What is the role of a nurse navigator–whether or not that is your job title? Guest Susan Bush, RN, BSN, CCRP, FPCNA, describes how these individuals can help patients with heart failure and other diseases find information, resources, support, and much more.
Episode Resources
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to today’s episode where we are speaking with Susan Bush. Susan, would you please introduce yourself?
Susan Bush (guest): Hi, I’m Susan Bush. I am a Registered Nurse and have been for quite a number of years–40 plus (I’ll just put it that way). I’ve been blessed to have this profession. This has been just an amazing journey. I wouldn’t have changed anything about it. I started out in pediatric care many, many years ago.
And then I transitioned into cardiac care and a lot of my career has been in cardiac rehab. I love cardiac rehab. I love watching the patient from the day we pick them up out of the bed, [00:01:00] literally, after their surgery or their MI, and we walk with them.
And then watching the progression over the next, you know, 12 weeks or so of getting them back to doing what they were doing before exercise-wise or, you know, starting an exercise program—maybe they never did that before. That is such a gratifying job. I love it. [In the] last five years I have been working as a Heart Failure Nurse Navigator. That’s a bit of a different role, but I have really enjoyed it.
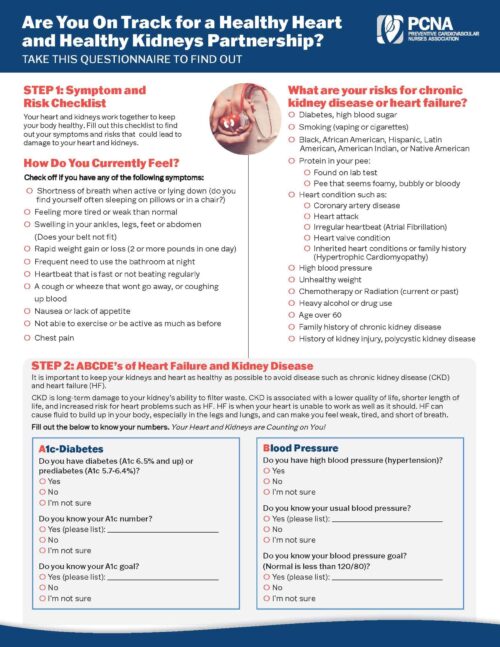
I am helping this really troubled population through the ins and outs every day of their new life with learning about their, you know, sodium and their diet. Learning about how to monitor their fluids, learning how to just watch their symptoms and what to do about them. And being there is a support for them that has been very gratifying. It’s a different population and sometimes you don’t have the outcomes [00:02:00] that you know are as positive as you might in a cardiac rehab program, but it is still gratifying for me because I’m helping them through this very difficult time.
And some of these people are brand newly diagnosed, some are not. But you know, some of them; it takes time. You know, you may have to work with them (on) several different occasions, different encounters to try to help them to understand what they’re dealing with, and how they have to work on this every day.
They don’t get a break, and they call me, they ask me questions, I develop relationships with them, which for me, that’s a big part of it. I’m a kind of relationship kind of person. And so, I am working with heart failure patients. I think that nurse navigation really is the way to go with many different diagnoses.
Geralyn Warfield (host): So, let’s dive in a little bit deeper to that Nurse [00:03:00] Navigator role. What types of activities, what types of things are you doing as a Nurse Navigator to help these patients in that long-term success route?
Susan Bush (guest): Well, it starts out with me meeting with them when they’re inpatient. And I do, education with them, of course, about heart failure. The AHA ‘Get with the Guidelines,’ you know, requires that we do about 60 minutes of education with them. So, I have a good bit of time to kind of introduce some principles with them, and then after that, I do phone follow up with their permission, And I usually do once a week for about 30 days, but in some cases it’s more than that, you know, if, if they have a lot of needs.
You know, I have some people that are alone. They don’t have anybody else to talk to, they don’t have anybody to help. So, you know, I will, you know, maybe I’ll call them twice a week. They also have my number—my work phone number—and they [00:04:00] call me if they have questions.
And I tell them, you know, I’m clear with them. “These are non-urgent questions. If you think of something in the middle of the night, call and leave a message and I will get back with you when I get in in the morning.” And so, you know, it’s, it, in a lot of cases it’s a great relationship.
And, so we, you know, I support them with all of the educational aspects of this. Their medications—that’s a huge thing. And you know, we’re starting these people on multiple medications. You know, our goal is to get them on probably four or five medications. We may not start that, you know, right away in the hospital. But you know, that’s our goal.
