Guests Rimsky Denis, MD, MPH, MBA, and Ms. Sam Hoeffler discuss community-based strategies for improving health outcomes and promoting health equity. Specific initiatives include health fairs, and barbershops, increasing communication in disenfranchised communities, improving outcomes in hypertension, and increasing access to healthy food.
This episode was recorded in partnership with Medical Alley and the Association of Black Cardiologists.
This podcast episode was supported by an independent educational grant from Novartis Pharmaceuticals Corporation and Pfizer Incorporated.
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield: Today’s episode of the Heart to Heart Nurses podcast is the first of a three part mini series focusing on health equity.
We are pleased to be partnering with Medical Alley to bring you this special guest episode. If you’d like to hear more from Medical Alley, you can follow the Medical Alley podcast or visit their website at medicalalleypodcast.org. Enjoy!
Frank Jaskulke (host): Welcome
Rimsky Denis (guest): Hi and thanks,
Sam Hoeffler (guest): Thanks,
Frank Jaskulke Good morning, good afternoon, and good evening to everyone out there in Medical Alley. Thank you for joining us on another episode [00:01:00] of the Medical Alley Podcast. This is your host, Frank Jaskulke, and we’re doing another episode today as part of our long-standing partnership with the Preventative Cardiovascular Nurses Association and the Association of Black Cardiologists.
Today, we’re going to have a fun and very important conversation on the role of community-based initiatives in improving health outcomes and promoting health equity, and I’m so pleased to be joined by two fantastic guests who are going to give us some perspective and some insight. And I’m so pleased to be joined by two fantastic guests, we’re going to be joined by Dr. Rimsky Denis and by Ms. Sam Hoeffler. And the two of them are going to give us some perspectives on community health and community-based initiatives. And what I might ask is, Dr. Denis, if you’d start, just tell us a little bit about yourself and your practice and your work. And then Sam, I’ll ask you the same thing.
Rimsky Denis Hello, everyone. My name is Rimsky Denis, and I am an interventional and structural cardiologist [00:02:00] here in Miami, Florida. I deal with a broad range of cardiovascular diseases, ranging from the management of hypertension all the way to the management of complex coronary artery disease and valvular disease.
Frank Jaskulke Oh, wonderful. Thank you. And Sam, what about you?
Sam Hoeffler My name is Sam Hoeffler and I am the Director of Food Programs at Reinvestment Partners and we are an anti-poverty nonprofit based in Durham, North Carolina.
Frank Jaskulke Oh, fantastic. Thank you both for joining us. Sam, I might start with you. When I was reading up on some of the work that you’re doing, I’d seen this produce prescription program. Could you tell our listeners a bit about what that is and why it’s so important to the work that you’re doing?
Sam Hoeffler Of course. So, a produce prescription is when a healthcare provider says to their patient, to improve your health I want you to eat more fruits and vegetables. So, through our contracts with health insurers, partnerships with clinics, and even [00:03:00] projects with the Veterans Health Administration, we’re working to make sure that that food that the doctor wants you to eat is paid for just like a prescription. We want to make sure that if a doctor or healthcare professional recommends using food as medicine or food instead of medicine, that that food is paid for just like any other prescription. And the way that we’re doing that is through a program called Eat Well, Eat Well provides money each month for participants to spend on fruits and vegetables of their choice. We leverage technology to make the enrollment and shopping experience as easy as possible. Eat Well participants use a prepaid debit card that reloads each month to buy their fruits and vegetables so that they can shop when and where they want.
Frank Jaskulke Very interesting. Okay, and how long has this program been going on? How’s it gone so far?
Sam Hoeffler We have made so much progress since we began this project in 2018. I think in part this is due to our focus on making sure that this model can meet the needs of health care [00:04:00] payers, providers and participants. And so for us, we keep participants at the center of everything, even as we build a program that can meet compliance requirements and manage data security and deliver high quality services and scale across geographies and lines of business. And we want, Eat Well and programs like it to be a covered benefit for anyone who needs it. We have the potential to unlock long term funding from the healthcare sector to pay for healthy food. And that’s what we’re really trying to do. And we’ve served a hundred thousand people so far.
Frank Jaskulke Oh, wow.
