Dive into the genetics of the rare Homozygous Familial Hypercholesterolemia or HoFH. Guest Ruth Schneider emphasizes the role family or cascade screening can play in this rare genetic condition.
Episode Resources
Supported by Regeneron Pharmaceuticals
Geralyn (00:20)
Welcome to today’s episode, the second of three episodes on familial hypercholesterolemia, also known as FH. Our previous episode explored the signs and symptoms of FH and the differentiation and diagnosis of homozygous FH and heterozygous FH. Today we’re going to winnow down a little bit more and focus on homozygous FH, also known as HoFH, and we’re going to talk a little bit about the genetic implications of that.
I’m joined today by a PCNA chapter leader who happens to work with patients with FH. Ruth Schneider, could you please introduce yourself to our audience?
Ruth Schneider (00:56)
Thanks, Geralyn. I appreciate being here today. So as Geralyn said, my name is Ruth Schneider. I’m a Nurse Practitioner at UT Southwestern, and I work with the Preventive Cardiology Team. In 2018, we actually opened up an FH clinic. So, we see patients with both heterozygous FH and homozygous FH.
The clinic was basically initiated because of a quality improvement program that an endocrinologist and cardiologist felt strongly about in that they wanted to get the word out about FH, educating both providers and patients about this disease.
So, when we first initially started, the cardiologist and the endocrinologist went out to groups at UT Southwestern. They included OB-GYNs, internal medicine doctors, APP groups, and basically told them a little bit about FH and what to look for when they’re looking for individuals with FH.
