Current President of the Family Heart Foundation, Dr. Seth Baum explores the importance of cascade screening with FH patients. Learn how to navigate difficult conversations with your patients and connect with resources to help your patients cope with their diagnosis.
- PCNA FH patient tools
- Family Heart Foundation Resources
- Family Heart Foundation Peer Support
- Family Heart Foundation Cascade FH Registry
- Dutch “Foundation for Tracing FH” Concept
Supported by Regeneron Pharmaceuticals
Geralyn (00:20)
I’d like to welcome our audience to today’s episode, the final of three episodes on familial hypercholesterolemia, also known as FH. Our previous episode discussed the genetic implications for homozygous FH, also known as HoFH, and today we’re going to take a deeper dive into genetic testing for HoFH. Today’s guest may be familiar to our audience, but Dr. Seth Baum, could you please introduce yourself?
Seth Baum (00:43)
Sure, name is Seth Baum. I’m a preventive cardiologist. Originally, actually an electrophysiologist and interventional cardiologist. I stopped doing those about, I would say, 20 years ago, and have just focused on prevention and lipids since then. I’m the Chief Medical Officer for Flourish Research, and I’m also the chairman of the board for the Family Heart Foundation.
Geralyn (01:07)
Well, we are so excited that you’re spending time with us today to discuss this really important topic. And I’d like to kind of pick up where we left off at the end of our previous episode. So Dr. Baum, could you please remind our audience about cascade screening for HoFH? What it is, why it is important.
Seth Baum (01:23)
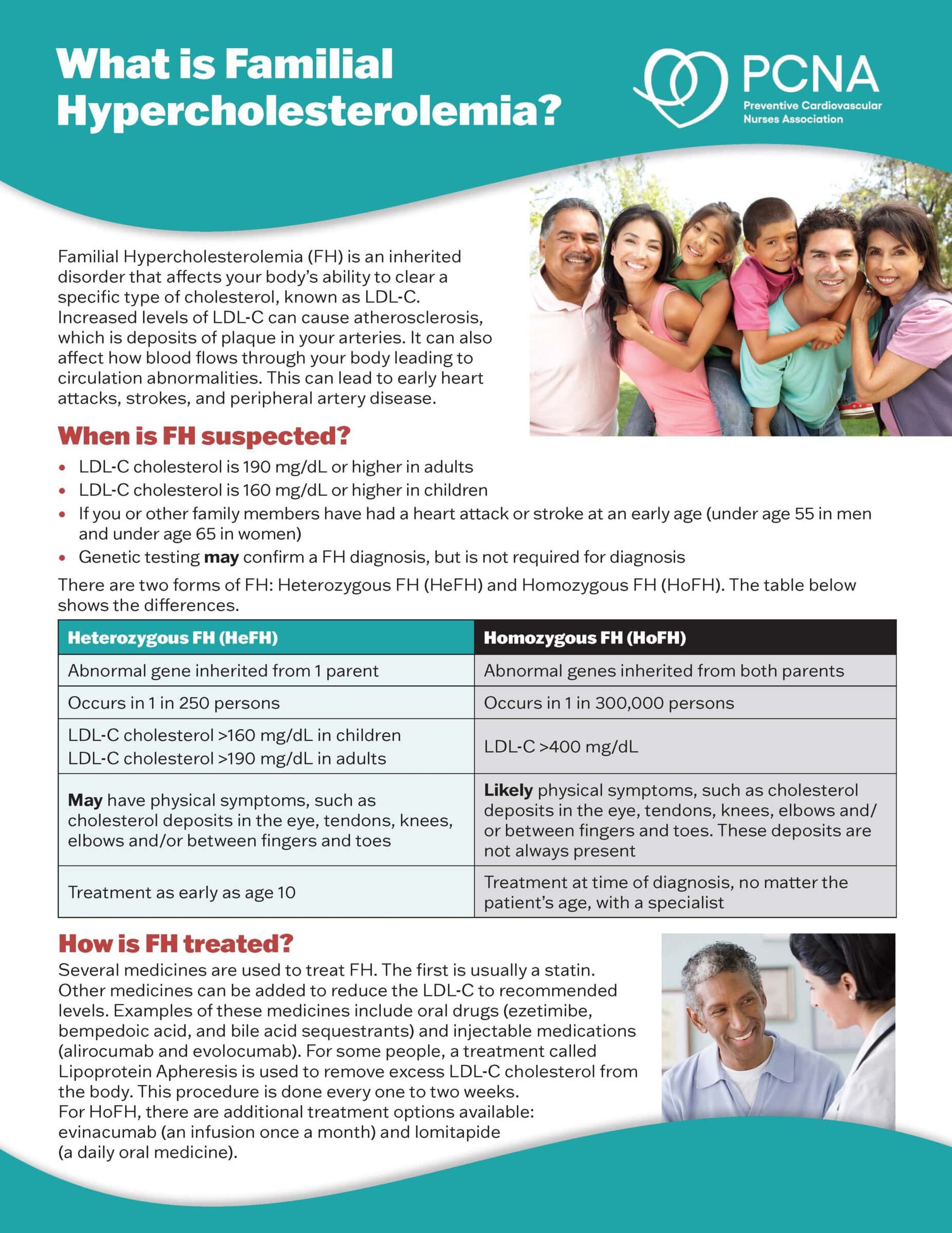
Sure. So cascade screening is important for FH period. Both heterozygous and homozygous FH. I just want to make that very, very clear. And you can apply what I’m about to say to both forms of FH. But today, of course, we’re talking about homozygous FH.