Sam Hoeffler And our participants, yeah, they spend a million dollars per month in fruits and vegetables right now at their local retailers. So, it’s… for me, just so incredible to know that folks are able to buy the fruits and vegetables that they want for themselves and for their families and that those fruits and vegetables are improving their health. We are embedded in the health care sector. Now we have been able to show not [00:05:00] only that food can be prescribed at a doctor’s office, which is the first proof of concept, but also that patients will spend the money if it’s easy to use and allows them to choose what’s best for them and their families.
Frank Jaskulke Oh, I love hearing that. Thank you for describing that. And I might ask you, Dr. Denis, you know, I think that that may be an example of a community-based initiative, but maybe you could give our audience some perspective from the physician side on this idea of like, what do we mean when we say community-based initiatives?
Rimsky Denis Certainly, when we speak about community-based initiatives, we’re speaking about initiatives that are primarily driven by individuals who live and reside in the community. That we’re referring to these individuals who work, they live, they commute, and they are active participants within that community, and they take a direct and active and a forefront approach to resolve a program or, a problem rather, that has deemed to be necessary to [00:06:00] address in their community.
Frank Jaskulke Ah, very interesting. That, that sounds then you would be working with them as opposed to, or not as opposed to, but instead of for them. You’re partnering with them on the issues they’ve identified as critical and important.
Rimsky Denis Exactly. They’ve identified these, these issues as critical needs and critical issues that they would like to be addressed, and they take the brunt of the initiative for the most part in addressing these issues and with assistance from other community partners and other organizations the issue is tackled and it’s addressed head on.
Frank Jaskulke Oh, very interesting. And I think I’d seen something you’ve worked on or worked with. Is this a CHAT program or C H A T program? What’s that?
Rimsky Denis Sure. As a member of the Association of Black Cardiologists, I currently serve as a member of the Community Programs Committee. And one of the things that we do on an annual [00:07:00] basis is, we put on multiple events and we put on multiple programs to address health within different communities throughout the nation. The goal of the committee in and of itself is to engage the community and healthcare political systems and efforts to reduce disparities in cardiovascular health, which has been experienced, disproportionately by African Americans. And we have programs that are designed to educate African Americans on heart health issues and to learn how to take a more proactive approach towards addressing cardiovascular risk factors that affect their health and wellbeing. And the CHAT program, which stands for “community health advocate training” is an initiative whereby we train individuals in the community. These are individuals who go to churches in their communities. These are individuals who work in the community. These are individuals who are from different [00:08:00] organizations. We train these individuals on how to identify certain risk factors. and also to educate other individuals in their community, whereby they can promote healthy living.
Frank Jaskulke Oh, very interesting. And maybe one more question kind of related to that. You’ve been an advocate for community health fairs, and you mentioned the events. What’s the role of a community health and why is it so important, even in this age of, you know, digital communications and information everywhere?
Rimsky Denis Yeah, I think that’s a great question. I think community health fairs are very important because they address a need in many communities that having it, simply having insurance, does not address. So, many individuals and communities have barriers to accessing health care that make it difficult for them to achieve optimal health. So, by having community health fairs, we certainly address the cost barrier, whereby we’re [00:09:00] providing free or low-cost services to the individuals in their community. Oftentimes, it’s on a weekend, so the issue with regard to going to work or not being able to attend the event that that’s addressed. In addition to that, the community events that we typically do such as a health fairs, it’s usually done with the assistance and with information that is provided by the community in efforts to decrease some of the social determinants of health barriers that oftentimes preclude individuals from achieving optimal health.
So, I think community health fairs still have a role in identifying and screening individuals who have a broad range of cardiovascular health issues or general, you know, health issues who have not been seen or have not seen a medical professional in many years. And then when we identify these individuals, our goal ultimately is to connect them with an organization [00:10:00] or a healthcare provider whereby their health can be managed much more effectively moving forward.
Frank Jaskulke Interesting. Well, then, Sam, in the work you’re doing, I have to imagine, maybe there’s similar strategies or other strategies you’re taking to engage in the communities, whether it’s relative to the food program or other efforts. Could you talk a bit about, you know, the work you and Reinvestment Partners do in partnership with the communities?
