Improving quality of life for patients with heart failure can include lifestyle modifications and require successful behavior change strategies. Learn best practices to apply to your clinical setting from nurse providers Colleen McIlvennan, PhD, DNP, ANP, FAHA, FHFSA, of the University of Colorado in Denver, and Binu Koirala, PhD, MGS, RN, of the Johns Hopkins University School of Nursing in Baltimore.
Earn 0.5 contact hours and .05 pharmacology hours from listening to the podcast episode and completing the course components.
This podcast is supported by independent educational grants from Merck Sharpe and Dohme Co, and the Pfizer-Merck Alliance.
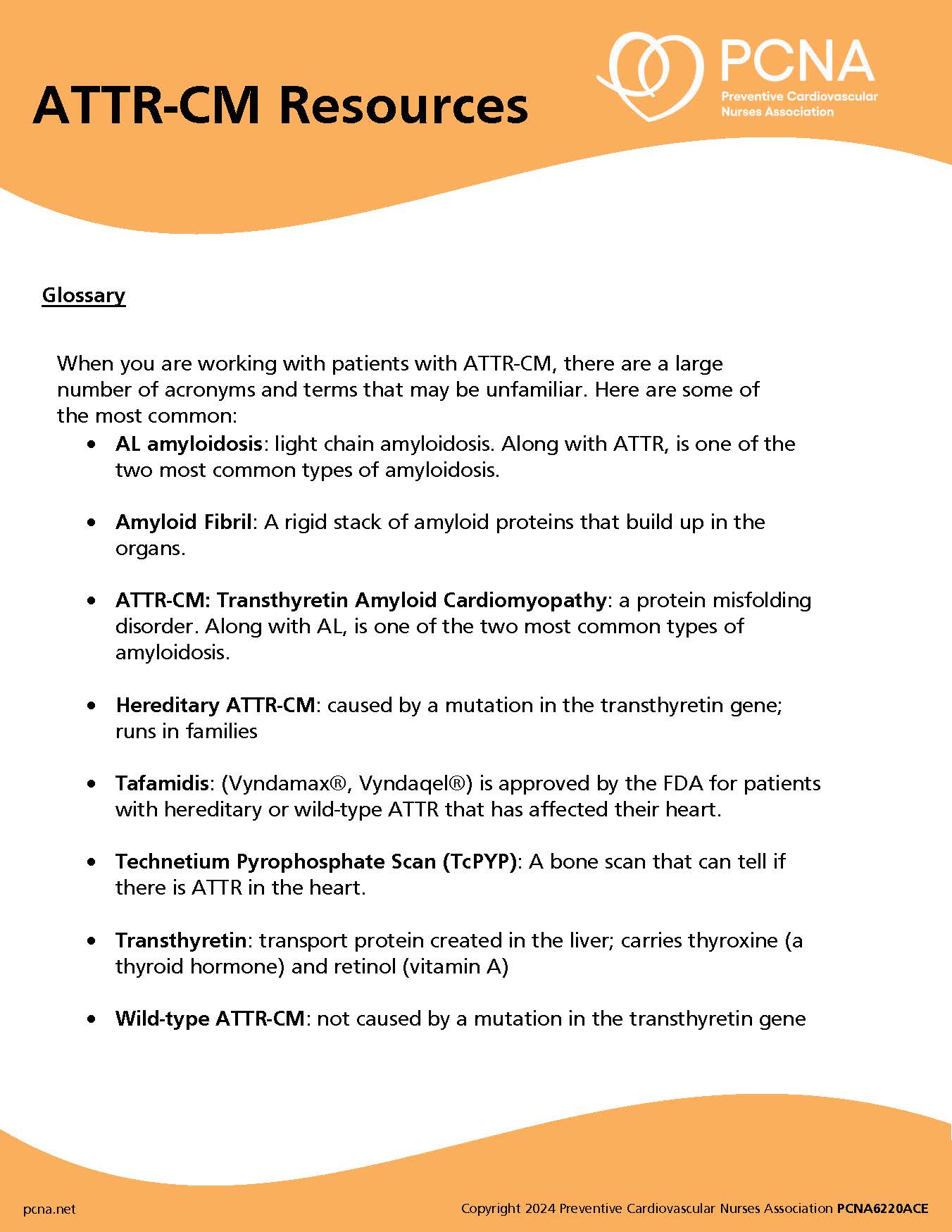
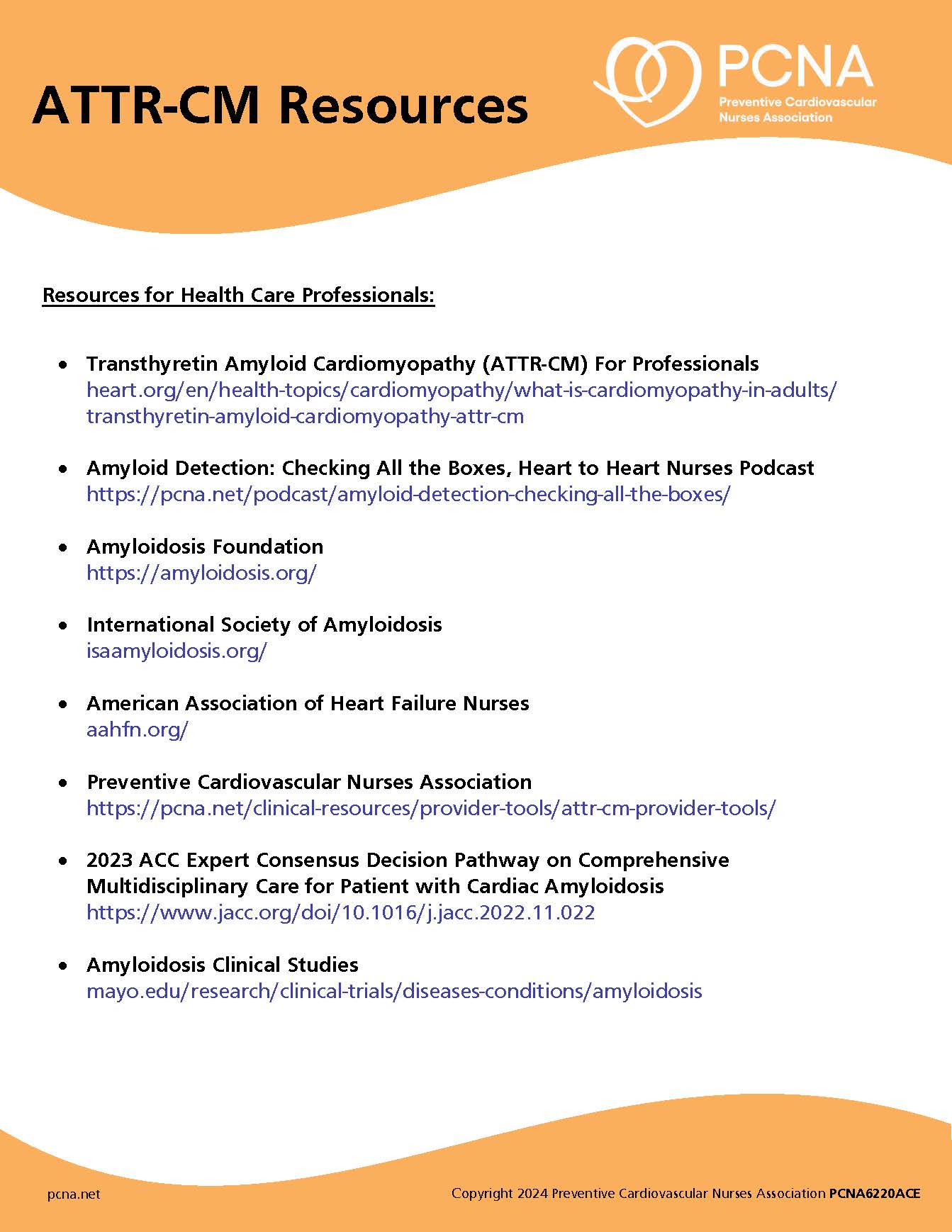
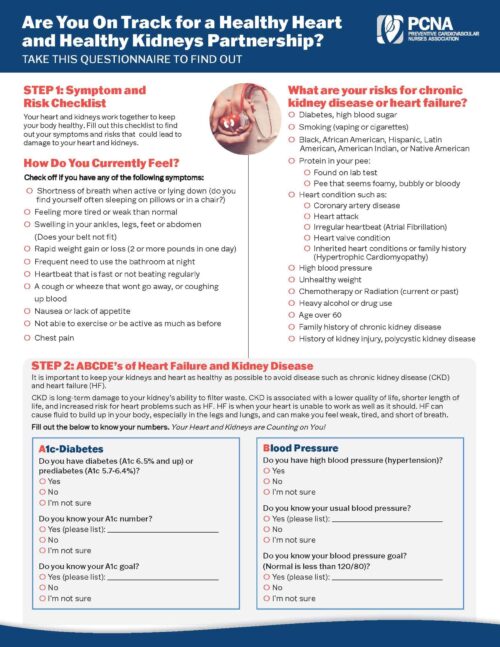
Episode Resources
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to today’s episode, which focuses on lifestyle and self-care in patients with heart failure. I’m your host, Geralyn Warfield.
This episode is available for CE contact hours. Please follow the link in the episode show notes to complete the post-test and access your CE certificate.
Today I’m joined by Colleen McIlvennan and be Binu Koirala. Colleen, could you introduce yourself? And then we’ll have Binu do the same.
