrease the risk for diabetes, but also one of the key goals of that program is to have about a 5 to 10% weight loss.
Then there’s commercial weight loss programs, and so, these are like your Weight Watchers, the Jenny Craig programs, every diet book that comes on the market, and then other programs to track food. So, like Noom is a new one and My Fitness Pal is another example.
And then there are clinician-supervised options. And those in, you know, are overseen by a clinician and they can involve either medical nutrition therapy, so there’s programs that can only be prescribed through a clinician. And then prescription meds, some that are fairly new on the market, and we can talk about those.
[00:03:00] And then finally, bariatric surgery and other devices to kind of manipulate the size of the stomach. So those are some of the main options.
Geralyn Warfield (host): Erin, I really appreciate the fact that you have brought to the forefront the issue of folks who have been overweight or obese over the years, suffering guilt, and suffering shame because they feel like they are at a loss. They’ve tried through willpower to accomplish the weight loss that they’ve been trying to, perhaps for years to lose weight and to eat healthier. And for our patients to be successful, we have this array of things that we can actually offer them that you’ve just described from lifestyle all the way through surgical opportunities. And I’m wondering if you could address for us the challenges with, for each of those, for our patients.
Erin Ferranti (guest): Absolutely. And yes, I mean, many people who suffer from overweight and obesity have really struggled [00:04:00] with the shame and the feeling of inadequacy that they have failed on some level.
But, you know, we live in an environment now that is very different from generations ago where we struggle now with having opportunities to be more physically active. We have processed foods available on the market, which weren’t, you know, 30, 40 years ago.
And people are not sleeping as well. The stress levels are high, especially in this Covid, post Covid era. There was a significant increase in weight during the lockdown. So just as a demonstration about how stress and isolation can contribute.
So yes, behavior modification and increasing physical activity is challenging just because to make that work in the context of a stressful life. You know, parents with children, jobs with multiple responsibilities, it’s really hard to fit that in. And particularly if you don’t have easy [00:05:00] access to healthy foods, that can make it very, very difficult.
Or if you don’t have cooking skills, you know, some of the healthiest ways of eating require whole unprocessed foods. But if you don’t know how to prepare those or you don’t have the tools to prepare food, it makes it very challenging.
With the community-based programs, like I mentioned, the YMCA Diabetes Prevention Program, those have a cost associated with them. And so oftentimes they’ll need a referral from a clinician. There’s cost associated with it. Not all insurance companies cover programs such as the Diabetes Prevention Program. Medicare does cover it, but a lot of State Medicaid programs don’t, and a lot of private insurance don’t cover that either.
So, you know, people have a really hard time paying out of pocket for something like that.
The commercial weight loss programs, [00:06:00] if any of you are familiar with, you know, Weight Watchers, Jenny Craig, again, those things have a cost associated with them and they don’t work for everybody. Not every program, you know, you’ll hear of friends or colleagues who’ve been tremendously successful on Weight Watchers, you go ahead and try it and it’s not working for you. So, there’s not a one size fits.
The clinician supervised options, so the medical nutrition therapy, and prescription meds, again these things are not always covered by insurance, and so out-of-pocket payment for this is really, really challenging for a lot of our population.
And then of course, bariatric surgery and devices, all, you know, surgery is a major thing. Not everybody’s eligible for bariatric surgery. It obviously requires being under medical care to have access to these options. And you know, if you’re severely, severely obese, you may not be able to tolerate the surgery.
So, there’s, you know, that’s why piecing together these different options. Trying to figure out what’s best for a patient, either in isolation or in combination, seeing what might work and then trying other things, it really needs to be very patient-focused.
Geralyn Warfield (host): We’ve been talking with Dr. Erin Ferranti about the interconnections between obesity and cardiovascular health. We’re going to take a quick break and we will be right back.
Geralyn Warfield (host): We’d like to welcome back our audience to our discussion with Dr. Erin Ferranti about obesity and cardiovascular outcomes.
We know that social [00:08:00] determinants of health can factor into this. We’ve talked about being patient-centric in terms of the types of activities that we’re asking our patients to participate in, that there might be cost barriers and there are some challenges depending upon our patients and what they have access to. So like the other disease states that we might be more familiar with, we see that people with lower resources are often the ones most likely to be impacted by obesity.
Erin, could you please explain why that might be?
Erin Ferranti (guest): Absolutely. It’s a very complex issue, as most things that are affected by social determinants of health are. As you can imagine, those with lower resources, lower education levels, live in areas that may not have easy access to healthy options.
So, if you’ve ever driven through a poorer neighborhood or community, you can just look around and see that there’s not a Whole Foods, for example, or even a [00:09:00] Kroger or you know, a big chain grocery store that brings in fresh produce every day.
You’re more likely to see fast food restaurants. And by the way things are priced in our country, fast food tends to be cheaper than a bushel of apples. So, if you’re a parent trying to feed multiple children, and you get a little free toy in one of the kids’ meals, you’re more likely to, just from a price point concept, feed your family fast food rather than try and shop for produce, which is not subsidized, tax-subsidized and tends to be more expensive overall.
So that’s one of the easiest things to see. But there are other social and economic and environmental factors that play into it. So, you know, clinicians ourselves and speaking as a clinician, as a nurse, we are not always [00:10:00] trained fully in how to help patients navigate this.