We also worked with the IT group and essentially, they were able to pull a registry of all individuals at UT Southwestern that had ever had an LDL above 190. Now, that turned out to be a huge group of individuals. From that, we basically ruled out those that were extremely high, 13,000 LDLs, around that, and we focus primarily right now on LDLs between the 400 to 200 range.
Within that, it is kind of an ardous process in that we have to go through, and we’ve had medical students involved, residents involved, where we go through chart by chart, ruling out secondary causes that may cause the LDL to be high. And those that don’t look like they have a secondary cause, then our research coordinator contacts the patient via MyChart message as well as a letter is sent. One week later, that is followed by a phone call by me to ask them if they have any questions, if they are interested in coming into the clinic. And so that’s how our FH clinic really started out.
Geralyn (03:22)
That sounds like an incredibly comprehensive process to try and identify some of these individuals that have FH that might otherwise be missed. So, I’m really excited to have you share about that particular process. I think we all could learn something from that. But we also would like to learn just a little bit more about HoFH. And I’m hoping you could talk just a little bit more about the specifics of that homozygous FH.
Ruth Schneider (03:47)
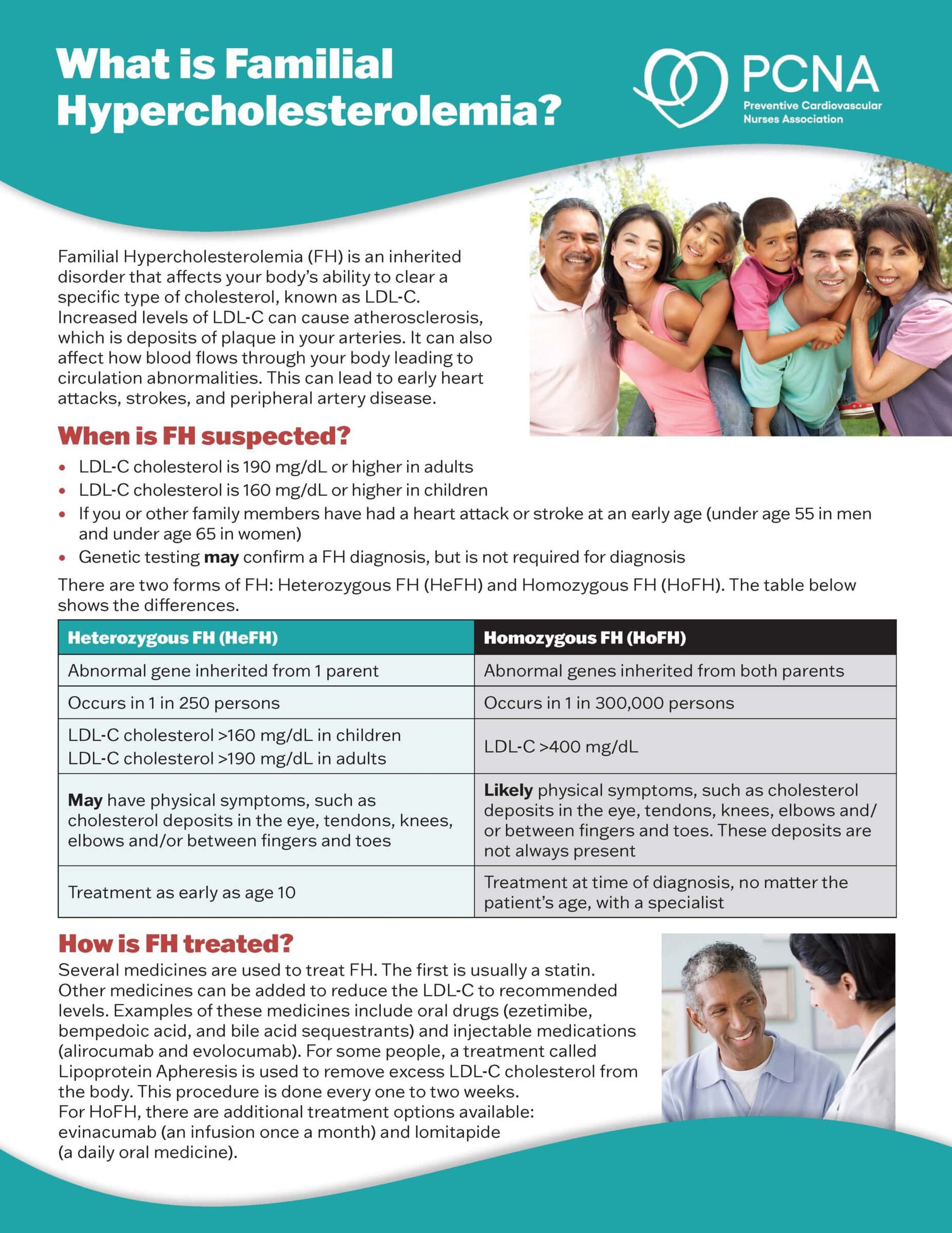
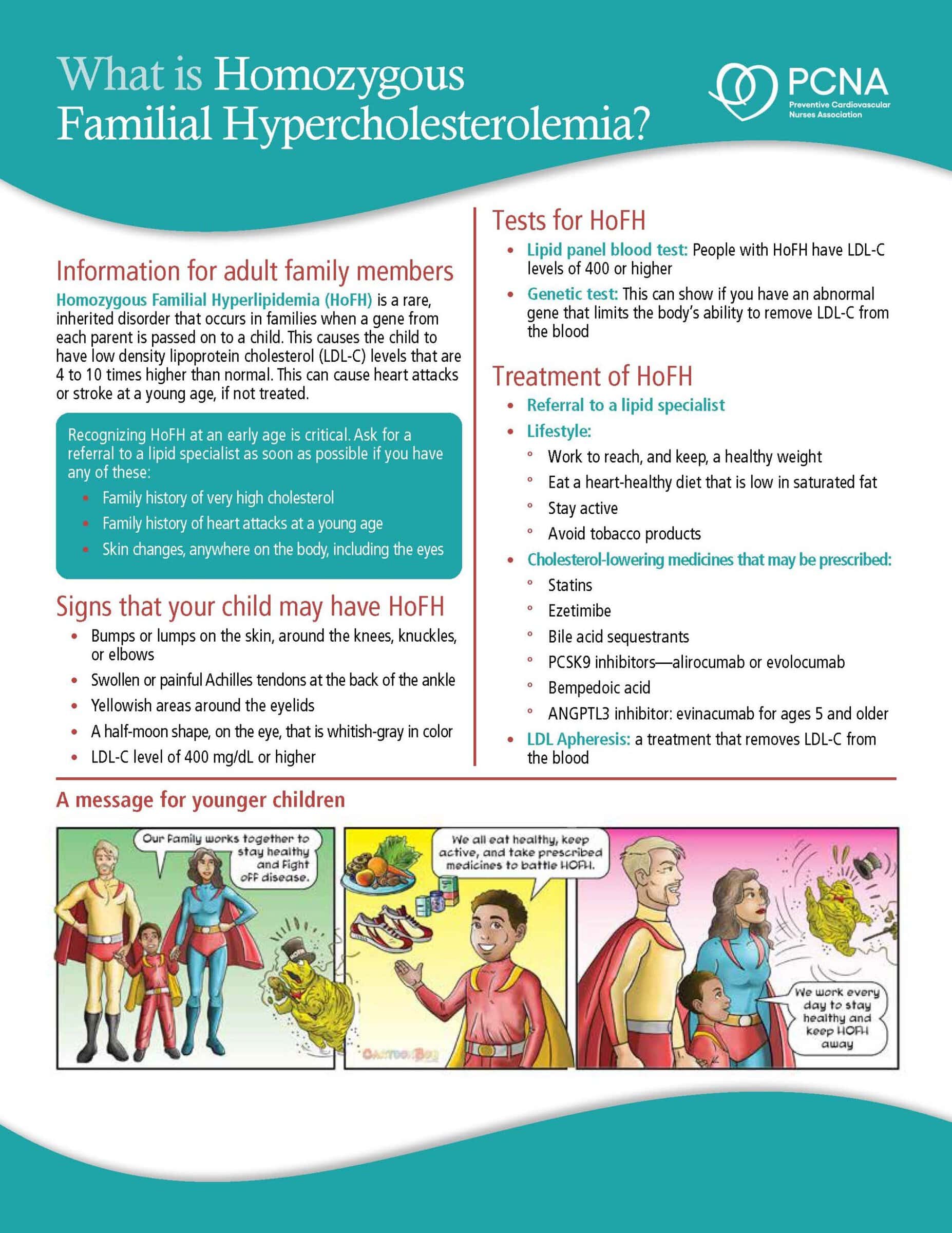
Yeah, so homozygous FH is different from heterozygous FH in that homozygous FH means that each parent gave this mutation to their child. So, the child has two mutations, one from each parent. That means that when we look at these individuals, their baseline LDLs prior to treatment are going to run anywhere from 400 to 1,000.
