Join Dr. Kathy Wood, PhD, RN, FAHA, FAAN, as she explores utilizing shared decision-making for your AFib patients. Leave this conversation with tools and resources to activate your patient’s engagement in their AFib care.
Thank you to the Bristol-Myers Squibb – Pfizer Alliance for supporting this episode.
Episode Resources
- Agency for Healthcare Research and Quality (AHRQ) website for Shared Decision Making (the SHARE mnemonic)
- Choosing Antithrombotic Therapy for Elderly Patients with Atrial Fibrillation Who are at Risk for Falls
- US hospital webpages on atrial fibrillation ablation: A potential source for misinformation
- Cardiac Tachyarrhythmias and Patient Values and Preferences for their Management: the European Heart Rhythm Association (EHRA) consensus document endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE)
- Provider Decision Aid Information:
- Univ of CO Shared Decision Making, Colorado Program for Patient-Centered Decisions
- Ottawa Hospital Research Institute
- Dartmouth Center for Shared Decision Making
- ACC’s CardioSmart page on Shared Decision Making
- Health IT.gov Shared Decision Making tip sheet PDF
- Patient Resources
- American Heart Association (AHA) sponsored website “My Afib Experience”
- StopAFib.org patient site
- Ongoing Trials
- ENHANCE AF
- Univ of Colorado Patient Centered Decisions Research Group
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to the third of three episodes focused on Atrial Fibrillation. In today’s episode, we’re going to tackle how to activate care for our patients with Atrial Fibrillation, which is also known as AFib. Today, I am honored to be joined by Kathy Wood. Kathy, could you introduce yourself?
Kathy Wood (guest): Sure. My name is Kathy Wood. I’m an Associate Professor at the Emory University, Nell Hodgson Woodruff School of Nursing in Atlanta.
Geralyn Warfield (host): I know, Kathy, that you’ve had some experience working with patients with AFib. Could you describe that briefly for us?
