Healthcare advocacy takes place in the clinic setting and in legislative chambers, and impacts the access patients have to needed therapies. Hear from Dharmesh Patel, MD, from the Partnership to Advance Cardiovascular Health about the Inflation Reduction Act, the MINI-Act, and being the voice for the voiceless–our patients.
Dharmesh Patel podcast episode transcript
[00:00:00] I’m Erin Ferranti, board president for PCNA, and I’d like to welcome you to this episode of the Heart to Heart Nurses Podcast. PCNA is the proud home of cardiovascular nurses and one of the leading figures in the fight against cardiovascular disease. We have the resources you need for your day-to-day practice or to follow your passion to new areas of learning and growth.
Geralyn Warfield (host): 00:19)
I’d like to welcome our audience to today’s episode where we have the great pleasure of speaking with Dr. Dharmesh Patel. And could you introduce yourself to our audience, please?
Dharmesh Patel (guest): (00:26)
Good morning, Geralyn. My name is Dharmesh Patel. I’m a preventive cardiologist practicing in Memphis, Tennessee. I’m a lipidologist with a focus on prevention. And I’m also the President of an advocacy alliance called PACH, which is the Partnership to Advance Cardiovascular Health.
So, very happy to be here, Geralyn.
Geralyn Warfield (host): (00:46)
Well, we know that you have a great affinity for, and a lot of expertise, discussing healthcare advocacy, and I’m hoping you could address that with our audience today.
Dharmesh Patel (guest): (00:56)
Yes. I think my journey really begins about 10 years ago. And I think you probably will recall we had the blockbuster therapies like PCSK9s which came onto the scene. And I was extremely excited to be able to give my patients a therapy that could lower cholesterol by up to 60%.
Dharmesh Patel (guest): (01:15)
But as you well know, Geralyn, when you are in the patient’s room now, there’s not just two people in the room.
There’s you the healthcare professional, the patient, but also the insurance company. And I hate to say it, but even as I practice today, I practice depending on the patient’s insurance type, not on the disease they have, which I think really is quite poignant.
And what happened is, 2015 to 2018, I had patients who basically had LDLs greater than 190, or with genetic high cholesterol, or patients who had LDLs of let’s say in the hundreds who had already had cardiac events.
And I was excited to give therapies. But low and behold, insurance companies would stop it or block the PCSK9 therapy. And I felt that that was a real call to action for me. I felt that we had therapies that could really make a difference in patients’ lives. Yet, they were not able to get groundbreaking scientific FDA-approved therapies.
And for that reason, I really became a bit more involved in advocacy, because at the end of the day, the patients really had no voice. We are the patient’s voice.
And I’m so excited to be here at the PCNA [conference] because we all appreciate that it’s