Sam Hoeffler Of course. when I think of community based, I really think about connection and what we’re able to do as an organization in service of people’s needs to keep patients at the foundation of every single decision we make. We’re not thinking of shareholders. We’re not thinking of anything else. And I think that’s such, such a gift to be able to really genuinely center what is best for folks. And not only are we able to listen to the way that people want to receive benefits or the way that people kind of speak of their own health, we can do [00:11:00] all of that and integrate what we’re learning from folks into our program and into our program design.
And so we are really thinking about how to get the most money to as many people as possible. And any additional funds that we access through this model are reinvested in the pressing needs of folks, especially for us who live in Durham, North Carolina, where the cost of living is rapidly increasing and it seems like everything is more expensive by the day. So we reinvest our funds in affordable housing that we, you know, we’re rehabbing or managing. We’re making sure that we have housing counselors that keep people in their homes or guide them through the home buying process, keep them from being evicted. And then also we do that work through our produce prescription. We focus on neighborhoods in Durham that don’t have access to food or have kind of lower income areas of Durham and, and we focus on, on those areas for our [00:12:00] produce prescriptions. So I think what’s interesting and what’s important about community-based interventions is that they’re deeply informed by folks on the ground. And I think that’s such an asset as we kind of cross that bridge into connecting into healthcare and corporate healthcare. So I think it’s a really cool role that we get to play.
Frank Jaskulke Yeah. And in that health care piece, and I’ll be interested to get both of your perspectives on this. Sam, you had talked about, you know, interacting with the providers and a doctor may give a prescription for the food. What is that like interacting with the provider community and developing those relationships and maybe moving something along that isn’t as traditionally part of the healthcare establishment?
Sam Hoeffler I think that that’s one of the parts that I’m really excited about, is this idea that we can redefine what it means to care for someone.
So, one of the things that we’re doing is focusing on something called affirmative outreach that I’m really excited about. And [00:13:00] what it is, is so often we hear from folks that it’s really hard, it’s really hard, to figure out how to navigate the health care system or if you’re thinking just generally of assistance or other kinds of benefits that it’s a challenging. And I think you could argue that it’s challenging on purpose in some ways, but I think what we’re trying to do with affirmative outreach is to say to people, or want to figure out, using their healthcare data that already exists, right? So let’s say we want to target someone with hypertension. Their medical provider, or their health insurance company already knows that they have hypertension and so they can basically recommend this program to them. They can let us know and they actually can even send them a text message that just says, hey, you’re eligible to get 100 per month in fruits and vegetables. And we develop something where they can just enroll online. So they’re sitting in their home. They get a text message or an email from their provider saying, hey, we want to care for you in this way. And we think you would benefit from [00:14:00] this. They enroll online and they get their prepaid debit card in two weeks in the mail. And we’ve done this with lots of different health partners and we’ve enrolled 5,000 people in the span of four weeks’ time. And imagine that experience for that person, right? They’re sitting in their home. They’re kind of realizing that whoever their insurer is, it’s like, oh my gosh, they’re kind of thinking about me. They actually care about me. They’re doing something that’s either preventative in certain cases or a treatment in other cases, facilitating that healthier diet for them. And so what we’ve seen is that people really enjoy it. And we’ve noticed that the healthcare companies also really, really benefit from that because more in their terms, they’re seeing member retention. They’re seeing member engagement, right? And this could be a tool to redefine the relationship that they have with their patients and get those patients in for additional services. So we’re, I’m very excited about this idea of affirmative enrollment. And I think that it could be something really special where we’re kind of trying to redefine what that relationship is[00:15:00] from the patient side with their health care provider and allowing the health care provider to treat them in a new or kind of different way and have a different path to do that with having the community based organization as the link.
Frank Jaskulke Indeed, and Dr. Denis, I know in your field in structural and interventional cardiology there’s often new interventions, new procedures, new therapies that are coming on. But I think for a lot of our listeners, we’re, we’re hoping to convey to them, as both of you have shared already, different tools that they can use to engage. One other thing I’d seen mentioned in your work was this barbershop hypertension initiative. So maybe continuing on the topic of hypertension for a moment, can you talk about what that initiative is and the sort of impact that it has?
