Hypertrophic Cardiomyopathy (HCM) diagnosis and management are complicated; symptoms may include shortness of breath, severe arrhythmias, or inability to exercise. Rarely, very vigorous physical activity may trigger dangerous arrhythmias and even sudden cardiac arrest. Centers of Excellence provide best practice approaches to optimize patient outcomes. Guests include Heidi Salisbury, RN, MSN, CNS, from Stanford University, and Carol Patrick, RN, ACNP, from Northwell Health.
Thank you to Bristol-Myers Squibb for supporting this podcast episode.
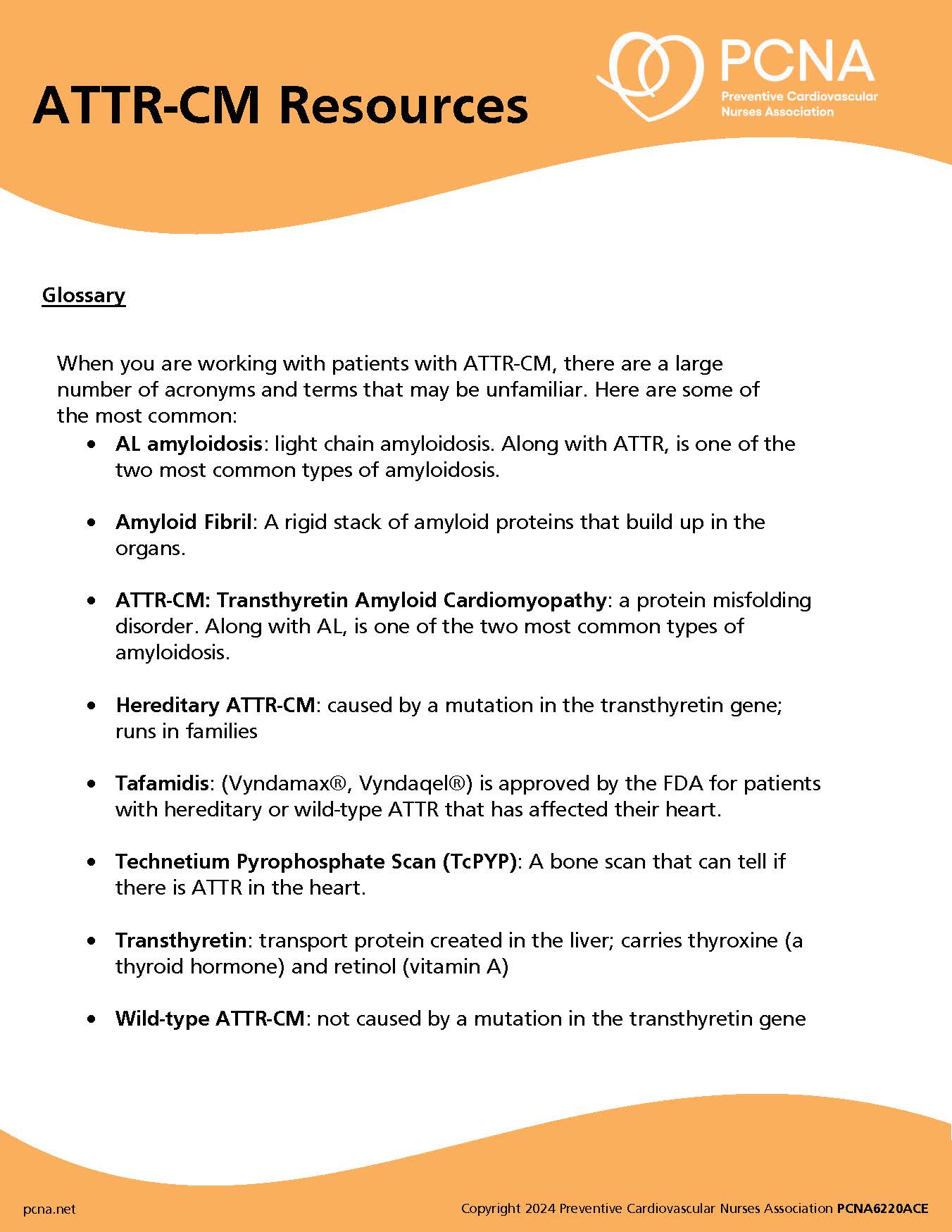
Episode Resources
PCNA (00:03):
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Dr. Eileen Handberg (00:18):
Welcome to PCNA’s Heart to Heart Nurses podcast. I’m your host, Eileen Handberg. I’m currently president of PCNA. I’m a nurse practitioner at the University of Florida in Gainesville and Director of the Cardiovascular Clinical Trials Program. I’m so excited to be here today as part of this podcast series. This is the second of three podcasts that will be focused on hypertrophic cardiomyopathy, which we’re going to call HCM for short. Hypertrophic cardiomyopathy is the most common genetic heart disease in the United States with 1 in 500 diagnosed with the condition worldwide. In HCM, the wall of the heart’s left ventricle is thicker than normal, reducing the heart’s ability to pump blood efficiently. Symptoms of HCM may include shortness of breath, severe arrhythmias, or an inability to exercise. While rare, some people with HCM can have sudden cardiac arrest during very vigorous physical activity, with physical activity triggering dangerous arrhythmias. Diagnosis and management of HCM can be complicated.
An HCM Center of Excellence offers teams of people that promote collaboration and uses best practices around a specific focus area to create positive outcome for patients. Tune into this podcast, to learn more about HCM Centers of Excellence and prevention of the more lethal symptoms that some patients may experience with our expert guests, Heidi Salisbury, and Carol Patrick. Heidi co-founded the Stanford Center for Inherited Cardiovascular Disease in 2006. She’s a clinical nurse specialist, board certified in genetics. Heidi is dedicated to mentoring nurses, genetic counselors, and physicians and fellows, to develop the clinical skills and gain the knowledge base necessary to expertly manage patients with inherited heart disease. Heidi is passionate about training the next generation of providers to think genetically when approaching the care of this vulnerable population.