a team effort. And it’s a known fact that patients and general public trusts nurses, trust nurse practitioners, way above any other profession in the country.
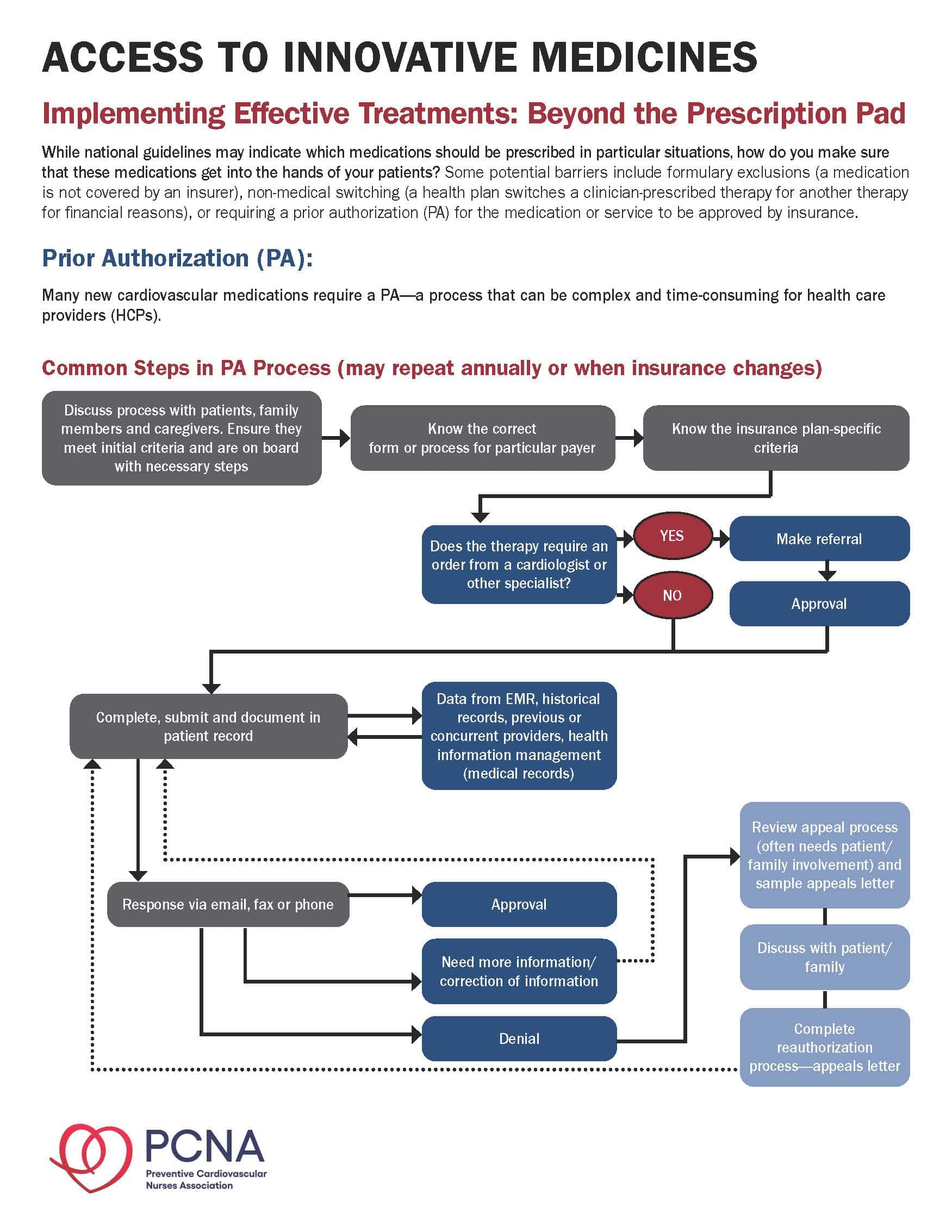
So with that being said, I feel that being here is just another way to communicate how we as a team can really change policy. Because, as you are well aware, there are many different barriers to healthcare access. We are all very, very familiar with barriers like prior authorizations. Step therapy. Copay accumulators. Exclusion formularies.
All ways of really putting barriers for us to help patients. Because, at the end of the day, we all went into this profession really, I think, genuinely to make a difference in patients’ lives.
I don’t think we were trained to fill out prior authorizations. And, you know, the sad fact is the average clinic in the United States, the average person in the office spends 13 hours a week on prior authorizations.
That’s essentially a full-time job.
And you know, I think there has been some changes, but I really do think that we have a very huge way to go.
As you are probably aware, the government did introduce things like the Inflation Reduction Act [IRA]. And a lot of people don’t know what the Inflation Reduction Act, but it’s a policy that really predominantly in the healthcare sector, to reduce the price of therapy.
Now, I think that’s very important, but there’s always two sides to a story.
For example, 5 of the 10 IRA therapies were cardiovascular medicines. And I think it’s important because we want our patients to get therapy. So, there has been some negotiating with the government and industry to make these therapies more affordable. They’ve made them fixed.
Now, that’s important. And so, things like the fact that insulin now is only $35 per unit for patients. These are very good things, just like the Medicare caps are $2,000 for patients if they have a catastrophic event. And I think those are really, really important things. And I commend those movements.
But please also understand on the flip side, as healthcare professionals, we are always looking for evolving science and new therapies in cardiovascular arena. Industry will, I think, appreciate the fact that, you know, with Inflation Reduction Act, the bottom line is, as much as that healthcare is important and access to care, I think money matters.
And as a result, the Inflation Reduction Act can also have unintended consequences. For example, if the cost of therapy is less, then maybe, who knows if prior authorization’s exclusions therapies will become more pronounced in the cardiovascular arena. We don’t know that yet.
We also don’t know the fact that with the Inflation Reduction Act, genetically treated therapies will be reduced in their patentcy life from 11 to 7 years.
So, therapies, or companies that have been making blockbusting therapies, may realize it’s not “so cost effective” anymore to put millions and millions of dollars into cardiovascular outcomes when the lifespan of the therapeutic would be seven years.