Rimsky Denis Certainly. So through the Association of Black Cardiologists, I’ve been fortunate to participate in their Barbershop Hypertension Initiative. Which essentially is an initiative whereby [00:16:00] barbers throughout the entire United States are trained on different cardiovascular disease risk factors, including hypertension, diabetes, obesity, smoking, physical inactivity, and hyperlipidemia. These individuals receive training on how these chronic conditions are managed, how they’re treated, and the ways in which they can ultimately be prevented. We also discuss different ways in which these conditions are screened for. So the barbers receive a host or a wealth of information with regard to these chronic diseases. In addition to that, the barbers are trained on how to properly obtain blood pressure measurements with a blood pressure monitoring device. The barbers themselves are then charged with the task of going out into their communities and providing [00:17:00] this information to their clients. And if a client is interested in receiving their blood pressure or having their blood pressure measured, rather, the barber can further do so within the barbershop. And if individuals are found to have elevated or blood pressure results that are out of range, those individuals are then referred to different community organizations or health care providers whereby they can receive proper follow up. So this initiative was started many, many years ago by Dr. Elijah Saunders who was an Association of Black Cardiologists member and has revolutionized screening particularly within minority communities for about three decades, three or four decades now. So we’ve been able to identify individuals who have a host of chronic diseases in addition to hypertension. And we’ve been able to plug those [00:18:00] individuals into the different healthcare systems and different organizations within their community, whereby they can receive follow up and proper treatment.
Frank Jaskulke Oh, that’s fantastic to hear, especially the, the longevity of the program. You know, there aren’t a lot of things that we get to hear about where they’ve had that sustained impact and the breadth of impact that you just described. Sam, what that makes me think of is, you know, the importance of cultural competency and inclusivity in the work that we’re doing. How do you think about that or how does that play out in the work that Reinvestment Partners is doing?
Sam Hoeffler That’s a great question. I think it’s so important and one of the things that we’re most adamant about is that folks should be able to choose the fruits and vegetables that they want and like, or that work with their diet, or their storage situation, or their cooking capabilities, or whether or not they have a fridge. All of these things come into play, and it’s a really foundational part of what we’re trying to do is to trust people to know [00:19:00] what their bodies need. And in large part, we’re offering fruits and vegetables because that’s kind of the only thing that everyone agrees is healthy. So that’s where we’re starting.
We’d like to see, you know, additional foods included. And I imagine that will happen over time, but I think there’s still a bit of debate as far as what should be included or not. So right now we’re focused on that and we’re hoping that by connecting people with funds for food, we essentially free up money and their overall household budget to allow them again, we’re focused on the autonomy. So now they can spend their money and different ways to, whether it’s to improve their health or, you know, meet their basic needs, these are, these things are linked. And so I think we’re really focused on allowing people to choose what they want to do. And we’re trying to make it as easy as possible. We’re trying to make sure folks are not applying or renewing or having to share, you know, income information with us. [00:20:00] And so in doing so, I think that people feel, my sense and when I talk to folks is that they can feel the difference. You can feel that we actually care for them. We’re trying really hard to make this as easy as possible for them.
Frank Jaskulke One last question I’ll ask both of you. I think we know healthcare and public policy are so closely linked, for good and for bad. And I always like to ask our guests, you know, when you look at the public policy realm, are there things we should be working on or doing more of or doing less of? Like what would be each of yours advice to policymakers who might be listening? Sam, I might start with you and then Dr. Denis finish with you.
Sam Hoeffler This is the question I think we could spend five hours on. Yeah. So I think it’s such a good question. And I think, I think it’s the right question. So we, for me, I think simply put, we should be insuring more people. So what we’re doing is really working through the health insurance system to, [00:21:00] use that as a funding mechanism for people to have access to money for food. And we know that not everybody is insured. So I think that that is a public policy question, right? Is to get everyone insured and then also to improve the quality of health care that people receive when they do have health insurance. Those are two key things. And I think when it as it relates to food as medicine, or the food as medicine movement, I think there’s a ton of potential here as I mentioned to kind of reframe and redesign how we’re caring for people and how we think about improving health. So I think it is transformative to imagine that there’s someone providing healthcare for you, whether that’s a doctor or another professional that actually sees you and wants to care for you in a way that’s rooted in connection and rooted in dignity and trust, right? And that’s what I mentioned before. I think trusting people and trusting their bodies is a key piece here. And I also think about political will. We know, and [00:22:00] Dr. Denis can attest, that a diet rich in fruits and vegetables improves health outcomes. We know that, right? So we need something to push us toward actually paying for that.