So what does cascade screening do? Well, first of all, we have to recognize that FH is truly a family disease, it’s a genetic disorder and it’s autosomal dominant. You have one mutation, you’re going to see the effect. The homozygous FH patients have two mutations. So they get one from mom and one from dad. And so if you think about it, there’s a larger group of people at risk because it’s on both sides of the family, a larger group of patient who may not already be identified and may therefore not be being treated appropriately.
So what do we do? Well, we take the index case, the individual we first identified, and let’s say that person has homozygous FH, and we say, well, let’s look at first degree relatives. Let’s go out and look at parents. Let’s look at siblings. Let’s look at children. And we see whether or not these groups of individuals have FH. They can have homozygous FH potentially; they can have heterozygous FH. So we look at all of them and we say, “Yup, you have FH, if you have FH, we go farther out.” So if it’s a parent, we can go to the grandparents, we can go to the uncles and aunts. You know, if it’s children and they have children, we go to their children. So that’s what we do.
In heterozygous FH, when this was done in the Netherlands, interestingly for every index case that was identified, when cascade screening was done, an additional seven or eight individuals with FH was identified. So it is incredibly important to do this. The sooner we make the diagnosis, the sooner we can treat and the better the outcomes will be.
Geralyn (03:47)
So I suspect cascade screening, much like a family history, can be hit or miss, if you will, in terms of some families where maybe they’ve lost touch with relatives or maybe there’s some outstanding circumstance that makes that conversation a little bit more difficult. Are there any suggestions or any things that happen in clinical practice that the clinicians listening to this particular episode would need to keep in mind as we’re thinking about cascade screening for families?
Seth Baum (04:13)
It’s a great point. It really is a great point and it is incredibly challenging because there are all sorts of family dynamics that get in the way oftentimes of cascade screening. I’ve had patients say to me, “I can’t talk to my sister. She’ll hang up on me. That’ll be the end of our relationship.” or things like that.
So it’s challenging. It requires a lot of time on the part of the clinician. And I think the best way to approach it is to emphasize that individuals with FH, you can liken to individuals with, frankly, with cancer. You wouldn’t leave these people untreated, unidentified and untreated. We have to identify them in order to treat them in order to prevent outcomes such as heart attack, stroke, or death. And these events can be premature especially in the homozygous FH patient population.
Geralyn (05:14)
So when we’re thinking about cascade screening and obviously that index case, that patient that’s sitting in front of you is the one who is the primary reason for this to happen. What is the role of the clinician who’s working with that patient and the patient themselves in actually getting this cascade screening done? Does the patient call their family or, you know, connect with their family? Does the patient say to the clinician, “Gosh, you know, I need some more information to share.”? How does that look in clinical practice?
Seth Baum (05:45)
So it can appear multiple ways actually. You can have a family, a patient who has a family that’s very tight, very close and the patient might say, “I can do this, I can handle this. I’ll make the contacts with my family members, and I’ll use you as a resource if need be.”
Alternatively, you might have a patient who says, “I can’t reach out, but I’ll give you my family members names and you can contact them.” When that happens it’s always best to have the patient reach out to the family members first so that they’re not getting a cold call. You know, “ Hey, I just want to talk to you about a genetic disorder you might have.” so you know it’s much better to forewarn them.
I would just re-emphasize the importance of doing it. It is our best way to identify the certainly 70 to 80% of patients with FH who have not yet been identified. And that, believe it or not, holds true with homozygous FH as well. A large number of patients with homozygous FH may be surprising since their LDLs are so high, but a large number have not been identified and need to be identified.
It’s important for physicians to engage actively in the process.
