Effective strategies for maximizing both inpatient and outpatient cardiac rehab are discussed by guest Jonathan David, MSN, RN, EBP-C, CCRP, NE-BC, AACC. Highlights include using a team-based approach, engaging patients in shared decision-making, providing a continuum of care that maximizes patient outcomes, and advocating for cardiovascular care.
Episode Resources
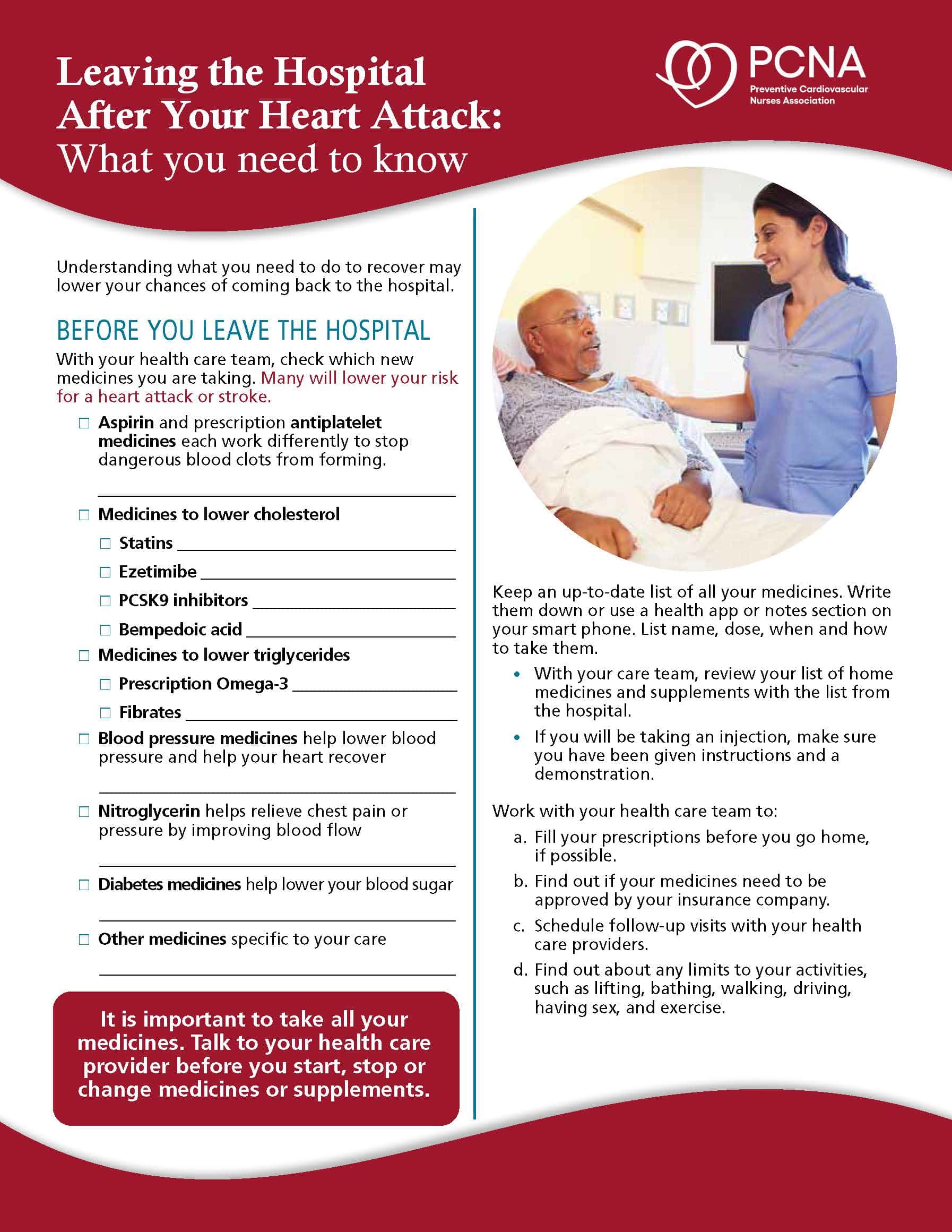
- PCNA Patient Education tool: Leaving the Hospital After Your Heart Attack
Jonathan David podcast episode transcript
[00:00:00] Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to today’s episode, where we have the great opportunity to speak with Jonathan David. Jonathan, I’m going to have you introduce yourself to our audience please.