These are things that are interesting. It’s a dynamic conversation. We don’t exactly know where this will end up. But I think it’s really important to understand some of the nuances and forces that we have when we talk about advocacy.
Now, on the flip side, let’s look as people in the “trenches,” we have made a difference.
For example, with step therapy, we know that there are 140,000 patients affected with step therapy when one DOAC was changed to another DOAC. And as you probably would be aware, lots of patients were confused. They didn’t take their therapy, increasing risk of strokes.
And the PACH organization, the Partnership for Advanced Cardiovascular Health, really helped be that advocate for the patient. And we reversed 140,000 lives on step therapy and that the insurance company did retract and stop that.
Other examples include, for example, PCSK9s in California. In 2020, one of the biggest insurance carriers in California decided they will stop PCSK9s. Period. And we fought that with some of our key opinion leaders, including members of the PCNA, sending a letter to the insurance company. And lo and behold, about two to three months later, that was reversed.
Now on the whole legislation side, we have made lot of changes in terms of advocating, for example, about prior authorizations. And in 2022, a bill has come out talking about the fact that prior authorizations need to be more streamlined, and responses need to be more efficient and quicker.
So, I think these are all things that we are doing to try to help, at the end of the day, the person that’s voiceless—that’s the patient.
So, I’m really excited that we have lots of things coming down the pipeline. There are things like the MINI Act, which is an act really to talk about, you know, should some of these small molecules be given a higher half-life, or what should I say, from 7 to 11 years. Please understand, Geralyn, that, you know, one thing we don’t appreciate is that cardiovascular trials, they are generally more riskier, they take a lot longer. They are very expensive.
And so if we were to stop what has made this country great, which I think is innovation, new therapeutic modalities in cardiovascular medicine, we also don’t want to suffocate the science and the industry that has brought [those] great therapeutic advances to our patients.
So there has to be a happy medium in there somewhere. For every action there’s always a reaction. So, I think as long as we all appreciate these different things, I think that’s key.
Another one of my nuances is we know, think healthcare professionals, people in general think that a lot of healthcare costs are driven by healthcare professionals and by industry. But please appreciate the fact that there’s these people called pharmacy benefit managers, the middlemen. A group of people that basically are contracting therapies to our patients.
And we do not need to forget that this is a huge industry with around $9.1 billion made in 2020. Pharmacy benefit managers, I do feel, incur unnecessary cost to the healthcare system. Fortunately, the Fair-Trade Commission has looked into pharmacy benefit managers too, because 77 % of all prescriptions are controlled by pharmacy benefit managers.
And so, I do think that it’s no surprise that out of the top seven Fortune 500 companies in the United States, two of them are healthcare companies. United and CVS are two of the top seven companies in the country in terms of revenue and profitability.
And you know, it’s kind of somewhat of a monopoly, in my opinion. We have an insurance company that basically owns the pharmacies or tells the pharmacy which therapies to give.
And then they also own the patients because the insurance plan is essentially a vertical monopoly, a silo that basically, is made profitable from the top all the to the bottom to the patient.
So, you know, I do think businesses should, of course, be profitable, but I do think that when we talk about healthcare costs and the amount of money that’s wasted in healthcare, I do think there has to be some accountability for insurance companies.
And they cannot be bigger than let’s say the Fords or the Googles for no reason. So, I really feel, you know, it’s important. I think recently the Wall Street Journal talked about the fact there’s been over a million denials for patients by healthcare insurance companies. I think, you know, this doesn’t need to be this complicated. I think these are purposeful barriers so that our patients don’t get the therapy that they need.
Geralyn Warfield (host): (11:14)
I am very grateful to you for providing that well-rounded view of what it’s like to be a healthcare professional in today’s marketplace. And it literally is a marketplace. And I can only imagine how complex it is when a patient comes in. You are using that lens of insurance coverage to determine what therapies to provide to them.
You write a script; they take it to the pharmacy. And they may or may not be able to fill it for a variety of reasons. They get confused. They might not fill it. So even your best intention in that clinical setting doesn’t necessarily result in that, even that one, that one therapy that you have determined is of benefit to the patient, maybe not the best benefit because it’s not going to be covered by their insurance. There still are barriers.
And so, I think you are astute in noticing that patients are very confused, they do feel a little lost. They don’t understand why they can’t get the medicines that they hear about, or that you’ve talked about, or that they think that they need, or they’ve researched, or their provider has said.