Colleen McIlvennan (guest): Yeah, thanks so much, Geralyn, for having us today. I am Colleen McIlvennan. I’m a Nurse Practitioner and researcher at the University of Colorado. And I also serve as the section head of advanced practice providers in the Division of Cardiology. [00:01:00] My primary work is on the inpatient advanced heart failure and transplantation service. And my research focus includes patient engagement around treatment options for heart failure.
Binu Koirala (guest): And hi, and this is Binu Koirala. I’m an Assistant Professor at the Johns Hopkins University School of Nursing. My clinical background is I’m a cardiovascular nurse, primarily working with people living with heart failure. And currently as a research faculty, my research focus includes cardiovascular disease prevention and management, palliative care, and care of people living with multiple chronic and complex disease conditions, including heart failure. Happy to be here today.
Geralyn Warfield (host): Thank you so much to you both for being with us today and let’s get started talking a little bit about heart failure as a chronic disease. We know that using guideline-directed medical therapy includes things like lifestyle, [00:02:00] pharmacotherapies, and other treatments. So, if you wouldn’t mind, let’s talk first about lifestyle modification and, specifically, behavior change. Colleen, would you like to start?
Colleen McIlvennan (guest): Thanks, Geralyn. I think that’s a great place to start when we’re talking about management of patients with heart failure. And when we talk about behavior change, like chronic disease, it’s ongoing. It’s something that we touch upon with every clinic visit, every hospital stay, in which we are educating patients about different areas that would help improve their quality and quantity of life.
I think we all know the stages of change, and with patients with heart failure, I would say it’s, it’s really no different. They really have to have that readiness for change. I had a conversation today, actually, with a patient who was 37 and had heart failure. And was still smoking. And she knew she should stop smoking, but she just hadn’t been ready. And I offered her to talk [00:03:00] with one of our smoking cessation specialists, but she said, “No, I really needed to be ready, and I think I’m ready now.” But it’s really having those different touch points with patients, to really catch them at the time where they’re ready to make that change, and then trying to give them the tools to do that.
I also think, in my research we’ve done a lot around shared decision-making. And we talk about shared decision-making in the context of medical devices, and medications, but I would argue that having lifestyle changes or behavior changes and a shared decision-making approach in that respect is really important, because we really need to understand what’s important to patients around their values, preferences, and goals in order to recommend, and coach them, really, through these lifestyle and behavior changes.