Jonathan David guest): Hello, Geralyn. Thank you so much for having me. It’s always a pleasure, doing podcasts and talking about the things that excite me. I’m Jonathan David. I’m a Nurse Coordinator at the inpatient cardiac rehab at the Stanford Healthcare Cardiovascular Health that is in Palo Alto, California.
Geralyn Warfield (host): Well, let’s start our conversation today with a single question, which is, what does it take to have successful team-based care in inpatient cardiac rehab [00:01:00] settings? I realize that our time is limited. We could probably spend a semester or longer on this, but I appreciate you trying to put it in a nutshell for us today.
Jonathan David guest): Absolutely. There are two concepts that I want to dwell on. One is, what is inpatient cardiac rehab? And what is team-based? I think team-based is pretty common knowledge. I will first talk about the settings.
Inpatient cardiac rehab is for patients who are within the hospital, that are hospitalized. So, the team—it is called as Phase 1 cardiac rehab or inpatient cardiac rehab—where immediately following a cardiac event could be a heart attack, could be a cardiac surgery, could be as simple as a chest pain. Whatever the course might be for the patient and the accompanying family, the inpatient cardiac rehab team meets them, right?
So, that explains the geography setting.
Now, what is it to have a [00:02:00] team-based setting and how can it be successful? I mean, there are two groups in it. One is internal, where the team that is going to meet with the patient and for it to be successful, those are stakeholders that we want to make sure that the internal team are aligned with the common goal, the workflow, the dependencies that are there between each of us as colleagues that we want to make sure this is how we are going to meet the plan of care for a particular patient. And then what barriers are there?
Now, see that and apply that to external stakeholders. Because you cannot be a team just being within the team itself. There is a lot of relationships, which I’m going to talk about, which also goes with stakeholder. Now, who are the stakeholders? That’s transdisciplinary, from physicians to advanced practice providers, to even the family, extended family and so forth. [00:03:00] Think of anyone in the hospital that overlap care. Those are team members as well.
So, to summarize, there is both internal and external. For it to be successful and team-based, I think it has to be cohesive, that everybody knows what was needed for us to provide a successful team-based care.
Geralyn Warfield (host): So, in terms of that external-looking organization, in terms of looking outside of the workflow and really, we’re looking at families looking at the patients themselves, looking at caregivers. How can you successfully partner with them on secondary prevention strategies?
I think sometimes that might be a lot more complicated than working internally because maybe your communication is not very regular. Maybe there might be a language difficulty in terms of them understanding what’s going on. And there might be a trust issue. So, how can you address all those kind of barriers or challenges and work with families [00:04:00] successfully on that secondary prevention?
Jonathan David guest): What a wonderful question, Geralyn. You know, you hit upon what is at the center of everything that we do.
I heard many years ago from a patient and I asked this patient, “Can I share that when there is a moment such as this?” And he said, “Yes.”
If it is about me, then there’s nothing without me.
Meaning if we are going to talk about a patient and their plan of care, then if the patient is not in it, then it’s of it is of no use because it’s all unidirectional.
So, what does it take to partner even before we go and complete with the partnership? It takes active listening. And it takes, silence, allowing them to express what their needs are what their concerns are, what is it that they want to achieve, what is it that they want to see in their [00:05:00] care. And at times, as the providers, we listen, or team members, we listen.
We want to anticipate their needs. We want to anticipate the barriers. We want to anticipate the complexity that they will face. Now, that’s where the trust begins. When the patient and the family feels that we are able to listen and really listen actively and restate what they’re asking, and making sure that we have, that I have or we have, understood it clearly what they meant, and build on that.