Geralyn (07:12)
We’ve been talking with Dr. Seth Baum about cascade screening for HoFH, and we will be right back.
We’re back to continue our discussion about genetic testing for hypercholesterolemia. And as we’ve been discussing cascade screening and family dynamics, I can’t help but think about the emotional toll that this must take on patients and their families. As you described earlier, it’s much like when we talk about cancer, the diagnosis, and knowing that what you are experiencing yourself might be also impacting family members and maybe there’s some guilt, maybe there is some reticence about sharing that with anybody. We don’t want anybody to know about this thing that we’re dealing with.
So, since HoFH affects multiple generations, how do you address this kind of emotional piece with patients?
Seth Baum (07:58)
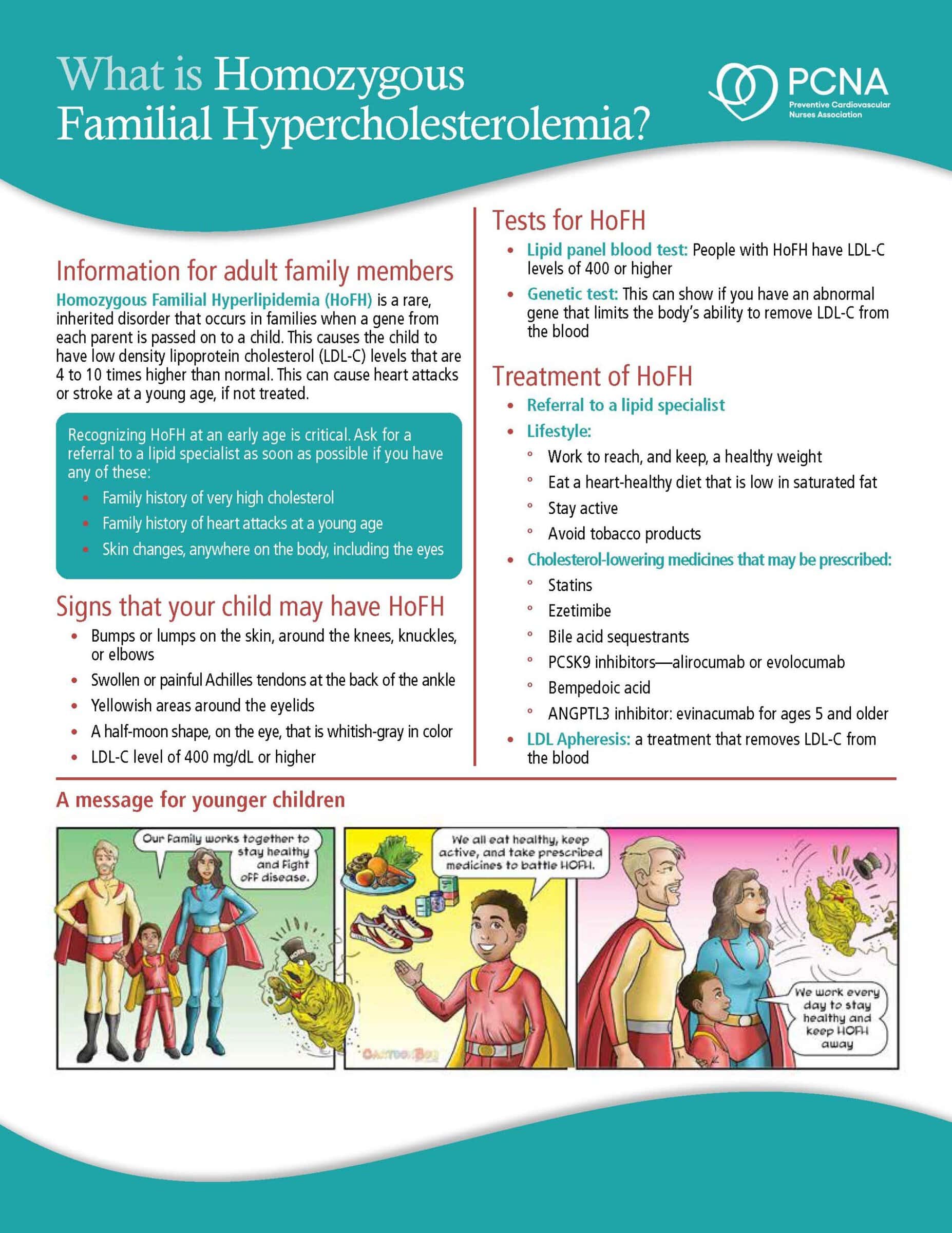
Yeah, great question. First, I’d say it really depends on the age of the patient who’s been identified, that index patient. If it’s a child, it becomes even more challenging from an emotional standpoint. So now you’ve shared with the family, the parents, that the child has something that could be, as we say, akin to a cancer. So now you’re dealing with a pediatric cancer.