Carol is an ANCC dual boarded, acute care, and adult nurse practitioner in interventional cardiology, cardiology electrophysiology, for the past 38 years at Northwell Health on Long Island, New York. She’s authored and presented both locally and nationally on cardiology, critical care, sudden cardiac death, genetic channelopathies, atrial fib, and advanced cardiac device therapies. She is a lead nurse practitioner participating in the New York heart screen, a high school-based program for the early identification and detection of sudden cardiac death in our high school athletes in New York.
For this episode, we’re going to take a deeper dive into symptom recognition and advocating to be able to refer to HCM Centers of Excellence. Ladies, in our previous segment, we’ve talked about HCM and how it gets diagnosed, family histories that often help confirm the suspicion, such as sudden cardiac death, car accidents of a family member in the past, with no reason why they would’ve been in an accident. Carol, how do we screen these patients and the patients that present with these sort of vague symptoms for HCM?
Carol Patrick (03:49):
Thank you, Eileen, for posing that question on our hypertrophic cardiomyopathy patients. Essentially what we are going to be focusing on is the unrecognized, those that are asymptomatic, or those that have certain symptoms that we want to take a look at and deeper dive into, to diagnose hypertrophic cardiomyopathy. When we look at the screening that’s utilized, for patients, for HCM, it’s again a genetic disorder. We start really in the young, we start in the lifespan going from the pediatric population, and what we’ve identified is there is a real clear need for clinical education and accurate recognition of certain symptoms. I really point to the American Heart Association, 12-point questionnaire, and what that is, it really encompasses three portions of a patient, to put together a viable screening tool to send them for cardiac referral into a genetic center of excellence for further diagnosis.