So, we are starting from what they know we can’t build medical knowledge, or procedural knowledge, or any information on the plan of care without building on what they already know. So, that’s very critical to build on that.
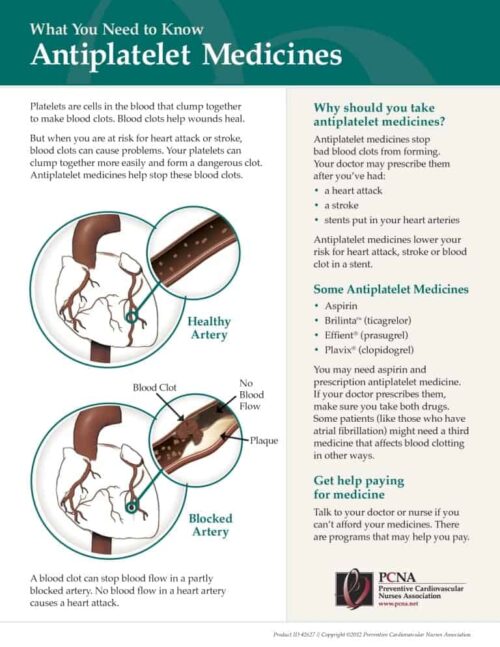
Now, there are many tools I want to mention from PCNA. There are many tools for patient decision-making, a lot of educational tools. We want to use that as [00:06:00] shared decision-making. Take a procedure, take a cardiac event, disease or disorder. We have tools that we could use, and show to them, “And this is what it is.” You could read upon it, ask questions, and you can circle back with them. So, you build on.
So, what we are trying to do is an active shared decision making, through patient decision needs. So, thus, you know, there is many approaches we could take in building on the partnership, but this is where we could begin and build on.
Geralyn Warfield (host): We’ve been focusing thus far on patients, families, caregivers, and kind of the external part of the team when it comes to team-based care.
I’d like us to revisit what it takes to have an effective team within the clinical or the hospital setting. In that inpatient cardiac rehab setting where an individual has had an event. What does it take from a healthcare professional standpoint to be effective in that [00:07:00] setting?
Jonathan David guest): Great question. I’ll talk from the angle of the inpatient cardiac rehab team.
The team members should know the patient. That would involve getting to know the patient’s history, the complications, or what procedure they went in. And often, patients don’t have any complications and at times there are complications. So, to be fully aware and not be surprised that the patient, or the family member, had to inform the team member.
So, being thorough on what the patient’s reason for the hospitalization is, and what procedure they went, and where they are in their recovery phase. That is a starting point. So, you’re well and you’re grounded in your knowledge about the patient.
Additionally, there are team rounds. I think every facility, every organization have team rounds. So, it’s important for the cardiac rehab team [00:08:00] members to be attending the team rounds to understand and get input from the other teams and on what the plan of care is, so that will help them to support, be aware and look for. Sometimes we may quickly discharge a patient like, okay, we have done our part, but at times there is a need that we need to go back and support them on that need. So, being up-to-date, on every day, attending the team rounds is important.
So, these are two fundamental workflow, a part among many, this is crucial to be successful.
Now what is, I mentioned earlier about other team members who play a big role in making…those swim lanes are: we are not isolated, we are working together. And including the successful parts or engagement of the other team teams, we are [00:09:00] able to now, you know, get to the part where the patient ,we are preparing the patient to have a successful hospital stay, and we are looking forward for them to be transitioned to home, or care and community.
Now, what is important before they leave?
From cardiac rehab standpoint that they have received the education. We, in our team, we provide an hour of consultation, talking all about what about the disease or disorder? Knowing the patient has understood what this involves, what procedure they went through, and if they have understood what is their recovery, what should be their, you know, activity patterns. What is should be their ADLs, what they should do, what they should not, what they should watch for, what reasons they should call us back, or when they should seek urgent care, or go to the emergency department, or call 911.