It’s just terrifying. Patients can often feel as though there’s no hope. So one of the things to do is to reassure individuals that identifying HoFH early is always a good thing. There are many, many therapeutics that we have available. Even in pediatrics, there are drugs that have been approved that have really changed the approach to HoFH and improved, dramatically improved LDL levels. I have patients who’ve gone through clinical trials, pediatric patients who started with LDLs in the seven, eight hundreds, and now on these new meds, LDLs are in the hundred range.
So, imagine that. This was not possible, you know, five, ten years ago. So we’ve really made tremendous inroads into the treatment and management of these patients.
So I would say, you know, we need to recognize the emotional toll this takes on the family, but then we need to also encourage the family and reassure the family that we have therapy, that it’s good that we’ve identified it. And now we have to go, as we spoke about before, and cascade screen, see who else might be affected in the family and aggressively treat those individuals.
Geralyn (09:56)
So do you have any resources that you could point our audience towards in terms of helping our patients better understand the disease or the process?
Seth Baum (10:06)
Yeah absolutely. So the Family Heart Foundation. So I am the chairman of the board of the Family Heart Foundation and that’s an organization that was established over 10 years ago to address FH now also Lp(a) or lipoprotein small a and it’s an advocacy organization a research organization an educational organization. It’s really a very substantial group with tremendous resources that are now over 200 ambassadors who have been trained to go out to the communities to help people who have FH or Lp(a). [They have] tons of resources in terms of finding clinicians with expertise in HoFH and people who they can talk to, the patients can talk to and actually you know, have an emotional conversation about this and the toll that it’s taken.
In terms of research, specifically with regard to HoFH, the Cascade FH registry is something that was started many years ago by the foundation. And for HoFH, there were 67 or so patients who were identified. Most of those were genetically determined to have HoFH, I believe it was 40 is the number.
And there were a lot of learnings from that.
One example is there was a genetically confirmed patient with homozygous FH with an LDL over 500, xanthomas as a child, family history of high cholesterol in both parents, family history of premature ASCVD in both parents. So classic definition of homozygous FH.
And yet the genetics in that individual were negative. Not a single pathogenic mutation was identified. So what that tells us is phenotype always trumps genotype. So if you have a patient who meets criteria for homozygous FH and the genetics are negative, the patient has homozygous FH. And that’s very, very important for multiple reasons, not the least of which is there are medications specific for homozygous FH patients, you do not want to deny a true homozygous FH patient one of those medications.
Geralyn (12:41)
We will be sure to put those resources in the show notes for this episode so our listeners or those watching this will be able to access those very easily so make sure you check those out for those of us that are interested in that. I have one final question for you. We’ve talked about a lot of different things today. What would be your one key takeaway for our audience?
Seth Baum (12:59)
The one key takeaway is that you may see a patient with homozygous FH in your practice. You may already have a patient with homozygous FH in your practice. You certainly have many patients with heterozygous FH. Don’t forget, one in 200 or 225 individuals has heterozygous FH. It’s about one in 300,000 with homozygous FH.
These patients are around and they’re under diagnosed, they have not been identified. And we have to always remember if we don’t know what the patient has, we’re not going to treat the patient accordingly and the patient’s going to suffer. These patients have a very, very high risk of premature heart disease. There are children with homozygous FH who die before the age of 10 from heart attacks or have bypass surgery before the age of 10.
And there are many therapeutics that we can administer, many approaches we can take to mitigate that risk. So please, please always have FH on the tip of your diagnostic tongue and always approach each patient who has a markedly elevated LDL or a strong family history premature ASCVD as someone who might have FH or homozygous FH.
Geralyn (14:20)
We are so incredibly grateful to Dr. Seth Baum for spending time with us today speaking about HoFH and for encouraging us to be vigilant in the patients that we’re seeing and those diagnostic cues that can help us get individuals diagnosed and then treated as early as possible.
This episode is part of a three-part mini-series exploring familial hypercholesterolemia. And again, we encourage you to check out the show notes for additional details and also to listen to the other two episodes. We’d like to Regeneron Pharmaceuticals for their unrestricted grant funding for this mini-series. And this is your host, Geralyn Warfield, and we will see you next time.
Topics
- Lipid Management
Published on
February 18, 2025
Listen on:
MD, FACC, FAHA, FNPLA, FASPC
Related Resources
Patient Education Handouts
What is Homozygous Familial Hypercholesterolemia? Fact Sheet
August 06, 2025