We have shown with EatWell that we now have the mechanism to connect people with those fruits and vegetables that that their provider is suggesting that they eat and so we are seeing a bit of a culture change within health care where they are thinking about this idea very seriously and more importantly they’re thinking about how to pay for it. We know there are champions within the health care sector who absolutely understand the importance of doing this. I think that from the outside and from a policy perspective, I think we can think about how do we push this on terms that serve people who are in need today, right? I don’t think we have to stop and defer to the timeline of the healthcare sector. So I like to see, you know, evaluation and research used strategically. I would like to see [00:23:00] different mechanisms to pay for these initiatives explored. We’re seeing in lieu of services out in California which is laying the groundwork for possibly a path toward treating these as covered benefits. And then I think we’re also seeing in addition to that, in lieu of service mechanism, we’re seeing creative ways that healthcare partners can get these initiatives to fit within that medical loss ratio, right? So there are lots of different ways to do this. And I would just say, I’m not exclusively relying on champions within the healthcare sector. I think that we can also find ways to push forward and in some ways hold their feet to the fire where we know this is important, and so we kind of are at a point where we need to put our money where our mouth is and figure out ways to creatively fund this for folks because it is urgent and it is affecting their health right now, and it’s also affecting their health in the long term.
Frank Jaskulke Thank you. And, and Dr. Denis, I’d ask for your perspective as well. You’ve, you’ve been involved with the Association of Black Cardiologists. Healthcare is [00:24:00] so rooted in policy. What’s your take on where we should be focusing?
Rimsky Denis Certainly. first and foremost, I agree 100 percent with everything that Sam stated and I echo her sentiments 100%. In addition to that, you know, I would simply add that we certainly have to increase the number of individuals who are insured in the United States of America. And I think that’s something that we as a community, as a nation, should and can do a better job in addressing. In addition to that, I think that, increasing the number of individuals who are represented in clinical trials who come from minority or underrepresented or underserved communities I think is a key component with regard to the development of new pharmaceuticals, development of new therapies, and ultimately having a better understanding of how to address different communities from a host of different standpoints. So I think that’s something from a policy [00:25:00] standpoint that needs to certainly be addressed and something that we can do better on. And I think from a policy standpoint, we as health care professionals and individuals within the health care community, we need to do a better job at addressing health disparities, within our community. I think we need to tie federal funding and reimbursements to these desired metrics or decrease in disparity metrics. And I think if we can have reimbursements and funding, you know, tied to these desired metrics. I think we can certainly make much better strides with regard to truly seeing a real impact in these areas.
Frank Jaskulke Indeed. Yeah. That’s the old saying goes, you get what you pay for. I gotta say thank you to both of you for sharing the insights, the perspectives, and the experiences helping our listeners gain a new [00:26:00] perspective on community-based initiatives and how they might engage. So, Dr. Denis, Sam, thank you both so much for spending some time with us today.
Rimsky Denis Thank you. Thank you for having me.
Sam Hoeffler Thanks.