What that in entails, is looking at that 12 points of questions, such as in their medical history, did they ever faint or have a syncopal episode, dyspnea, any fatigue associated with the exercise, increase systolic blood pressure? Do they have a heart murmur? That’s a real key piece in physical exam. As we journey through the 12-point questionnaire, the next piece is family history, very, very key component of diagnosing and moving forward with these points that add up. Does the patient have any primary family relative that died of a sudden cardiac death or a premature death that was unknown, less than the age of 50? That’s a clear question on this questionnaire. Physical examination then comes into play, and that’s really taking a look at, obviously if there’s a heart murmur, their personal physical exam, checking for femoral pulses to exclude any sort of problem there, and really getting that stigmata of any Marfans.
Doing the arm span, measuring that compared to their height, and having them listen to heart sounds, whether they be supine, leaning forward, and performing the Valsalva maneuver. What I wanted to share with all of my constituents today, that I’m very excited to be part of, is Duke Children’s, Duke University, has a national pilot study screening form and research program going on. I have had the pleasure, and the honor, to lead the nurse practitioners in the Heart Screen New York Initiative, that’s part of this Duke University initiative. The initiative was formulated and born from two moms whose sons passed away, several years ago, from sudden cardiac death, from hypertrophic cardiomyopathy, on the lacrosse field and the basketball field. What has happened and transpired with this program, we in New York have had the opportunity to go to high schools and perform EKGs, echoes if needed, the targeted 12-point American Heart Association questionnaire being filled out, and then checking their vital signs such as blood pressure, pulse, the NPs, listening for heart murmurs.
Then we have an interventional cardiology team that does the screening overall to see if in fact, this particular athletic student, pre-procedurally, needs to have further evaluation by a pediatric cardiologist. We have had many saves, from New York, from having this program in place. We’re so proud of having heart screen New York, and what has come about as a result of, again, these foundations, from moms having banded together, Parent Heart Watch, and all the organizations from parents that have lost a child from sudden cardiac death, related to genetic channelopathy, such as HCM, is the establishment of Louis’ Law. Louis’ Law, in New York state, was signed in by Governor Pataki in 2002 on the day Louis Acompora would’ve graduated from high school. He was a 14-year-old lacrosse player and he collapsed on the lacrosse field and his parents, watching, and struggling, to figure out what was happening, minutes went by and there was no AED present. I share with you, from this tragic loss, that the Acompora family went further to Albany, and to New York state, in 2002 establishing Louis’ Law, which mandates that every public school in New York state, regardless of age, must have an AED on-premises, as well as an AED accompany, all sporting events from that school. As a result of Louis’ Law, there have been over 3,000 – 4,000 saved lives in New York state.
Dr. Eileen Handberg (09:19):
Wow, that’s very impressive. It shows the power of advocacy. Whether it’s parents, whether it’s the public, that’s impressive.
Carol Patrick (09:31):
Yes, it’s really a heartwarming experience, as well as from a professional standpoint, it really just emphasizes how advocacy is so important. With HCM, sometimes the only symptom that we see is a fatal arrhythmia, such as a sudden cardiac arrest event, and that’s the piece of it that we really need to focus on for education advocacy and teaching our clinicians how to recognize and utilize the 12 point questionnaire, as well as their physical exam, as well as their family history. Knowing when to refer to Centers of Excellence, such as what Heidi has really initiated.
Dr. Eileen Handberg (10:16):
Carol, and Heidi, if you know the answer to this, how widespread is this community screening? We hear a lot of things about this, and more prevalent for screening of athletes in Europe than it is in the U.S. All the calls out that, it affects such a small number, is the cost worth screening hundreds and hundreds of thousands. Obviously, any life lost, but when people talk in terms of public health and costs per screening, where is the U.S. overall? In general, it sounds like New York is pretty progressive.
Carol Patrick (11:04):
In response to that Eileen, great question posed, thank you for that. Again, the most common cause in sudden cardiac death, in the young, is a genetic channelopathy, such as HCM. It’s the leading cause of death on our school campuses, in our athletic fields. 90% of these are preventable. If you ask the Parent Heart Watch members, which are all the moms and dads, parents and siblings, that all lost somebody, they will tell you that we have not done enough and that we need to do more. The screenings that we do in New York are free, nobody gets charged, it’s all voluntary. All of our interprofessional teams come together, we use nurse practitioner, medical students, nursing students, and it’s a daylong event, and it’s all voluntary. It’s funded by all the foundations of the students that lost their lives to sudden cardiac death, and it’s totally free for everybody.