Kathy Wood (guest): Sure. I started working in electrophysiology with supraventricular tachycardia and AFib patients at the [00:01:00] University of Alabama in Birmingham in 1983. And, at Case Western in Cleveland with Dr. Waldo in 1986. And then, UCSF in San Francisco with Dr. Shyman in 1991. And have been also on the industry side in devices for patients that have Atrial Fibrillation.
Geralyn Warfield (host): Well, Kathy, oh my gosh. You’ve got such great experience and we are so lucky to have you on the podcast today.
So, let’s go ahead and get started if we can.
Kathy Wood (guest): Sure.
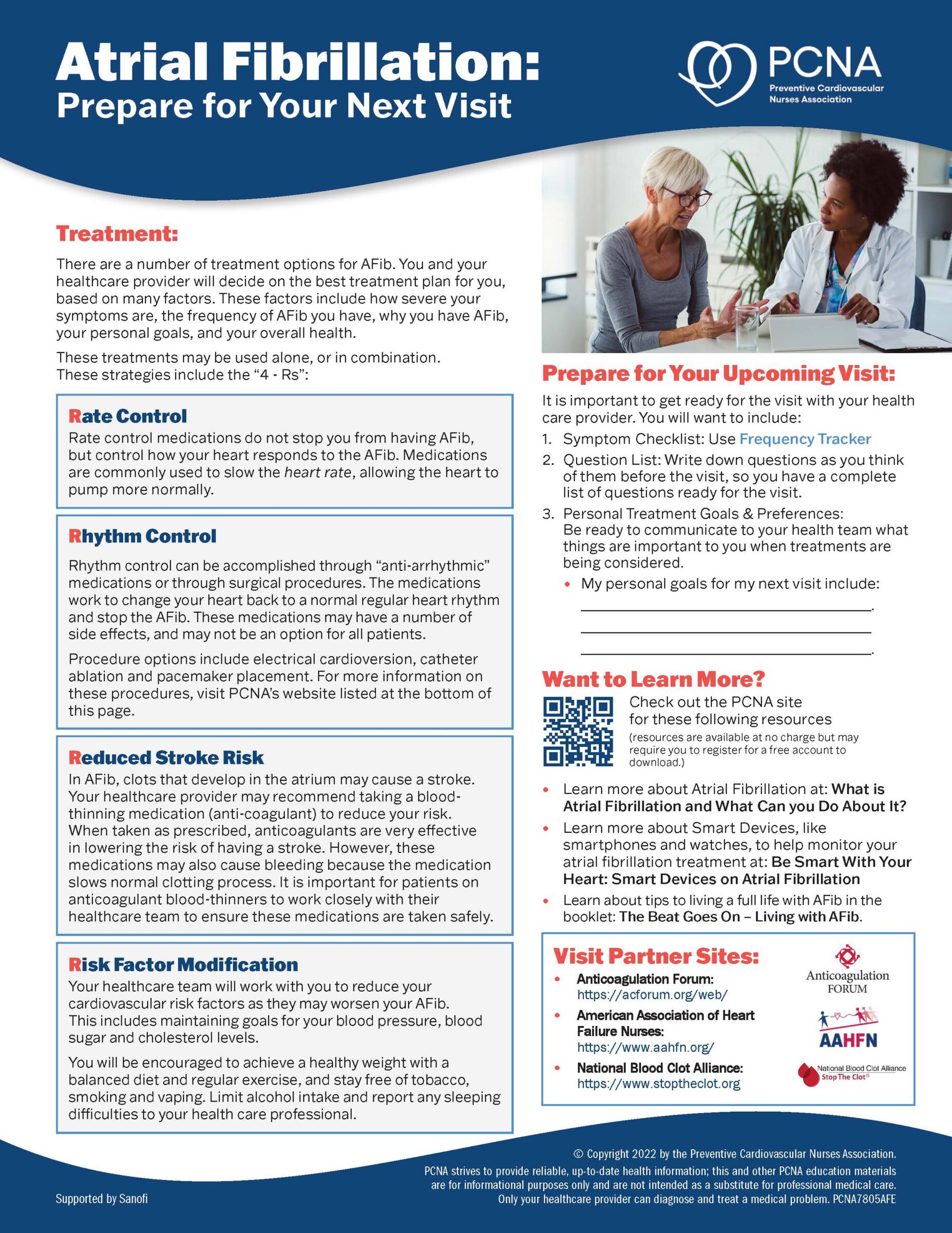
Geralyn Warfield (host): I’ll give our audience just a quick recap of what we’ve done in previous episodes where we covered the different treatment options for patients with AFib, including those who have other disease states such as heart failure or venous thromboembolism, also known as VTE.
And as clinicians, we recognize that an important piece of choosing the right treatment plan is having a shared decision making [00:02:00] conversation with the patient on what might work best for them. Could you please talk a little bit about this process and what evidence-based strategies we can implement to receive the best outcomes for our patients.
Kathy Wood (guest): Yes. We’re kind of in the beginning of evidence-based strategies, but shared decision making encourages patients to play a more active role in the process of decision making regarding their treatment. It’s really important when there’s more than one reasonable treatment option when there’s an obvious answer it’s not necessarily, necessary. But it is a conversation between the patient and their clinician where the risks and benefits of all the treatment options are presented in a balanced manner, and then you inquire about the individual patient preferences or their goals for their treatment, and you engage the patient in decision making.
Now, some patients are really interested in this. And some are not, and they really want to defer to the clinician. But [00:03:00] we found the more we do this, the more we find patients are interested in participating. So, with AF patients, shared decision-making discussions are usually led by an EP physician or their designated nurse practitioner or physician’s assistant that works in that practice or healthcare system.