And last point, I think, when we talk about behavior change is that often in the initial diagnosis of heart failure, [00:04:00] patients are overwhelmed and we’re focused very much on treatment options, diagnostics, and, and really kind of the care plan going forward. That, a lot of times, the lifestyle and behavior changes fall to the bottom.
And I think as we continue to see these patients and follow up is really when we can get down to what it is that we can do to help them change lifestyle, change behaviors, that will lead to, an improved quantity and quality of life.
Binu Koirala (guest): Just to add on what Colleen said, effective management of heart failure, and its science and symptoms, require equal participation by the individuals with heart failure, their family members, as well as the whole healthcare team members. And behavior changes or lifestyle modification in heart failure, which can help prevent or manage signs and symptoms as well as disease progression, is just as important [00:05:00] as medications prescribed to heart, like to treat heart failure. And our research among people with heart failure, as well as other studies, have shown that lifestyle modifications to promote self-care activities in heart failure have improved patients’ quality of life and health outcomes such as rehospitalizations.
And when we talk about lifestyle modifications, which can include like, changing diet by eating a heart healthy diet low in salt, getting more physical activity, maintaining or losing weight, quitting smoking, limiting alcohol intake, managing stress and anxiety, and more. And, for example, our research studies suggest that dietary interventions aimed at increasing patient’s appetite may increase diet variety and enhance the nutritional quality of diets [00:06:00] for people with heart failure.
And as a healthcare provider, it is really important for us to improve health outcomes of our patients by identifying their modifiable risk factors and providing follow-up behavior change, goal-setting education, and interventions.
Geralyn Warfield (host): Those were exceptional examples of how behavior change and heart failure management for our patients really are closely intertwined. And I appreciate, Colleen, you sharing that real-life example of behavior change is not linear, nor are our patients ready for that behavior change process at the times we would wish that they would be. So, using our shared decision-making with those patients can be a really important tool in that trajectory of care, where we’re working to improve those patient outcomes alongside those patients and, as you said, Binu, with their families, with their caregivers. It definitely is indeed a team [00:07:00] effort.
So, I’d like to pivot just a little bit and focus in just on access to care. I’m hoping we could talk a little bit about how access to care specifically impacts these patients with heart failure. Colleen, could you start us off?
Colleen McIlvennan (guest): Yeah, I think access is a real issue. And, unfortunately, we are continuing to see disparities in care, and I worry that, instead of closing the gap, it maybe widening with advances in technology, and, and people not having access, to the areas of technology that we need, in order to meet them where they’re at.
And so. I think one of the areas and, I believe, Binu’s going to touch a little bit on this as well, but pharmacy deserts is something that we don’t talk too often about, but are a real issue when it comes to access to [00:08:00] medications. And now that pharmacies are really providing more preventative care and immunizations and education to patients. We really saw it with the COVID-19 pandemic; people were really going to pharmacies for a lot of their information, for their immunizations, for their education around medications. And I, I think with patients not having access to, to readily available pharmacies that, that we are seeing maybe a, a larger gap, in this care, I think.
One of the areas that we, are hopefully making some strides are mail-order pharmacies, and then places like Amazon who are, I think, are dipping their toes into the pharmacy market, and, and legislation being passed around lowering prescription drug prices. I do think we are, we are moving in the right direction [00:09:00] and there are, people that are paying attention to this, but one of the things that I think would be really beneficial is having those conversations with patients about access to medications. And making sure that they not only can afford them, but can they pick them up? Can they pick them up in a timely manner? And does the pharmacy have the medications that we are actually, hoping to prescribe to them?
Binu Koirala (guest): So, when we are talking about access to care, I just want to remind our listeners, if you have not listened to the previous episode of heart failure podcast series, please do listen. We have talked in more detail about access to care and how it affects heart failure patients on prevention and management.