And I think the other issue is that when they have to change insurance, maybe they’ve changed jobs and the therapy that they’ve been on now for however long now is no longer covered.
There’s a lot of transitions that I think are unnecessary, in my personal opinion, that really put additional barriers on those patients. So, I applaud PACH for what you’re trying to do in terms of leveling the playing field to ensure that patients do get the access to the medications and the treatments that they need.
So, you’re a great partner with PCNA in terms of trying to educate individuals, be they nurses or other health care professionals, as well as patients in terms of what’s happening and what can be done, what potentially could be said. So, thank you for doing that as well.
Dharmesh Patel (guest): (13:11)
Thank you, Geralyn. And you know, to your point, when we give the prescription to the patient, let’s talk about what happens next. Because, a lot of times, patients don’t get that therapy because of prior authorization, costs, etc.
So, let’s be honest. If I give the therapy that I think is the right choice for the patient, then I don’t know what happens.
And the reality is we have about 1/3 of patients not getting their therapy. Can you imagine what the patient thinks? ‘This healthcare professional gave me a medicine and he doesn’t even understand that I can’t afford it, or it’s not indicated or approved my insurance?’ And a lot of the time, the fact is they just don’t get the therapy—and we don’t know because we don’t follow up with them.
And so, I think there really needs to be an easier streamlined process for our patients at the end of the day.
Geralyn Warfield (host): (14:05)
Yes, that prior authorization process has put up a big roadblock for many of our patients and many of our providers. As you’ve discussed, it does take a lot of time to fill out that paperwork, be it that electronic or in person, whatever it takes.
So, I think helping patients also, though, find their voice and to be a partner with us in terms of helping to effect change is one of the strategies that I think PACH has encouraged us to use.
And I think it’s really valuable. Because I think when we work together, just like on therapies and treatments and patient outcomes, working together as a team with everyone involved, the more the merrier in this case, is my opinion.
Dharmesh Patel (guest): (14:36)
Well, thank you, Geralyn
Geralyn Warfield (host):
We are going to take a break and we will be right back.
Geralyn Warfield (host):
We’re back with Dr. Patel talking about access to medications and treatments. And Dr. Patel, I know you work in a very specific part of the country where maybe there are additional barriers that some of us, no matter where we work, might be facing as well. And I’m wondering if you could address those for us.
Dharmesh Patel (guest): (15:04)
Absolutely, Geralyn. And I work in both the states of Tennessee and Mississippi, some of the most obese, unhealthy states, unfortunately, in the country. And please remember, especially in Mississippi, we serve a very underserved, rural community, especially a lot of African American patients in particular in those areas.
I think that’s really important, because what we know is that healthcare access in certain parts of the country, like Mississippi, is immense in terms of barriers.
And you know that can be due to so many different factors including education, socioeconomic, literacy, housing even. And I think is very important.to appreciate that some of these patients have a different set of services than we truly think.
Some are living paycheck to paycheck. Some are not even sure where they’re going to be living next month. But I think it’s really important that we do bring advocacy to these areas because, unfortunately, these are areas where there has been no voice.
So, one of my personal missions has been to try to increase advocacy, and awareness, and access to care in “rural deserts” of Mississippi. And you know, I think our group in particular has really made a stance and gone to areas which are very, very underserved. And we have clinics there now. So, we’re very pleased to do that.
But what’s important is that even access and insurance companies, sometimes can be barriers to therapies for these patient populations. And we are working really hard to fight that.
You know it’s very sad to say that it’s a fact if you’re let’s say Afro-American, you’re 20 % less likely to be getting access to care, or certain therapies, if you in the Southeast states of the United States. Your likelihood of getting a prior authorization is 20 % less than other parts of the country, just simply on your race or where you live, which is just not acceptable.
So, you know I sometimes say the joke if you have cardiovascular disease, don’t live in Mississippi. Because it’s very, very difficult sometimes to get FDA-approved therapies to patients that need them.
So, we’re fighting for this cause every single day and I know that will make a difference.
Geralyn Warfield (host): (17:23)
Well, thank you so much for carrying the banner for us and leading us towards better access for all of our patients, no matter where we live.
Dharmesh Patel (guest): Thank you.
Geralyn Warfield (host): Thanks so very much for being here. This is Geralyn Warfield, your host, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. Visit PCNA.net for clinical resources, continuing education, and much more.
Topics
- Advocacy
- Health Equity
Published on
June 17, 2025
Listen on:
Related Resources