Frank Jaskulke And folks, that’s been another episode of the Medical Alley Podcast. If you’re not already a subscriber, make sure to get over to MedicalAlleyPodcast.org, or you can find us on Apple, Spotify, or wherever you go for your podcasts. And hey, do me one little favor. Would you share this episode with just one other person? If everyone listening did that, we’d help share this important story and so many other stories in this incredible community with more people in advanced health care faster. I’d really Appreciate it. Until next time, have a great day.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Health Equity
Published on
September 19, 2023
Listen on:
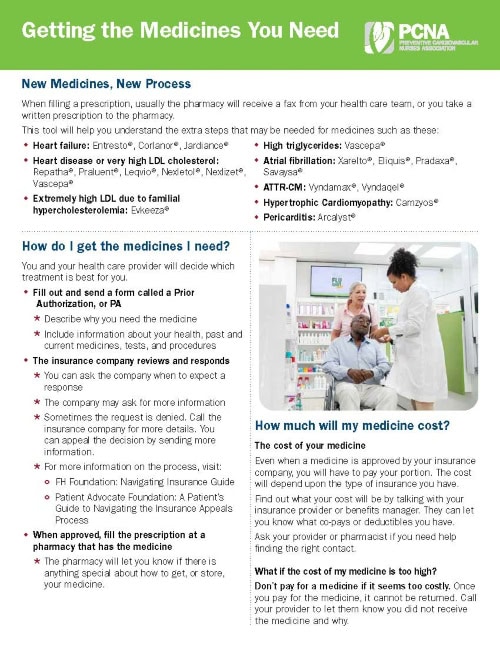
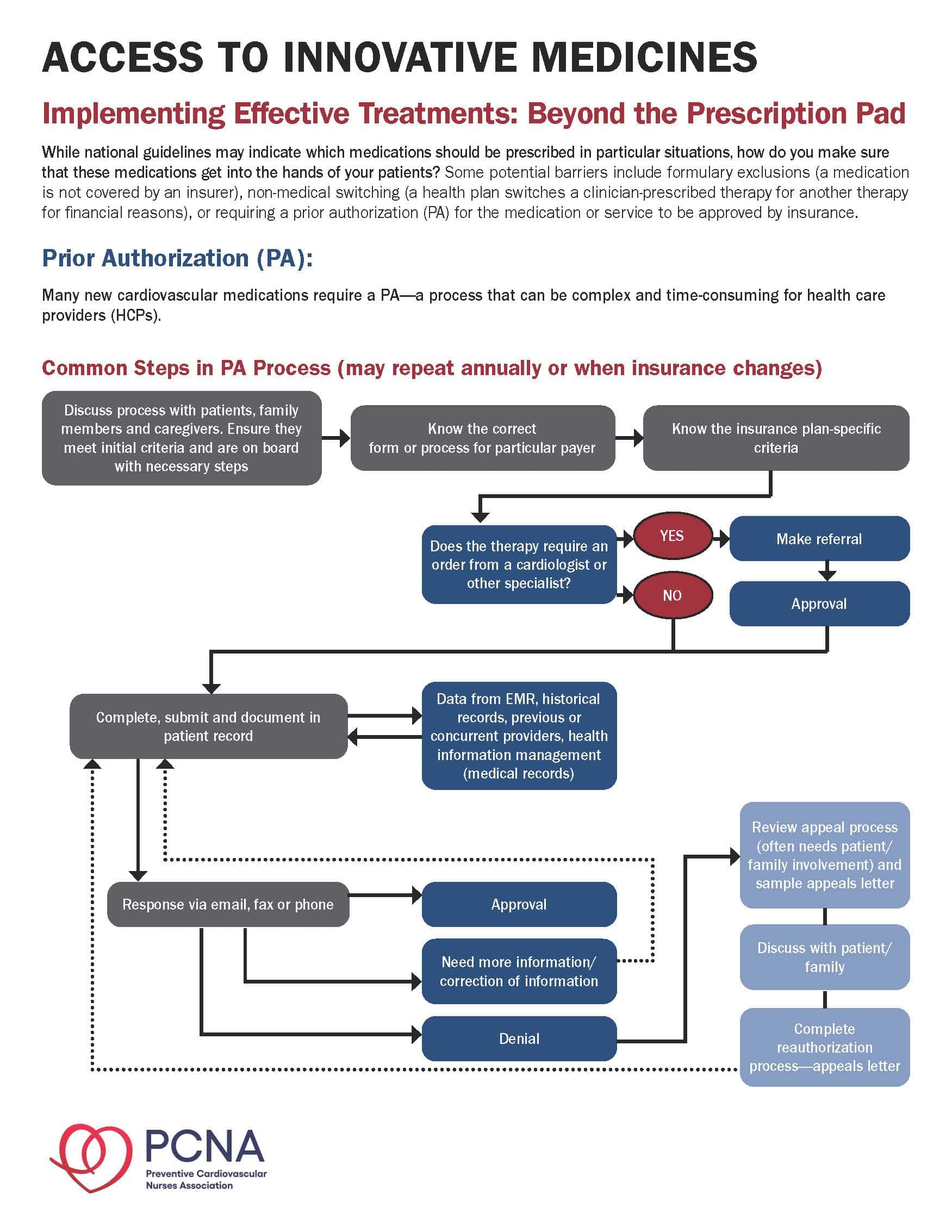
Related Resources