So, providing them, and then providing them [00:10:00] tools to self-measure that they could chart down their activity. They can chart down their blood pressure, their heart rate, their daily weights. So, these are, important resources or materials that the patient should have properly a written a book where the patient could write for themselves, or family members can write for them.
So, having done that, the critical part for cardiac rehab, inpatient cardiac rehab, is the patients are educated, and they’re referred before hospital discharge.
Here again, a shared decision-making. The cardiac rehab referral should happen before hospital discharge. This means the team member has discussed with the patient and family is the cardiac rehab. Why you need cardiac rehab? How soon you should go to cardiac rehab? What happens in cardiac rehab? How it benefits you and what outcomes are we expecting overall. And cardiac wellness. Not only recovery to health, but also, overall cardiac [00:11:00] wellness.
So, we want to make sure that patient and family has understood that, and provide them the resources about cardiac rehab and find out which location is the convenient location for them. Here, the patients may have to go two to three visits a week. So, we don’t want them to be driving more than an hour to a location: find the nearest location, So, that is a shared decision-making, and then send the referral to that facility.
And a step further, connect with the facility at the outpatient cardiac rehab, and see if we could get a first visit scheduled so they could get their intakes done by the team at the outpatient clinic and they have their first appointment. So, that way we can enroll them early and have them participate at an early stage.
Geralyn Warfield (host): We’ve been talking about inpatient cardiac rehab with Jonathan David. We’re going to take a quick break and we will be right back.
Geralyn Warfield (host): We’re back [00:12:00] speaking with Jonathan David about cardiac rehab. And just like our patients transition from inpatient to outpatient, our conversation is going to do the very same thing.
So, as we focus a little bit more now on after our patients leave our inpatient facility, what are some qualities or some strategies that need to happen beyond what we’ve already discussed, perhaps, to make sure that we can in ensure improved patient outcomes after that hospital stay?
Jonathan David guest): Great question, Geralyn. Now for making sure the patients have improved outcomes and they’re not coming back to the hospital right away, it’s important that they have the contacts I earlier mentioned about the resources that the patients have. One more thing to add to it is they know who to contact, for what to contact, when to contact. These are clear details that [00:13:00] should be provided for the patients and the family.
And those contact numbers are readily accessible to them. Not buried somewhere in some kind of pages but upfront so that they could really reach out.
Now from the provider, from the team, what is to help, and help them with the continuity of care to have successful outcomes? We have, when we met with the patient, we had goals laid out for them.
So, when we laid out goals, these goals are not me as a team member laying it for them. As we went through discussing and engaging them, we listed out what risk factors are, and how we could turn them around, how we could improve towards recovery and health, and cardiovascular wellness. And these goals are laid out.
And having the patient’s engagement in what should be the goal? And how should we measure it? And having the kind [00:14:00] of a soft agreement. And by what timeline? And what if this is not happening? What resources do you have, and who should you contact? And making those contacts or referrals.
So, these things are, you know building blocks for us to have successful outcomes. Because without which reaching or improving successful outcomes, it is going to be hard because there is discontinuity in workflow or process to care. So, if once the patient has gone home, a follow-up phone call is a great way to connect with them and say, “Hey, Mr. Jones, how did things go? Hope you’re getting better. Were you able to do your walks? Did you check your temperature? How is your blood pressure going? Are you taking your medications? Kind of you know, each phone calls have a list of questions to ask and making sure we have that process or standard workflow to follow up on [00:15:00] questions.
Upon connecting with them, again, using the tools of active listening and anticipating any needs that have been missed out earlier, and coordinating.
Care coordination is a huge topic. We could go on hours the many levels of care coordination, but that is key for successful outcome. Once we are able to coordinate, or make secondary referrals and additional referrals, so that the patient could be seen by the specialist and team, we are able to provide everything that we could at this time to the patient, and empower them towards the successful outcome.