So today, when we are talking about self-care, access can mean a number of things, for heart failure, treatment and self-care. For example, access to knowledge, access to medicine, access to care team, [00:10:00] access to effective health programs, for example, self-care resources including healthy food. And with our work, with people living with heart failure, and as Geralyn said before, what we have learned is self-care in heart failure is not a linear process.
And access to care and heart failure management, specifically self-care, is compounded by the effects of several social determinants of health. And although there has been an increasing focus on social determinants of health to help reduce health inequalities, daily clinical practice and research agendas generally do not focus on assessment of complex relationship of these determinants and their effect on heart failure treatment, behavior change, and outcomes.
So, what we know already is, in heart failure, limited access to resources [00:11:00] about the disease and the lifestyle changes, as well as evidence-based guideline directed care, are associated with more frequent symptom exaggeration, increased symptom, burden, decreased quality of life, and multiple hospitalizations.
Geralyn Warfield (host): We’ve been discussing lifestyle, and behavior change, and access to care as it relates to our patients with heart failure. We will be right back.
Geralyn Warfield (host): We’re back speaking with Colleen McIlvennan and Binu Koirala about heart failure and some of the factors that affect our patients. And I know that there has been an increasing set of research that’s related about quality sleep, and that really does affect our patients with heart failure. Binu. I’m hoping you can start us off talking a little bit more about those interconnections.
Binu Koirala (guest): Geralyn, I have to say thank you for having this question, because sleep is something that has been [00:12:00] less explored and less discussed in heart failure management. And recently, American Heart Association has identified sleep as one of the healthy behaviors in Life’s Essential Eight.
And it is believed that adequate sleep promotes healing. It can also improve brain function, and it can also help reduce the risk for chronic disease, including heart failure. And specifically in heart failure, the relationship between heart failure and the sleep is a two-way street. For example, heart failure can affect your sleep, and sleep problems such as obstructive sleep apnea and insomnia can make heart failure symptoms worse
And specific to self-care, although the direct mechanism is not well understood, it has been found that sleep quality can mediate self-care. So, with the existing evidence [00:13:00] highlighting the potential importance of adequate sleep and quality sleep behavior in the prevention and management of heart failure, we need to explore this more and examine this more in our clinical practice, as well as the research.
Colleen, do you want to add more based on your experience?
Colleen McIlvennan (guest): Yeah, I would, agree. This is a great question. And an area that is not touched upon probably as much as it should be. And we’ve actually seen quite a bit of interest over the last several years, too, in screening, and treating central sleep apnea for patients with heart failure. And we are implanting some devices that help with central sleep apnea and presents with symptoms that don’t correlate as much as people would think, like snoring, as you would see with obstructive sleep apnea.
So, I think we are under-diagnosing across the board. I [00:14:00] think sleep is, difficult, as Binu mentioned, for a lot of reasons, especially for patients with heart failure, but an area that we need to focus, and really need to have conversations with patients about their sleep quality.
Geralyn Warfield (host): Thank you both so much for addressing sleep as one of the considerations in working with our patients with heart failure. There are a multitude of things that affect our patients. And we spoke a little bit earlier about behavior change, how it’s a process that’s not necessarily linear, but I’m hoping you might be able to share some strategies with our listeners for how we can help our patients by successfully coaching them.
Colleen, I’m wondering if you could start us off, maybe with some examples or just some ideas that our clinicians could use in practice.
Colleen McIlvennan (guest): Yeah, I think this is difficult, because it’s going to be different for each patient. But I think some pearls that I have, just from my clinical practices. Number one, [00:15:00] really engaging the family and the support system. So, back to the example I gave earlier about the woman being educated about stopping smoking. Her mom and her husband were in the room. And I, I said, “We really, let’s talk about the smoking; everyone’s here.” And she, you know, immediately pointed to her husband and she said, “He’s trying to stop also” and he had been smoke free for three days. And she said, “I think it will be a lot easier to stop without, my husband not smoking around me.”
And I, so I really do think support systems can help encourage, they can help motivate. And have everyone on board, to promote certain lifestyle changes, that doesn’t need to just be smoking, but if it’s a change in diet, making sure patients are taking their medications, as much as we can engage the people that the patient relies on for their support, I think, [00:16:00] the more successful we will be.