And these types of discussions are usually easier for nurses because of our focus on the whole person versus just their illness. But as far as evidence based, the AHRQ or the Agency for Healthcare Research and Quality uses an evidence-based mnemonic called SHARE. Where S stands for seeking your patient’s participation, letting them know that we want to hear from them. We want to hear about their preferences, and that’s a key point in the process. H is for helping your patient to explore and compare the options but providing information on the benefits and risks of each. This is [00:04:00] often where we bring in a decision aid. If we’re going to use that, we can talk more about decision aids later. And A is to assess your patient’s values and preferences by asking them what is important, what are they concerned about, what are they most fearful about? And R is to reach a decision together by letting them know that they have time to think about it if they need that, or they can make their decision that day in clinic or in the encounter. You can ask them also at this point what other information they might need, what other questions they might have about the treatments that we haven’t covered. And then finally, E is to evaluate the patient’s decision together by addressing any concerns they might have.
In AFib, I can give you an example of a shared decision-making situation.
Shared decision-making has garnered a lot of attention in electrophysiology recently because the centers for Medicare and Medicaid, CMS, has mandated [00:05:00] shared decision-making as a condition of Medicare coverage for three conditions. One is lung cancer and using low dose CT scan. In 2016, it was decisions about a left atrial appendage closure device for stroke prophylaxis and patients that couldn’t take oral anticoagulation. And then more recently as far as implanting ICDs or implantable cardioverter defibrillators for primary prevention in sudden cardiac death. So not only does this involve a discussion, but also the documentation of the discussion to receive insurance coverage for the procedure.
In the cases of left atrial appendage closure devices, patients have a choice between long term anticoagulation therapy with the bleeding risks, an invasive procedure with the procedural risks, and then no treatment with the appreciable stroke risks. So, theoretically, [00:06:00] one treatment is not superior to the others. And in this example, you can go through the steps of SHARE, but if the patients often have questions about falls and how that would affect it if they took the oral anticoagulation. And you can spend time talking to them about fall prevention activities, strength training, or Tai Chi training, if it’s an older adult that has shown to reduce falls, those kinds of things.
Geralyn Warfield (host): Kathy, I really appreciate that SHARE acronym in how we address shared decision making with our patients. We all know that this is a relationship with our patient and like all relationships, it doesn’t always go smoothly. So, I’m wondering if you might be able to discuss that time when we might be having difficulties in this shared decision-making conversation process and what strategies you might suggest to try and avoid or address those difficult moments.
Kathy Wood (guest): Yes. These, [00:07:00] shared decision-making discussions do add time to the clinic visit or the patient encounter in the hospital setting. And so, it can be challenging, but what we found are some points that make it a lot easier. One is the process has to be incorporated into the clinical workflow, so it can’t be an extra step that you’re doing when you’re seeing that patient and other patients that day. So, we got together as a group and wrote a script with key words, key language, key points that should be discussed and brought into the shared decision-making interaction from all the providers in our practice.
And that way we were all using the same language, the same risk benefit figures, the same decision aids. And consistently we were all kind of doing the same thing, which really helped. Some centers I know [00:08:00] have their decision aids online, so patients can check those out before their appointment, and they’re referred to that online website to look at the decision aid. So, they come in with questions.
In other centers, they give the decision aid to the patient, and they look at it and are followed up later with questions. So, either way, it just lets them know that they aren’t forced to make a decision on the spot, but they can put some effort into learning more about the procedure and the process for the shared decision-making encounter.
The other thing we found that works is a designated clinician responsible, and that could either be the physician, and each physician does their own encounter. Some people using that SHARE acronym again, will send the nurse practitioner in for the first SHA; seeking, helping and assessing the patient values and [00:09:00] preferences, and then the physician comes in for the R and E part to reach a decision, answer questions, and evaluate the decision.
Other centers do it just the other way around, and the physician does the whole. S-H-A-R-E part of the shared decision-making encounter, and then the nurse follows up with them later, a week later to see what decision they’ve made. It really depends on the difficulty that the patient has in making a decision, and that’s individualized by patient.
But the most important thing that’s helped us is a template that we developed for documentation. So, in the paper, at some centers still are doing paper charts, and they can develop a stamp where the provider just fills in the details such as the date and time, their name, what was discussed, and usually that is already in the template, and then the decision and [00:10:00] the patient’s choice and outcome.