And asking them if they don’t see progress, and giving them tools if these symptoms, or if you don’t seem to progress, then you need to call us back. So, kind of reassuring them with those information.
So, these things, put together comprehensively, would help us in improving patient outcomes. Making sure those are measured and by timeline, and [00:16:00] validated by the team members—either internal or external—helps us to be on track.
Not to forget, the providers on the inpatient, the teams in the hospital in supporting continuity of care should send or should be able to send the relevant medical records to the family care physician, a PCP, or the specialist, or the cardiologist and the outpatient cardiac rehab.
The documents, the care records, the labs, investigations, and the referral details and all those, paperwork to be sent over in a timely manner so that the continuity of care can progress quickly. Or else we face situations…there is a lot of waiting period where we lose [00:17:00] patients. And that’s not helping in improving patient outcomes as quickly as we can. So, making sure the health records are reaching the teams simultaneously as we coordinate care.
Geralyn Warfield (host): Those are all exceptional thoughts and things for us to apply in clinical practice if we aren’t already.
We initially talked about team-based care in the inpatient cardiac rehab setting. Team-based care continues throughout this process for the patient, and the team may change a little bit from the inpatient to the outpatient, but I love the fact that you talked a little bit about that continuity of care and how it’s important that people are not lost as they transition from one to another location or set of healthcare professionals, or anything like that.
So, thank you for, reinforcing that for us because sometimes I think that’s the easiest thing for us not to do because the next crisis, of course, the next patient is right in front of us as we’re trying to follow up with the patients that we’ve just seen.
[00:18:00] I’m hoping that we could talk a little bit more about advocacy and as healthcare professionals, how we can effectively advocate for cardiovascular health.
Jonathan David guest): Advocacy to cardiovascular health is a huge topic. And for this context, I want to mention about early detection.
Patients and families should know when there is a sign of illness or symptom. They should visit a provider’s office and have them evaluated and screened. Primordial prevention—even before any form of disease or disorder takes place, they should be able to engage in healthy lifestyle to prevent onset of any illness or cardiovascular illness. Primary prevention and secondary prevention, so, the tertiary prevention—there are levels of prevention now.
I think one great tool that we could lean on is the AHA’s Essential Eight which sums it all up. I like that tool very much, and I [00:19:00] share that with my patients as well.
The first one is eat heart healthy diet.
Number two: get at least 150 minutes of moderate intensity activity, or 75 minutes of vigorous intensity. And this is not for all. So, I often encourage, “Listen to your body and we don’t want injury related to physical activity.” But listening to our body, one’s body and progressing physical activity is a great way to remain physically active.
Avoid smoking or vaping or secondhand smoking.
Aim for seven to nine hours of sleep.
Maintain a healthy body weight.
Keep your fasting blood sugar less than a 100 mg/dL, or A1C less than 5.7.
Know your numbers. Keep your lipids or cholesterol [00:20:00] numbers in normal range.
Keep blood pressure systolic less than 120/80.
So, these are great way to, you know, advocate for heart health and cardiovascular wellness.
Geralyn Warfield (host): I have one final question for you. We have covered a lot of topics today and I’m hoping that you’d be able to identify one key takeaway that you would like our listeners to consider as they finish listening to this episode.
Jonathan David guest): Thank you, Geralyn. I think team-based approach., patient-centered, and engaging patients through patient decision-making is key.
Geralyn Warfield (host): Thank you so much, Jonathan David, for spending time with us today, speaking about cardiac rehab, speaking about advocacy, and encouraging us to be active participants with our patients in this journey that they take, from inpatient to outpatient cardiac rehab and beyond.
This is your host, Geralyn [00:21:00] Warfield, and we will see you next time.
Jonathan David guest): Thank you very much, Geralyn. Thank you for having me.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Acute Coronary Syndrome (ACS)
Published on
April 2, 2024
Listen on:

MSN, RN, EBP-C, CCRP, NE-BC
Related Resources