So, I help them to understand that and that, you know, this is a process. This is not going to just be, “OK, here’s your meds, go home.” This is a process. Getting their follow-up labs done, getting their follow up appointments, making sure they’re not missing those. Those are the conversations that I have with them over the phone [00:05:00] when, you know, I make those weekly or, you know, twice weekly calls.
Then as they start to get a little stronger and kind of get used to some of the things we’ve talked about, then we start talking about exercise. And you know, potentially, if they qualify, getting them into a cardiac rehab program. If not, you know, we have great educational materials at my institution and so, you know, I refer them to the guidelines that we have in our book about exercise and we talk about that.
And you know, as you can imagine, there’s people on all ends of the spectrum. Some people are very big in to exercise already, so, I help them to understand, you know, how they can resume that.
I also, you know, work with people that have probably not exercised much at all in their life. So, we just start out with walking, and we do what we can, and we go through symptom limited activity. We go through all the things to watch for symptom-wise.
So, you know, [00:06:00] it’s, it’s a lot. And, and the discussion, a lot of times the discussions, are led by the patients. Because I don’t want to, I don’t want to just sit and spew information at people. That, that’s not my, my style. I don’t think that that’s the appropriate way to educate adults. I think you have to let them lead in that process. And I answer their questions because to me, if they’re going to ask me a question, that’s something they want to know, and I’ll answer it. And, you know, then they, they’ll, they’ll probably remember that.
But you know, we have to be cognizant that, you know, a lot of what we tell them, they’re not going to remember. So, repetition is a big part of it. And sometimes you see the light bulb go off, you know, and those ‘Aha!’ moments, and, and that’s always great.
Sometimes you have people that, you know, that don’t either, for whatever reason, they don’t adopt the recommendations and then, you know, well, we’re going to see them again. And we [00:07:00] do. And you know, I just gently approach them and just say, “Hey, what, what do you think’s going on?” You know, “Tell me what happened. Tell me what’s, you know, what do you think you maybe could have done a little differently?”
I don’t, you know, I don’t do any preaching. I mean, it’s so counterproductive in my mind. And so, it, it’s just that, again, I keep harping on it, the relationship. I think that’s a huge part of being a Nurse Navigator.
Geralyn Warfield (host): We all recognize that heart failure is a very scary diagnosis, and it’s also a very complex disease to manage.
And you have given us some ideas of what that’s like to try and share with patients over time, rather than talking about diet, talking about emotions, talking about exercise all at once when they may be just initially just trying to come to terms with the diagnosis itself. “What does that mean? How does that affect me? How does that affect my [00:08:00] family? Am I going to be able to work?”
All of the emotions, all the thoughts that are going through their heads. So, if you are building this relationship with these patients, how much information are you providing at any given time? Do you—and I heard you say that you are focusing on the questions that they ask you—but sometimes I think maybe they don’t even know that they need to know something. So how do you bring up topics like that?
Susan Bush (guest): So, before I make a phone call, I usually will review my notes, you know, from previous discussions with them, and I’ll make myself little notes about what I think we need to talk about at this given time. We may or may not get to that depending on what their concerns are at that moment, you know.
But those things that, that I discussed already, you know, the, the biggest thing is watching the sodium in their diets. You know, making sure they’re not drinking, you know, copious amounts of fluids. Weighing themselves every day, [00:09:00] exercise, and then the, you mentioned this, the, the psychological effects of this. I mean, it’s sometimes they just need somebody to talk to.
And we offer—I work for University of Colorado Health System in Colorado—and we offer a lot of virtual classes across the system. And we’ve, we’ve just recently made all of those classes available to all of our, our Colorado patients. So, you know, they have plenty of opportunities to get more in depth, you know, support and education if they choose to do so. Primarily like with the diet, a registered dietician.
But we have, we have a nurse practitioner who works in our heart failure clinic, and she does a presentation on heart failure symptoms and what we do about them. We have an exercise physiologist that presents on exercising with heart failure.
We have a [00:10:00] pharmacist that presents on, you know, the medications, which are myriad and important. And she does a great job with going through them all.
And, and then we have psychosocial kind of situations. You know, we have people that present about, you know, dealing…there’s also a support group that’s being run by one of our sister hospitals in, in the Colorado Springs area. So, they have opened that up virtually, so that people can join that support group if they wish virtually. Even from, I’m in the northern part of the state, so even from, you know, the northern part, they can do that.