They’re going to be extremely high. This is much more rare than heterozygous FH, typically one in three hundred thousand.
The problem with homozygous FH, it’s much more difficult to diagnose because these LDL levels they’re born with, just like heterozygous FH, but they’re so much higher, and they tend to get cardiovascular disease before the age of 10.
Geralyn (04:46)
So, in addition to those really high LDL levels, what other diagnostics are you looking for in that process to delineate whether or not it is actually HoFH?
Ruth Schneider (04:57)
Yes, so essentially you can do genetic screening, that definitely is done. Also, when you’re seeing an individual, and this is probably a lot of times pediatricians at that point, there are familiar marks or in the physical exam that you may see.
So, xanthomas, those are cholesterol plaques that occur. A lot of times we think of them being between the fingers or in the down tendons behind your ankle. But we have seen them on the back. We’ve seen them all over an individual, depending on how high their LDL is. A lot of times the first person who may see that is they’re sent to a dermatologist to have those plaques removed, thinking they are something else.
Again, you can also see that corneal arcus, that’s that yellow or gray circle around the cornea. And you can see what we call xanthelasmas, and they are basically plaques around the eyelid or right below the eye.
The other thing is just getting a very good family history, looking for premature cardiovascular disease, looking at their parents or other family members that had extremely high lipid levels.
Geralyn (06:21)
So, you were talking a little bit about seeing pediatric patients. At what ages could we test for this?
Ruth Schneider (06:27)
Yeah, great question. You can test as early as two. The guidelines now say it is recommended that they check at 10 years of age, a screening. But definitely if you have someone who has some history, you see these physical exam features, then I would go ahead and check it too. Because by age 10, as we talked about, they already have developed cardiovascular disease.
Geralyn (06:54)
We’ve been talking with Ruth Schneider about HoFH and are going to take a quick break.
We’re back to continue our discussion about homozygous familial hypercholesterolemia, also known as HoFH. And Ruth, you’ve already discussed just a little bit about the genetic transmission of this that we need both parents to have shared that mutation with their offspring. Can you talk a little bit more about what cascade screening might look like in these families?
Ruth Schneider (07:20)
Absolutely. So, the first person who probably is identified is that individual with homozygous FH or it can be heterozygous FH. So, if they do genetic testing, then you determine that abnormal gene that they have. From that, you can go out to all family members. You can go out to aunts and uncles, grandparents, children, and basically screen for that gene.
You don’t have to do the full genetic testing, you can screen for that gene, getting to many more individuals than you would be if you hadn’t done the screening.
Geralyn (07:59)
So, it sounds like that genetic testing is really, for some, kind of their entree into knowing that they even have that, that maybe somebody else in the family has it, but it’s a great way for us to identify those family members that might also be at risk and not even know it. Perhaps they don’t have the xanthomas or corneal arcus or those types of things, correct?
Ruth Schneider (08:05)
Exactly.
Geralyn (08:19)
So, if individuals are looking for education for their patients with FH, what kinds of resources would you point them towards?
Ruth Schneider (08:28)
Honestly, we point our patients to the FH Foundation. When they come in as new patients, we give them a packet. It’s got their website on it. We give them several pieces of information from them. Also, the PCNA website is an excellent resource. There is information for patients as well as providers on FH, and both are an excellent resource.
Geralyn (08:58)
I have one final question for you and that is, Ruth, what do you think is the top takeaway you would like our listeners to keep in mind as they leave listening or watching this particular episode?
Ruth Schneider (09:09)
I think if you’re a clinician, the top takeaway points are if you’re looking, thinking about FH on a patient is the LDL level is extremely important. And remember that’s untreated LDL at those levels. And also, the physical exam can give you a lot of information as well as a detailed family history looking at premature cardiovascular disease.
Geralyn (09:41)
Well, it definitely takes a team for us to be able to prevent cardiovascular disease in our patients. And particularly for those that are at risk with FH, there are some additional steps that we can certainly take.
And we are very grateful to Ruth Schneider for taking time with us today to share some insights and some clinical takeaways that we can address right away in practice. This particular episode, as I mentioned earlier, is part of a three-part series on familial hypercholesterolemia. And we encourage our listeners to listen to the other two episodes for more information. You can also search for links in our show notes and listen to parts one and three there.
We also would like to thank Regeneron Pharmaceuticals for their unrestricted grant funding for this podcast miniseries. This is your host, Geralyn Warfield, and we will see you next time.
Topics
- Lipid Management
Published on
February 18, 2025
Listen on:

RN, MS, ANPC
Related Resources
Patient Education Handouts
What is Homozygous Familial Hypercholesterolemia? Fact Sheet
August 06, 2025