Carol Patrick (12:09):
The network of the mothers and parents is immense throughout the nation. There are centers that do the same types of screenings we do in New York, I know they’re in the Midwest and I know they’re somewhere down south in the Southern states. They have a very strong network. Again, it’s called Parent Heart Watch, very strong advocacy going to their legislatures, trying to establish laws such as Louis’ Law. Just recently, Melinda Murray, just recently in 2021 established Dominic’s Law. She lost her son on the basketball court and Dominic’s Law, in New York state, was signed in by Governor Kathy Hochul, last October. That mandates that the pre-procedure, 12-point questionnaire, from the American Heart Association, is mandatory to be completed prior to the high school student performing athletics. We are making some strides thanks to our parents.
Dr. Eileen Handberg (13:13):
Wow, that’s fascinating. We’ve been talking to Carol Patrick about hypertrophic cardiomyopathy. We’ll be back after a quick break.
Dr. Eileen Handberg (13:22):
We’re back to discuss more about hypertrophic cardiomyopathy with Heidi Salisbury. Can we pick up on the issue of, Carol elegantly covered screening and identification of these young athletes who have HCM or other channelopathies. Can you talk to us about, how do you find out where centers of excellence are? What is a center of excellence? What would be the expectation of going there? Do you have to stay hooked to that center for the rest of your life? Could you tell us a little bit about that journey?
Heidi Salisbury (13:57):
Yeah. Thank you, Eileen. Thank you, Carol, for all of the work that you’ve done, the leadership, the wisdom. Just to piggyback onto what Carol said first, and shared first, is that, there’s not a cure for HCM at this time, and clearly, it affects many individuals, and sometimes without them knowing, and sometimes we don’t discover this until after a loss. In general, what we think about with HCM, key is early detection and screening. Carol just outlined this so well, so I’m going to come in here now and talk about what happens as a provider, as a nurse in the field, if you’re able to refer to a Center of Excellence. But key, really in treating HCM, because it is a treatable condition, is early detection in the community.
I can just really echo what Carol shared, how important it is for our primary care teams, in particular, and our primary cardiology teams, to consider using the 12-point questionnaire from the American Heart Association, and if that’s not an option, to just strongly pay attention to your history and physical and family history. Then once the individual, or family, is referred to a Center of Excellence, how do you do this? Where do you start? Center of Excellence’s were described earlier by Eileen, but in general, a Center of Excellence for HCM, consists of an interdisciplinary team that can take care of an individual, and a family, across the generations, touching base with experts across all different areas in cardiology and family care that a patient might come across in a lifespan. That ranges from experts in imaging and cardiac testing, to nursing, to family planning and obstetrics, and so on, and I’ll walk through some details there.
If I were out in the community and I have this referral, where would I start? I would actually start with going to one of our advocacy groups, again, very powerful in this community. The Hypertrophic Cardiomyopathy Association website lists the national Centers of Excellence. That is one place that you can reliably find a list, an up to date list, of the centers of excellence across the United States. There are some international Centers of Excellence listed as well. You’d then go to the website and follow the referral process. On the receiving end of that referral, on my end, what’s really, really helpful to have is the reason for the referral, any cardiology testing that’s been done, specific family history, that’s informing this referral, all of that’s key.
Once the referrals received on our end, what we do is we have our nursing team trained to contact the family, and to check in on the family history, on symptom history, on cardiac records, and then order some additional testing, if appropriate, so that we are ready to go when we see the patient in person. When the patient comes in person to our center, they typically, have had echocardiogram at rest and very likely also with exercise, they may also have had a cardiac MRI. I believe these tests have been reviewed in a previous podcast, but Eileen is that… Did you?
Dr. Eileen Handberg (17:56):
Yeah, they have.