So that can be an online form in the computer system that can be filled out quickly after the encounter, or it can be left open if the patient wants some time to think about it and someone comes back later and fills that in. So, people have worked different ways, but those are kind of tips that we use.
The decision aids also, this might be a time to bring that up in the conversation, have been terrific. There’s a lot of different ones, but we use the ones from the University of Colorado’s Center for Patient Outcome, and I can give you more details about their website and their work later. We can also put that in the show notes, that might be helpful.
But the decision aids enhance the patient’s understanding of the risks and really has helped us provide uniformity in how we present the content for a shared decision-making encounter. There’s a lot of evidence [00:11:00] based findings about the best ones to use for which condition and with which patients, but usually we use one that has little hearts on it. And so, you can show if you make this choice, here’s the number of patients that end up with this outcome versus the other outcome. If you make the other choice here’s the example of patients that turn out with one outcome versus the other. If we stick to the oral anticoagulation and stroke example, we show how many people would have a stroke with one option versus another.
So, it’s helpful. Patients can quantify what we’re talking about more readily when they see the individual people or the individual hearts on the decision aid.
Geralyn Warfield (host): Those have been excellent strategies that you have shared with us in terms of how to activate our patients through a shared decision-making process. And also, you have eloquently described team-based care and the [00:12:00] importance of having the right person at the right time, speaking with the patient about what is happening and what the options are. And the use of decision aids helping share information and what potential outcomes might be.
I wonder if you could spend just a moment more speaking about, for those patients that are not making a decision in the clinical setting at that moment, you said you’ve left that record open. What’s the follow up look like from your clinical perspective with those patients. Is it anything that’s happening between now and the next clinical visit, or what are the triggers that you’re using to try and follow up with those patients?
Kathy Wood (guest): Well, here at Emory, we give them one week to make a decision. We send them home with information such as the decision aid and information and websites for each of the types of therapies. If we stick again to the oral anticoagulation versus left atrial appendage closer devices versus no treatment [00:13:00] example, we send them home with decision aids that show the number of people at risk of stroke for each outcome.
So, they go home with those decision aids and then, they notify us. We give them a contact person of our nurse practitioner and they email her. Or if one week has gone by and we haven’t heard from them, she contacts them and follows up, and that can be another telehealth visit if they want physician in on it as well, we can schedule that meeting, or the nurse practitioner often answers all their questions and they give her the decision they’ve made that’s then recorded in the medical record.
Geralyn Warfield (host): Have you ever found that patients are just so overwhelmed with the decision-making process, that even after that week there needs to be almost another session with them to describe the outcomes? Or by the time those seven days have gone by; they for the most part, have their decision already. [00:14:00]
Kathy Wood (guest): Yes, I think it’s kind of half and half really. We have a lot of patients that don’t need the whole week, and they contact us after a few days, and then we have others who we reach out to, and they feel that they’re not ready. They’re still confused. They want another discussion. And so, we will follow up with another appointment to discuss more issues. Oftentimes they’ll ask, “If I only could talk to a patient who’s had this experience, who’s had a left atrial appendage device implanted” and we can connect them with that.
Often our patients will volunteer to talk to other patients, and so, it’s kind of a variety of options, but we can let them go until their next appointment and follow up with that discussion. It just really depends on the severity of the patient’s condition.
Geralyn Warfield (host): Kathy, thank you so very much for sharing already today so much great information about how to activate AFib care with our patients. [00:15:00] We’re going to take a quick break and we will be right back.
Geralyn Warfield (host): Welcome back to our audiences as we continue our discussion about strategies for activating AFib care for our patients. We’ve been discussing how shared decision making is a very important part of the process of AFib management and AFib care for our patients, and I’m hoping we can pivot now to discuss the risks associated with untreated or undertreated cases of AFib and how shared decision making might address these patients.
Kathy, could you take that as a question, please.