And so certainly if you don’t have access, you know, to medical care, you don’t have access to the resources that we talked about, but even if you do have access to healthcare providers, you know, slowly incorporating this content into nursing curricula, medical school curricula. But it’s not an area where like family providers have traditionally, you know, worked with this concept.
And insurance companies don’t pay for the longer visit that’s needed to counsel patients thoroughly on all the different options that they may have for treating overweight and obesity.
So those are some big areas. And obviously given that social determinants of health really affect overweight and obesity, we need a systemic approach to solving the obesity crisis. So, it’s not going to be [00:11:00] so on the individual as it has been.
We need to look at how do we bring in healthy options in these lower-income neighborhoods. How do we incentivize grocery stores and farmer’s markets to be in these areas? How do we make sure that people have adequate cooking tools in their house. I’ve been in situations as a public health nurse where I’ve done home visits and I can see, you know, they don’t have working stoves or working ovens. And so it’s really hard to make a healthy meal when you don’t have the tools in which to do it, or don’t know how to use those tools.
Geralyn Warfield (host): Erin, you have given us quite a variety of things to think of from the social determinants of health lens. And in a clinical setting, what kinds of things might you be doing as a clinician to try and get at some of these more basic issues that some of our patients are facing?
Because I anticipate that many of our patients are not going to be forthcoming, [00:12:00] may not feel comfortable with the provider, depending upon what the setting is, how often they’ve been to this individual provider’s office. Maybe it’s in a community outreach setting that they’re first seeing a provider, in a long time, perhaps for the first time in a long time.
But beyond that, what could an individual clinician do to try and start the process of addressing some of these resource and other issues?
Erin Ferranti (guest): Yeah, I think that’s a great question, Geralyn. You know, you mentioned patients may not be forthcoming with some of these issues that tend to be sensitive. They’re definitely sensitive and, you know, overweight and obesity has its own sensitive issues around it with the shame and things we talked about earlier.
So, the first thing is to really establish trust and to let it be known to your patient that you are not judging and you see overweight and obesity as a chronic disease as it is, and it’s not solely the responsibility of [00:13:00] the individual.
There are some short assessments that you can do, like paper surveys that address some of the social determinants of health, where you can get an idea about your patient’s food insecurity issues. Do you know, do they have access to healthy foods? Do they run out of money by the end of the month in which to buy produce? That happens with some of the SNAP and WIC programs, the Federal Nutrition Assistance Programs. Where they have more month than they have money coming in.
So yeah, really establishing that trust. Having the time in which to work with patients on this. Advocating for insurance companies to cover appointments that fully address, you know, all the issues that go into overweight and obesity. Having the time to sit with your patient and recognize that. And really letting the patient know, you know, there [00:14:00] are monumental systemic issues that are contributing to overweight and obesity. And how can I help you navigate, you know, what is going on in your neighborhood, in your workplace?
And a lot of it is problem-solving and linking people to needed resources. I was just reading a document that was highlighting how much people who are eligible for food assistance, for federal food assistance, how many people are actually enrolled in those programs. And it ranges anywhere from like 40% in some states, all the way up to a hundred percent. So, there’s real opportunity for us as providers to connect people to the resources that they need.
Geralyn Warfield (host): Those are all excellent suggestions, Erin, and I’m hoping that you might be able to help us understand just a little bit more with all of the issues that are facing, those that are overweight and obese, what are those links to cardiovascular disease? And it’s not an isolated [00:15:00] factor that obesity is, you know, an issue that affects your metabolism, that it also affects your heart and cardiovascular system as well. So, could you address that a little bit for us, please?
Erin Ferranti (guest): Absolutely. So overweight and obesity is a precursor to a lot of chronic diseases, not just cardiovascular disease. But since that’s what we’re focused on, there are direct effects of having additional weight.
So, the heart has to pump harder, it has to pump stronger when your body mass is higher than, you know, it was designed to be for your cardiovascular system. So that puts excess pressure on the heart, on the vascular system. Its why hypertension is often associated with overweight and obesity.
And then there’s some of the indirect effects of obesity. So, insulin resistance being one of the [00:16:00] key factors. So, insulin resistance is when your muscles are not as keen to uptake the insulin, and so your average blood sugar will stay higher. That puts tremendous strain on your vascular system, on all the microvascular, small vessels in your body. Which is why diabetes is associated with neuropathy and kidney failure and all the things, you know, associated with, long-term high, blood sugar there.
There’s also, like I said, hyperglycemia, which is high blood sugar, puts pressure on all the systems. That’s why, you know, cardiovascular disease and type two diabetes and obesity, all three of them are systemic whole-body diseases because it affects everything. Hypertension, as I mentioned, and then dyslipidemia. So those are like abnormal cholesterol levels, abnormal triglycerides.
So, and those each and of themselves incur [00:17:00] additional risk, which sets up the pathway to cardiovascular disease.
Geralyn Warfield (host): We are so grateful to our guest, Dr. Erin Ferranti, for today’s insightful conversation about obesity and cardiovascular disease. This episode is part of a three-part series in partnership with Medical Alley on the bidirectional relationship between cardiovascular disease and obesity.
For additional obesity-related content, we encourage our audience to visit the show notes from today’s episode. We’d like to thank Novo Nordisk for unrestricted grant funding for this episode.
This is your host, Geralyn Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit PCNA.net for clinical resources, continuing education, and much more.
Topics
- Obesity Management
Published on
February 21, 2023
Listen on:
Related Resources