Heidi Salisbury (17:58):
Great. 24-hour or at minimum 48 hour, but usually up to 14 day ambulatory telemetry, called Zio Patch, used to be called Holter Monitor, looking for their arrhythmia burden as well as lab work. The patient then on day of visit will start with the nursing team, building relationships, getting an overview of the center, taking vitals, reviewing medications. They will then meet our physician, and our genetic counseling team. The physician will go through all of the history and all of the clinical data that we have, and either confirm, dismiss, direct the diagnosis. From that point on, a decision will be made if genetic counseling and testing is appropriate, and typically in these patients, it is.
I think we’re going to talk a little bit more about that later, but genetic counseling is always part of a Center of Excellence visit, at least offered to the patient, and then testing, if appropriate, can be authorized and sent out at the first visit or a future visit. Following this first visit, typically our patients follow up with our advanced practice providers, based on next steps for them, which could include considering a defibrillator, could include medication adjustment, titration tolerance, could include review of genetic testing results, and could include additional tests if that was required. Overall, once you’ve made that referral to us, our priority is always first, to make a good thorough diagnosis and to provide a first or second opinion on what are we working with.
Then if this is true, true hypertrophic cardiomyopathy or not, is this patient safe? Do we need to think about anything in terms of primary prevention for sudden cardiac death, such as a placement of defibrillator. Then further, can we further define this disease by looking into their DNA and consider genetic testing? Next step is, okay we know what the diagnosis is, the patient is safe, we have sent out genetic testing, let’s continue to support their quality of life into the future, with either medical support and or education, set up routine cardiac surveillance for them, and finally, family screening, what does that look like for this family? In the end, we wrap it all up with a patient letter provided to the family, that indicates diagnostic information and who in the family should be screened.
Dr. Eileen Handberg (20:58):
Can we take up that point about screening? We’ll get into the device and sudden death as the next part.
Heidi Salisbury (21:10):
Throughout the first visit, and evolving visits for a patient and family, we construct a document, it’s a pedigree. A pedigree of the family’s history, and this evolves as we get to know the patient, it also evolves as we might receive genetic testing results, and the pedigree evolves as the generations continue to grow and people have children. The first thing we do is, we offer genetic testing in the individual in the family who has the most obvious disease, because their highest chance to yield a result that we can use. In some cases, the individual with the most obvious disease might be deceased, and perhaps we received these results on autopsy.
In that instance, there are times where we try to do postmortem genetic testing on the tissue sample that was saved during the autopsy, or if we do find another living family member that has obvious disease, we start with the genetic testing on that individual family member. If we find a genetic marker, genetic mutation, that we are confident defines the disease for this family, and that happens in anywhere from 50 to 60% of the cases of hypertrophic cardiomyopathy, that we find a genetic result that we can use to screen family members. We take this genetic result and we can use it then for what’s called predictive genetic testing screening and in a family. What that means is I’m confident that the genetic variant that was identified for this family is correlated to causing disease and therefore I can take this information and look for just that genetic variant in each family member, starting with the first-degree relatives or any second-degree relatives who might have symptoms that are suspicious. We now have this key that we can look for in the family.
We don’t just go testing everybody, we offer genetic counseling, previously this is a shared decision-making conversation, not everyone in a family will go through with genetic testing. In the case that we have the ability to do predictive genetic testing, you look for the variant, just that specific variant, versus a whole panel of variants, starting with first-degree relatives. You counsel them first, and then should they proceed, you wait for the results, and then disclose the results to them. All of our individuals who go through predictive genetic testing still have a baseline echo EKG, which is the recommendation for screening for all first-degree relatives of HCM. Again, independent of what genetic information you have. Just to restate that a little more clearly. We recommend a basic echo and EKG for all first-degree relatives of individuals who have HCM.
Dr. Eileen Handberg (24:19):
What do parents do if they’re raising children that do carry the mutation? How does that walk through? If they’re young enough, they haven’t manifested really any symptoms of disease, but you know that they have the mutation, that doesn’t necessarily mean that they’re going to manifest the disease. Is that correct?