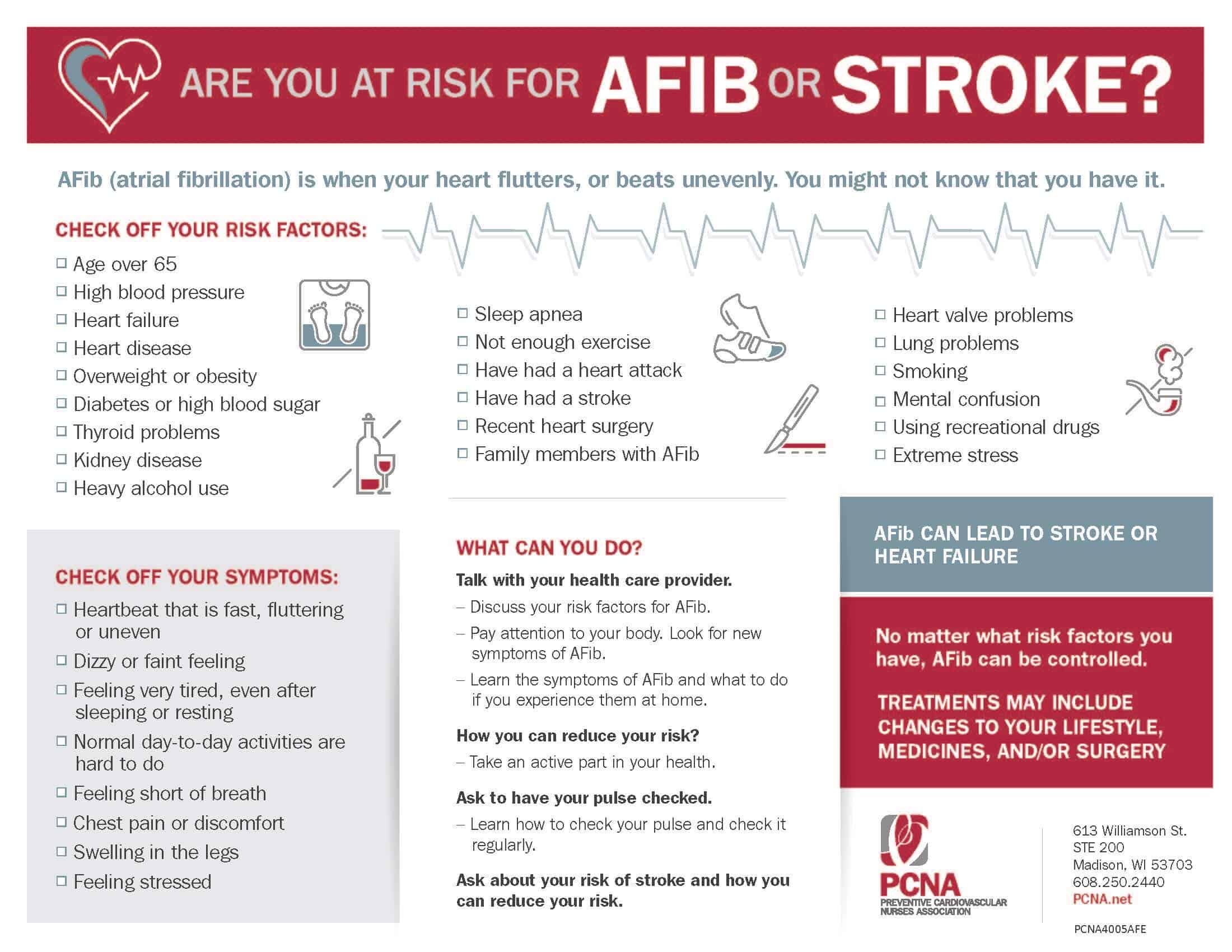
Kathy Wood (guest): Sure. I could start with the undiagnosed maybe, as a first category. We found, through research evidence that targeted screening for AFib is important and very effective. Whereas screening for AFib in the general population has a very poor yield.