And then second, I, I think I have been most successful in kind of establishing a rapport with a patient and also tackling the low hanging fruit. So, is there one small change that they could make? And, and are they getting positive feedback for that small change in which they want to maybe, start with maybe a little bit larger of a change. And we do see this, now with activity trackers, you get an alert on your phone if you close your, your rings in a day, and that can be motivating.
So there are different ways to nudge patients, into kind of positive reinforcement. And I, I think, starting with kind of the, the easy things first in order to really kind of then get to the larger, the larger issues or the larger change, has been, has been most successful in my practice.
I’d be interested to hear what Binu has [00:17:00] to think about that.
Binu Koirala (guest): And just to add on that, Colleen, when we think about behavior change, I remember a proverb: if you give a man a fish, you feed him for a day, but if you teach a man to fish, you feed him for a lifetime. So, as I also work in palliative care, what I believe more is rather than teaching them or giving them the right answer—we can do that; every healthcare provider can provide right answer—but the more important thing that we can do, including the nurses can do, is help them explore what matters to them, and then determine what changes they are ready for. And then implementing the behavior change. And associating their goals with their long-term vision of health and wellbeing.
And with this, I just want to provide an example that we are now at Hopkins building a program, with [00:18:00] people living with heart failure and multiple chronic conditions. And we are trying to empower them, identifying their person-centered goals, and needs, and then helping them achieve that to help improve quality of life and decrease disease burden and healthcare utilization.
And, we are doing this among people with heart failure and multiple chronic condition. Because if you work with heart failure people, you know, they rarely have only heart failure. So, studies say, like, on average, one heart failure patient have six multiple chronic conditions. And the outcomes and the self-care, or behavior change activities are more challenging and complex among those people.
And I can talk more about this, like for a whole day, but thinking about, behavior change, what I believe is having the person-centered care models and empowering [00:19:00] them, understanding their goals, and helping them through the behavior change is important for the healthcare providers.
And one last tip. I know everyone does this, but it’s still like when we are discussing with our patients and family caregivers about the heart failure or lifestyle modifications, just using simple language or terms that they can understand and they can relate to.
Geralyn Warfield (host): We certainly have covered a lot of ground today, and I’m hoping each of you might have some suggested resources for clinicians who are interested in learning more about this topic? Binu, do you have any ideas to share?
Binu Koirala (guest): I know there are several resources that have been developed and published online, from different professional organization. There are resources from Preventive Cardiovascular Nurses Association. As well as from American Heart Association. So, AHA has an interactive [00:20:00] heart failure workbook on healthier living. So, you can just Google, and we will be also providing these links to these resources.
Colleen McIlvennan (guest): Yeah. And I would just add, you know, as we’ve sort of alluded to in this podcast, that patients with heart failure are really juggling a lot of different medications, lifestyle changes, and different providers. But it’s important, for them to really strive for a healthy lifestyle, as much as we can promote it. So, if our listeners are looking for additional information on behavior change, PCNA does have a mini-certificate program available to help you learn more about the theories of behavior change and how they can be applied into a variety of clinical settings. So, you can look for that on PCNA’s website.
Geralyn Warfield (host): Thank you both so very much for sharing these incredible insights into helping our patients with heart failure, in terms of behavior change, considering social determinants of health, and other issues. We’ve been talking with Binu Koirala [00:21:00] and Colleen McIlvennan, and we so appreciate you sharing your time and expertise with us.
This particular episode is available for CE contact hours. We’d ask our listeners to please follow the link in the episode show notes, to complete the post-test and access your CE certificate.
This podcast is supported by independent educational grants from Merck Sharpe and Dohme Co, and the Pfizer-Merck Alliance.
This is your host, Geralyn Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Heart Failure
- Lifestyle and Behavior Change
Published on
September 21, 2022
Listen on:

PhD, MGS, RN
PhD, DNP, ANP, FAHA, FHFSA
Related Resources