So we, we also have somebody that in our northern part of the state talks about community resources. There’s a lot of those. And I think sometimes these people need that, and they can’t get out and clean their yards up anymore. They can’t, you know, do even their housework, you know, things like that. So, there’s resources for that. [00:11:00].
And then we also address advanced care planning. You know, not everybody’s in end stage, of course, but it’s just a good opportunity to introduce, in some cases, that subject to people so they understand that, you know, this isn’t that we think they’re dying, this is, you have the right to put in writing what you want for your life. And then we will abide by that. You know? And so that’s how we approach it and I think they, they get that, you know, I think they understand it and appreciate it.
Geralyn Warfield (host): We are going to take a quick break and we will be right back.
Geralyn Warfield (host): And we’re back talking with Susan Bush.
And Susan, I know that your job title includes Nurse Navigator, but what would you offer for our listeners who perhaps don’t have that as their job title, or maybe there’s not that role at their institution. What can we do to assist in this relationship building that you’ve described?
Susan Bush (guest): It’s a challenge.
I mean, we’re talking primarily, I would assume, [00:12:00] about the bedside nurses that work on the units. You know, they have the patient maybe, you know, 24 to, you know, maybe 72 hours. With heart failure diagnosis, sometimes it’s a little longer, but because, because we’re trying to diurese them and that takes a little time, you know?
But that is a huge challenge, trying to get them up to speed on what they should be teaching the patients.
For my system, my health system, we have developed in Epic (our electronic medical record) we’ve developed some tools that have hopefully been helpful. We have the Heart Failure Education book that we’ve developed, and they have access to all of that.
And I encourage, especially new nurses on our cardiac unit, if they want to come in and just sit in when I talk to a patient, I’m always encouraging that, and I think that’s been very beneficial.
I think they just don’t [00:13:00] realize the depth of what these people are going through and what they need. And they’re busy and I understand that, but you know what you’ve brought up is definitely a challenge because we have a couple of hospitals nearby where I work in Loveland, that don’t have Nurse Navigators. And I can see the difference. And our nurse practitioners in our cardiac clinic are always calling me, you know, “Can you, can you follow this patient?” because they’re at a hospital where they don’t have, you know, that education and support. So, and I have no problem with that, but we’re working on that.
You know, it’s, you know, it’s a big role and, you know, it’s, you know, health systems. It’s hard to get, you know, FTEs approved for new things. But I am gratified that in the, at least in the northern region of my health system, this has been in place for more than 10 years.