So targeted just means it’s directed at those patients who [00:16:00] have risk factors for atrial fibrillation currently. Such as being overweight, and that’s a BMI greater than 27. Patients who use alcohol. Patients with obstructive sleep apnea, hypertension, diabetes, who might be sedentary with low physical activity or who have coexisting coronary artery disease or heart failure, either reduced or preserved heart failure, and then chronic kidney disease with GFR rates of less than 60.
So those patients are at risk of AFib. So, screening for those patients is really important because they’re, especially if they’re older age, over 70 years of age, 10% of the population has AFib. So, there’s so many more ambulatory ECG monitors now that patients can wear from two weeks for up to 30 days, very unobtrusively under their clothes. [00:17:00] And so their adhesive monitors that stick on the chest. Or there’s ones that you can use your fingers to use and there’s an app on the phone and it saves a jpeg recording of the arrhythmia.
So, we’re so much better now at capturing AFib burden or finding AFib in patients. And no one, or certainly there are some that are still using 24- or 48-hour Holters, but they don’t capture very much. So, the longer you monitor AFib, the more you find. So, we’ve come a long way from Dr. Holter’s initial work in 1947, developing the Holter monitor.
I think, in those patients, once it’s found, then they get in the system, and they’re treated. And a shared decision-making could happen.
But for those who are undertreated, I think that’s really where the shared decision-making can [00:18:00] help. Because often, certain types of patients, younger patients or older patients, physicians are hesitant to treat because they don’t think AFib is either, in the younger patients, too severe or dangerous, or, in the older patients, it’s too risky to use oral anticoagulation. And so, they are afraid that the patients may fall and cause an intracerebral bleed, or a hip fracture and bleed that way.
So, there’s a hesitancy. In fact, there was a recent study that showed only 21% of consecutive patients at a center, mean age in this group was 79, were hospitalized with a stroke or TIA and had preexisting AFib, weren’t on anticoagulation. So that’s really disappointing that we’re so far behind guidelines for giving older people [00:19:00] anticoagulation.
There was an old study, and I can put this in the show notes as well, from 1999 that used a Markov decision analysis model and they looked at evaluation anticoagulation for patients that had AFib that were older than 65 years old. And they found that patients who were at risk of falls had to fall greater than 295 times a year to make the merit of not anticoagulating them worth it.
So, you really do need to do a CHADS VASc score and a bleeding risk score, such as the HAS BLED. But there’s other bleeding risk scores you could use, to kind of quantify the patient’s risk of stroke and their risk of bleeding, and that’ll guide providers to make the correct guideline driven choice for oral anticoagulation in older patients.
Geralyn Warfield (host): You’ve discussed using the CHADS VASc and HAS BLED scoring [00:20:00] systems to assess the risk for our patients. Is that a one-time type of assessment or is that ever repeated for those patients that might be at risk?
Kathy Wood (guest): That’s a great question. I think, in current practice, many centers consider that a one-time assessment. But in the guidelines, it says we should be doing this at every visit with a patient who has AFib. Either evaluating their risk of stroke before they’re put on anticoagulation, in order to put them on anticoagulation. Or after they’re on anticoagulation to evaluate their risk of continuing with that therapy and their risk of bleeding.
So, it should be done at every interaction, but unfortunately that’s not done routinely in clinical practice.
Geralyn Warfield (host): And particularly for our patients that have heart failure or venous thromboembolism, are there any additional considerations that we need to [00:21:00] have when we’re looking at their risk for AFib?
Kathy Wood (guest): Yes. Patients that have preserved heart failure, HFpEF, have a real high incidence of AFib and that’s often more common in women. And so, those are patients that are perfect for shared decision-making interactions because sometimes they’re hesitant and they just need to be given permission that they can share their preferences and values for their goals of treatment and whether they want to continue on antiarrhythmics or rate control or anticoagulation, all of those options. But the main thing with patients who have both heart failure and atrial fibrillation is to keep them out of atrial fibrillation, because the more they’re in it, the more it will lead to episodes of heart failure.