Heidi Salisbury (24:41):
Correct. That’s correct. It’s more likely that they’ll manifest it than not. It does mean that we put into conversation early, a cardiac surveillance plan. By guideline, you really start echo EKG without any symptoms, you start echo EKG moving into puberty, between age 10 and 12. As we all know, that’s a little bit of a moving target for children. The other piece here is, you know this individual carries the variant, you know that they’re at risk, you just don’t know when and if the cardiomyopathy will present itself. Again, really go back to shared decision-making and offering support to the families, this is a difficult piece of the work that we do, and difficult piece of the parenting. There’s advocates, there’s a lot of support through the Children’s Cardiomyopathy Foundation for parents who are shouldering this, and then we offer support through our counseling teams, and just through our own experience.
As the parent see us in clinic, we keep the care of their children and the parenting around decision-making for a child that is positive for the genetic variant, as part of the conversation, so they feel supported on our end too. One thing that is important to talk about, is that although the guidelines indicate that you begin the cardiac screening when they’re entering puberty, we know that a child that does have physical expression of HCM on their cardiac testing, is going to be likely restricted from physical activity. Especially in the state I live in, kids are very active all year round at a young age, and many of our parents will decide to do the first thorough screening, including echo, EKG, before children start kindergarten, because by the time they’re in kinder here in California, they might already be playing two or three sports. That is something that is often part of our conversations. The second piece on the parenting side is, the younger you can normalize cardiac screening for a kid that’s going to likely need this cardiac screening for a lifetime, a lot of parents find it helpful to start that sooner than later.
Dr. Eileen Handberg (27:05):
Okay. Carol, can we talk a little bit about HCM? We know that the risk, the first manifestation in many of people, especially young athletes, is that sudden cardiac death episode. It’s horrifying to see this on ESPN and all the places that this gets broadcast. Clearly, defibrillators are the lifesaving therapy that exists. Can you talk a little bit about device placement and those conversations in people with HCM?
Carol Patrick (27:48):
I would love to, thank you Eileen. Heidi, on the heels of your eloquent discussion of genetic testing, family conversations, and shared decision-making. I look to that as the guide for how we move forward in discussing and really making an algorithm approach to the device selection. First of all, is it needed, primary versus secondary prevention. To define that secondary prevention is a no-brainer in terms of that particular person had a cardiac arrest, had sustained ventricular tachycardia event, so they will get a device, an implantable cardiac defibrillator. There’s not just one type of device. The primary prevention is where we get back into the parents, the patient, as well as the shared decision making with how many risk factors, major risk factors, for sudden cardiac death are there? What is the psychosocial adjustment and appropriateness of the patient? As well as the family. I have patients that have children 12, 13, the mother cannot live each day worrying and wants the defibrillator. They know the child has the mutation, they know there might be manifestation, they might have passed out once, they want the defibrillator.
Those are the types of conversations that ensue. Typically, the decision for ICD implantation surrounds the patient, the parents, the physician, and all the diagnostic testing that Heidi’s center has performed, in looking at, were there major risk factors, more than one, for sudden cardiac death. Such as sustained ventricular tachycardia, the echo being quite abnormal, the ejection fraction being affected, more than one episode of syncope. There’s different pieces of the puzzle that come into that decision. The other piece, the risk-benefit ratio, that has to be weighed, whenever a device selection is made, is devices are not without complications.
You can get inappropriate shocks, 22% of these patients have atrial fibrillation, which means the upper chamber has that undulating, not contracting, ability and can run rapid and the patient can get what’s called inappropriate shocks. Shocks that did not result from the ventricular arrhythmia, they were from the upper chamber. That can be quite horrifying and terrifying for a child, a pubescent, or even an adult. All ages have those types of fears and psychosocial attempts at really adjusting to living with an ICD, so those things have to come into play. The other piece of it is, especially in the child, as they’re growing, the number of generator changes that will be needed, the types of devices, typically there are subcutaneous, lead-less, defibrillators that could go to the lateral side of the chest without leads, and those are very positive in terms of not having any infection, lead fractures, things like that. They can also cause erosion, you can have device erosion, and those too also need to be changed.