And, and yet some of the other hospitals in our system didn’t have it [00:14:00] until just recently, have the Nurse Navigator position for heart failure. So, I’m hoping that this is a trend. I’m hoping that, you know, as I said earlier, even other disease states. I mean, you know, I know that cancer uses Nurse Navigators because there’s a lot to go through with that, with, you know, the different treatments and such.
But I have really come to love this role, and love being able to help people in that way.
Geralyn Warfield (host): If one of our listeners has questions about nurse navigation, particularly in heart failure, what would you point them towards when it comes to resources?
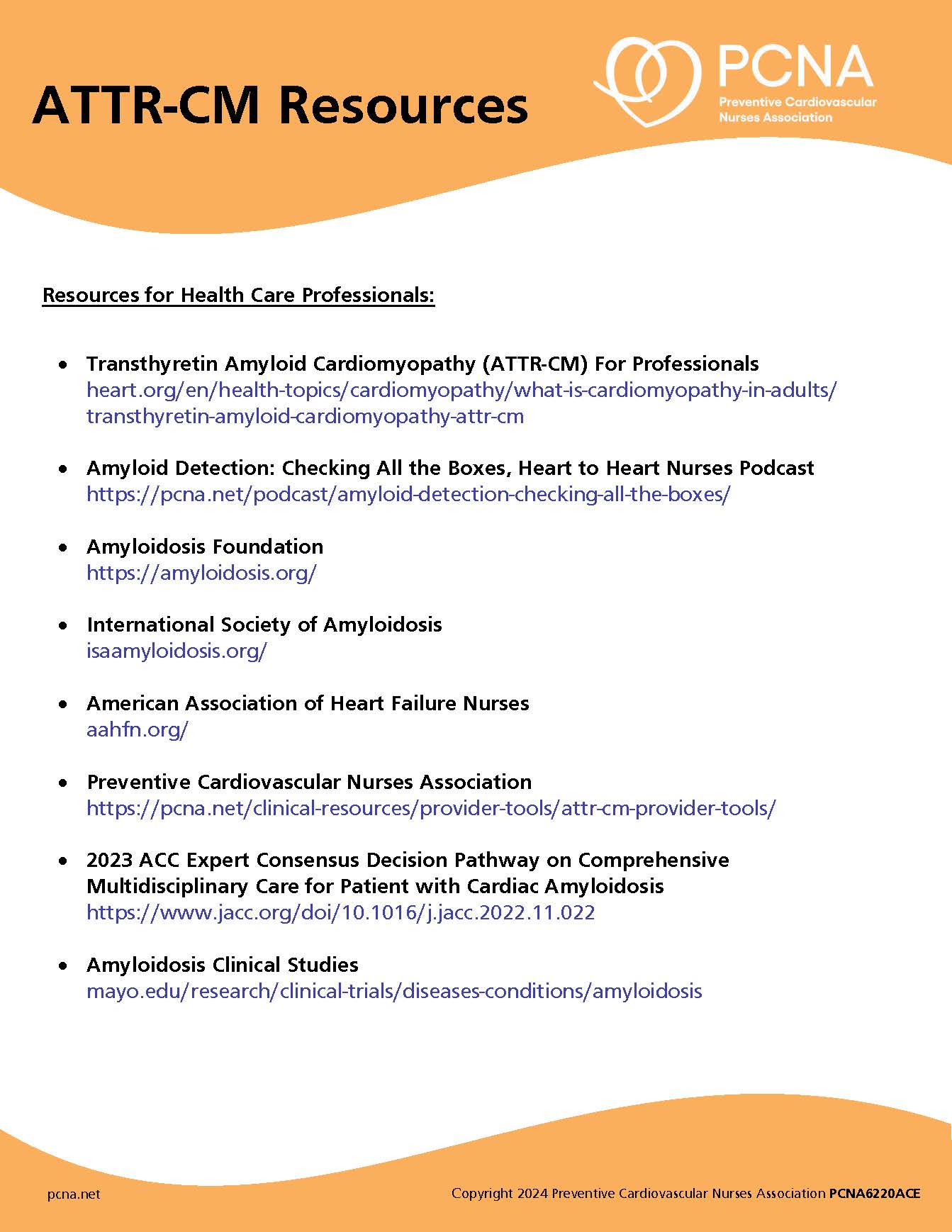
Susan Bush (guest): Well, PCNA has amazing resources for all of the different potential things you would see with, you know, a heart failure type diagnosis. The, you know, hypertrophic, cardiomyopathies, you know, it’s, there’s a lot. So, there’s a lot of, of resources through PCNA.
There’s also the Heart Failure Nurses Association, of which I’m a [00:15:00] member and they have a lot of resources. So, for heart failure there is, there’s a lot out there.
I’m sure that even the government websites and such, you know, would have a lot of resources for that.
Geralyn Warfield (host): Is there anything else that we neglected to discuss that you’d like to add?
Susan Bush (guest): I am a huge proponent of PCNA. I have been a member for I think it’s been 20 years now.
Geralyn Warfield (host): Wow.
Susan Bush (guest): So, yeah. If you haven’t picked up on it, I’m an older nurse. I don’t think of myself as old, but you know, I’ve done this for a long time. And, you know, I’m so appreciative to PCNA for the opportunities that I’ve had for leadership, for project development. You know, the patient education resources through PCNA are amazing—and I’ve been very fortunate to work on a few of those.
And, you know, just the professional development we have. You know, I worked on the behavioral health mini certificate that we have [00:16:00].
And, you know, just all the opportunities. I mean, nursing in general offers so many opportunities. I am a huge proponent of, you know, guiding younger people that I may encounter in this direction because there are so many different things you can do.
And you know, as I’m getting to the point in my career where I’m, you know, probably going to be scaling back, looking at retirement. I am not retiring from nursing. I will keep doing things, I will keep—through PCNA, through other organizations I belong to, you know—I’ll keep contributing. Because it’s hard to not, when you have so much experience and so much knowledge about different topics and particularly preventive cardiovascular care.
Geralyn Warfield (host): Susan, thank you so much for sharing your passion for cardiovascular nursing, for nurse navigation, for ensuring the success of our heart failure patients as they [00:17:00] move from one inpatient setting to wherever they’re headed next.
We’re really grateful to you for your time. This is Geralyn Warfield, your host, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Heart Failure
Published on
January 30, 2024
Listen on:

RN, BSN, FPCNA
Related Resources