So, if their ejection fraction is less than 40, it makes it a little [00:22:00] trickier about prescribing antiarrhythmic drugs. But we found that antiarrhythmic drugs, certainly from the EAST trial that came out last year, the earlier you use antiarrhythmic drugs, the better off the outcomes are, and people stay out of AFib, more frequently stay in normal sinus. So that would be great for heart failure, but it’s often difficult because their ejection fractions are lower than 40 and that limits your options for antiarrhythmic drugs.
Geralyn Warfield (host): Thank you so much for those additional details for those specific patient groups. I’m wondering if a listener has any interest in finding more information about AFib or any other part of our discussion today. Do you have any great resources that you could point them towards?
Kathy Wood (guest): Yes, there’s several I’d like to mention. There’s an article that I’ll put in the show notes from the Journal of Cardiovascular Electrophysiology that just came out [00:23:00] last month, in September, and it examined hospital webpages for how accurate the information was that they provided to the public. It was a public facing website about atrial fibrillation ablation, and the systematic review found that only 33 of 487 webpages from over 4,000 hospitals provided accurate claims about AF success rates and the potential complications. In a small minority, 3%, the authors found had misleading or overtly false statements saying that AFib was a cure. It’s a really interesting article about making sure we’re putting forth the accurate information and facts and success, and limitations of treatments such as AFib ablation.
There was an article recently in the Wall Street Journal about patients that come to the electrophysiologist with [00:24:00] their Apple watch, telling them that they have AFib and how should they be treated. And the Apple Watch is found to have a very low accuracy rate for AFib, but it does tip off the physician or nurse practitioner that that patient maybe should be monitored for up to two weeks or 30 days to see what’s going on in a more accurate way, especially if they’re patients with any of the risk factors I talked about earlier.
The University of Colorado has a fabulous shared decision-making website, and that’s www.patientdecisionaid.org. With a lot of overviews of how to do shared decision-making, different aid worksheets, booklets, a video. Also, all of these are in Spanish as well, which is really helpful. They have grids on it, and that’s the one I talked about earlier that we use with [00:25:00] hearts to represent how many people are affected by stroke per year that can help with decisions.
Also, the Ottawa Hospital in Canada has a great website about shared decision-making, the process of shared decision-making and decision aids. Dartmouth also has a center for that, for that with a great website.
And for patients, “My AFib Experience” that the American Heart Association sponsored, has multiple educational resources for patients in online AF support group that’s monitored by a professional, where patients can ask questions and share experiences. That’s been really helpful for us to refer patients to, and they come back much more knowledgeable and certain in their decisions.
As well as the stopafib.org website, which is great. I’m sure that’s been mentioned before, in your podcasts.
Geralyn Warfield (host): We have had a rich conversation about our [00:26:00] patients with AFib today, but is there anything else that I neglected to ask that you would like to share?
Kathy Wood (guest): No, I just wish people luck. I think starting shared decision-making can be a little overwhelming, but if you work together as a group to come up with a process, and a template that makes documentation easier, it becomes a lot less arduous.
There’s two studies also that are ongoing now about shared decision-making that might be of interest to the group. One is called ENHANCE-AFib, and that’s looking at the benefits of using an online AFib decision-making tool That’s run by the NIH. And a second trial is run out of the University of Colorado and they’re looking at centering patient decisions and shared decision-making interactions based on the CHADS VASc [00:27:00] score for that patient. So, you score the patient with the risk score and then go into the shared decision-making interaction, which may limit or broaden the options for that patient to consider.
So those two studies are going on now, so stay tuned for results from those in the future.
Geralyn Warfield (host): We are so incredibly grateful to our guest, Kathy Wood.
We’d also like to thank Bristol Myers Squibb – Pfizer Alliance for their unrestricted grant for this particular podcast episode. This is your host, Gerald Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Atrial Fibrillation
- Lifestyle and Behavior Change
Published on
October 18, 2022
Listen on:
Related Resources