The other piece is if there is any sort of bradycardia, slow beats, or need from a sinoatrial standpoint and they need two leads, then two leads would be placed. Most recommendations for HCM would be to have a single, what’s called a shock box. Meaning it’s a backup, it’s a life insurance policy to be implanted in the patient, to shock them, with a single shocking coil lead, should the need for a sustained ventricular tachycardia, ventricular fibrillation event, occurs. Most patients generally do very well with that type of a defibrillator because they feel, psycho-socially comfortable, knowing that they have this, should that particular event occur. It really is shared decision-making, there’s several pieces to the puzzle that have to be put together to make a decision. There are other patients that absolutely do not want a defibrillator, they have work requirements for their employment, that they cannot have a device implanted, even though they have some major risk factors and they refuse that, and that’s their option.
I’ve had patients that work on high tension wires, up in the telephone poles, and they said they cannot accept that kind of a device on their insurance plan and so forth, because it would identify them as having this, and they do not want the device. Multiple pieces and discussions surrounding, especially if it is a child, in terms of device selection, first to either have it or not. The American College of Cardiology has some very, very robust and clear criteria in terms of guiding our providers on whether or not the person should have a device implanted. Again, the primary prevention has several pieces and if they have more than one risk factor for sudden cardiac death, they do recommend a device implant.
When we say major risk factors, that’s your syncope, more than one episode of fainting or passing out, the LVH, left ventricular hypertrophy, they have that echo showing that set the wall. It’s a no-brainer that they’re going to possibly have an event. The other pieces to the puzzle is if they are having, as you said, the Zio Patch and Holters and so forth, they’re having sustained VT. If they’re having arrhythmia and they’re arrhythmogenic to begin with, it’s very reasonable. It’s a two-way recommendation from the American College of Cardiology to implant a defibrillator. The one A’s are obviously, secondary prevention and the primary prevention of those that have really shown those greater than one risk factors for sudden cardiac death.
Dr. Eileen Handberg (34:31):
Let me ask you a question, both of you, whoever wants to answer. What’s the percentage, obviously, if you have a young athlete who has a primary event, as you said, sort of a no-brainer, although I guess with an athlete, they are thinking about the ability to continue to be an athlete. We’ve seen some of those things play out, especially for college-age athletes and wanting to go into the pros and those kinds of things. What’s the incidents of, say a young child, less than 16 years old, not having a primary event, but having a genetic mutation and ending up having a defibrillator placed in their youth?
Heidi Salisbury (35:29):
What we think about is, this individual either has a family history, a clinical diagnosis by echocardiogram EKG, or a genetic diagnosis, carries a pathogenic genetic variants. Does this individual, this young individual, this athletic young individual, need a defibrillator for primary or secondary prevention of sudden cardiac death. For an individual like this, we have a cardiac surveillance plan in place. How are we going to answer that question? What data do we need to collect and how frequently do we need to collect that data? Typically, it’s annually for an individual who has either the clinical diagnosis or carries the genetic variant. We’re going to do annual cardiac testing. If it’s an athlete, we’re very likely including in that annual cardiac testing, a Zio Patch or ambulatory telemetry monitor, to look for those silent arrhythmias, because an athlete is not going to have a sudden cardiac arrest because they have obstructive hypertrophic cardiomyopathy, they’re going to have a sudden cardiac arrest because of ventricular tachycardia, which is clearly associated with hypertrophic cardiomyopathy.
You really want to think, as a provider, when you’re dealing with a young athlete, and you’re thinking about cardiac surveillance, always wanting to keep an eye on their potential risk for a sudden cardiac event. What test do you need to order to inform that decision-making? An echo is going to tell you how thick the walls of their heart are, it’s going to tell you about any left ventricular outflow track obstruction. An EKG is going to tell you obviously the fingerprint of their electrical rhythm at baseline. How do you assess what their rhythm’s doing the rest of the time out in the real world, especially while they’re active, so we have these tools that we use. Then, once we have that data back, if an individual, as we just described, this young athletic individual, comes back with an arrhythmia or a syncope episode, especially a syncope episode while exercising, or the family history, as you refresh it every annual visit, comes back with a cousin that just died suddenly, their risk is now increased according to the different ways to approach evaluating risks that Carol so beautifully reviewed. Now we have a shared decision-making conversation about considering a protective internal cardiac defibrillator, and what would be the best for this individual, should they choose to proceed?
Dr. Eileen Handberg (38:15):
We’ve covered a lot of content here and this has been absolutely fabulous and eye-opening in terms of the whole process about identifying, assessing risk as Carol covered. What happens when you go to the Center of Excellence? How does that relationship with the center over time evolve?
Heidi Salisbury (38:43):
Hypertrophic cardiomyopathy is a treatable disease and the best way to manage this disease is early detection, in all the ways that we outlined. At our center, once we get through diagnosis, and risk stratification and managing individuals’ risk, family screening, genetic testing, we really move towards annual visits or the patient and family might return to their local cardiologist. Typically, and I’ll be curious, what Carol’s experience is on the east coast. Typically, patients continue their care with our center at a minimum of an annual visit because they’re living with a chronic heart condition, they’re living well, but they’re living with a chronic heart condition that does require nuances in terms of the care of their disease until we have a cure. They appreciate that the Centers of Excellence do see the most amount of individuals with hearts like theirs, and so that annual visit does tend to really go a long way for them in terms of supporting their quality of life. We do that in partnership with really encouraging them to keep routine care with their local team, really stress that, and the majority of our patients have that combination.
Dr. Eileen Handberg (40:12):
Carol, what do we do on the east coast?
Carol Patrick (40:16):
We are so fortunate to have centers of excellence, as Heidi delineates. I feel completely comfortable once a patient is detected, diagnosed, and algorithmed into the cardiac surveillance plan, then I know they’re taken care of, regularly, for the rest of their lives. The focus that I seem to always migrate back to, are the unrecognized, the undetected, and the unknowns, of those people in our population out there, that are on the athletic field that might be exercising, didn’t know or recognize that they had fatigue, shortness of breath, any sort of problem, echocardiographically or EKG, especially in our children, because we don’t do EKGs regularly in the United States for children, and they collapse.
Again, the first symptom is ventricular tachycardia that could be irreversible, unless the AED reverses it. Again, once recognized, once detected, once going into the excellence centers, we are solidly with a cardiac surveillance plan going forward for the rest of that patient and family’s life. Prior to that is where we need to really focus our efforts on awareness, clinical education, educating our primary providers to understand the 12-point American Heart Association questionnaire, understand the components of the physical exam, and how important it is to move further when there’s a family history, such as anybody dying under the age of 50, an unknown death, as well as, syncope and all the different symptoms we’ve gone over, and putting that all together to refer, to get them to the Centers of Excellence, and that’s what’s key.
Dr. Eileen Handberg (42:14):
I can’t thank you both enough for this very informative podcast that we’ve had, where we’ve talked about hypertrophic cardiomyopathy, really centering on screening and detection and how to get referred to a Center of Excellence. Thank you both so much for joining me. On behalf of PCNA we’d like to thank Bristol Myers Squibb for their support of this non-CE podcast. PCNA is proud to offer educational opportunities like these to further our commitment to educate our members in an objective way, regardless of funding support.
Thanks to everyone for attending and please join us for the third podcast in this series and look forward to seeing you on the next round.
PCNA (42:44):
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Cardiomyopathy
Published on
June 21, 2022
Listen on:

RNFA, MS, CCRN, NEA-BC, ACNP-BC

RN, MSN, CNS-BC, ACGN
Related Resources

Videos
A Nurse to Nurse Conversation on Hypertrophic Cardiomyopathy and Shared Decision-Making Video
January 19, 2025