How do we effectively address the increasing strain on an already overwhelmed workforce? Guests Nikki Akparewa, RN, MSN/MPH, and Michelle Johnson, MD, MPH, describe how burnout, turnover, and early retirement are impacting healthcare professionals, and how training and education can lead to a better workplace.
This episode was recorded in partnership with Medical Alley and the Association of Black Cardiologists.
This podcast episode was supported by an independent educational grant from Novartis Pharmaceuticals Corporation and Pfizer Incorporated.
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield On today’s Heart to Heart podcast episode, we are excited to be partnering with Medical Alley to bring you the second part of this three part miniseries on health equity. If you like what you hear, follow Medical Alley podcast or visit MedicalAlleyPodcast.org
Frank Jaskulke Good afternoon and good evening to everyone out there in Medical Alley. Thank you for joining us on another episode of the Medical Alley podcast. This is your host, Frank Jaskulke, and we’re having another one of our [00:01:00] fantastic conversations as part of our partnership with the Association of Black Cardiologists and the Preventative Cardiovascular Nurses Association. This time on one of the most important topics, healthcare workforce and the topic of burnout and strain. I’m so pleased to be joined today by two fantastic guests who are going to share their perspective on the issue and some of the things we might do as a community and as an industry to better address these issues. Joining me today is Nikki Akparewa, who’s a nurse entrepreneur and Dr. Michelle Johnson who is the vice chair of health equity and a clinical director of cardiology at Memorial Sloan Kettering Cancer Center. Thank you both for joining me today. Nikki, I might start with you and Dr. Johnson, I’d appreciate your perspective as well. When we say burnout, what do we mean and how does it show up in the healthcare professions and contribute to turnover and other challenges?
Nikki Akparewa Yes, I think that’s an excellent question. [00:02:00] And again, just thank you so much for having me on the show today. My name is Nikki and I am a nurse. I’ve been a nurse for almost 20 years. And so when I think of burnout, I think of it as very personal, right? Not so much a scripted definition, but for me personally, burnout have been those experiences in which I have felt that I’ve given all that I could to the role and I did not feel that it was making me feel fulfilled as a nurse practicing whether bedside or in community or, you know, working as a case manager where you’re giving more than what you’re getting back. And burnout is endemic, unfortunately, in nursing, almost specifically, where we know that nursing, we experienced lots of instability, right? So nurses are really getting to a point now where burnout is not only on the rise, but it’s really taken front seat, as COVID has really amplified the impact of burnout for so many nurses. And [00:03:00] what nurses have been saying and have been trying to say for many years is that burnout makes them feel unsafe, right, to practice. It also happens in a way where they feel lack of validation and support from their management and peers. And that’s also coming from a lack of flexibility where these schedules that they have are really difficult or they may be required to stay over their shift when they work 12 hours, right? So this is where you’re starting to see persons who are experiencing burnout when they feel like that they have given everything that they can and they still don’t feel validated, safe, or have the capacity to care for themselves or their family in the way that they really need to.
Frank Jaskulke Oh, indeed. And thank you for sharing that it’s personal and individual, not just some route definition we might give. And Dr. Johnson, what about from your perspective?
Michelle Johnson Well, thanks again to our hosts and to Nikki for sharing in what I think is a very timely and very [00:04:00] important conversation. From the physician side, the clinician side, we, using a more technical definition, I guess, which includes some of what we just heard. Burnout is the syndrome which includes the emotional exhaustion that we highlighted in our first answer. It includes a loss of interest in work, feeling ineffective or having a sense of reduced personal accomplishment, which you just heard Nikki describe. And there is also an element of depersonalization that can go along with burnout. A tendency to see people as objects, rather than as humans. And you can imagine that any and all of these things could have negative impact on patient care. So, you know, really an important issue. Far higher rates in our physicians, colleagues, or [00:05:00] physician body post-COVID than pre-COVID, but continuing, even though the pandemics over the rates of burnout in the clinical physician community remain high.
Frank Jaskulke Right, and I want to dig more into that part of it, but where I might start in this first part of the discussion. If we go back to the clinical training, the education that doctors, that nurses, that other health care professionals are getting, are there things we could or should be doing at that level to better prepare health care professionals or to better manage the situation? I don’t want to minimize it, but maybe starting from that point, are there things we should be doing?
Nikki Akparewa So 1 thing I can say, and I think this is a really timely and important question is that what I experienced, at least for me, and I mean, I went to [00:06:00] nursing school almost 20 years ago, right? It wasn’t talked about at all. Burnout was not discussed in my education. It wasn’t discussed while I was trying to prepare and while I was training for the work that I was going to go into. So, I think for me, I experienced a really steep learning curve and I was really shocked to really have these experiences. My very first year at the bedside that I just almost felt like I was going to leave the profession.
I really felt a lot of instability, which is those, you know, those feelings where, or those behaviors that are, considered demeaning, rude and demoralizing. I had experiences where I saw other people that were not being treated the same way that I was being treated. And we can talk about that a little bit more later, you know, being a nurse of color as well and what that looks like. But for sure, burnout is not really effectively addressed in nursing education and to that end, one thing that I have [00:07:00] really done and really worked really hard as a nurse to model for my students because I’m a clinical instructor as well is to give them, you know, just to help them understand that this is the work that they’re going to be going into that it’s difficult. It’s challenging and to prepare yourself. Right? So you’re not walking into it just completely thinking that I’m here because I care. I’m here because I want to take care of people. All that is great. And that is very necessary and important and we really need that. And we want them to know that persons who are working at the bedside, many of them are just intentionally decreasing their work effort because they’re so exhausted. And, we have nurses that are saying, listen, you know, our seasoned nurses who have been there for years, 71 percent of nurses that have over 15 years of experience are leaving the profession, you know, as soon as possible. So when you have persons who are leaving the profession who are seasoned and [00:08:00] you have lots of newer people coming in who really don’t know this work. Burnout is really, really common. So one thing that I do is really talk to my students about what burnout is and how to prepare themselves and how to safeguard and when to walk away and how to advocate. I think all of that is really necessary, but I don’t think they’re getting it from every faculty member or clinical person. And so I think that’s something that we need to do better at as clinicians.
Frank Jaskulke That seems to be true in so many facets of life that while it is not the be all end all, it is often a starting point of acknowledging and talking about the reality of a situation and the problems that are out there. Dr.
Johnson, what about from the physician’s side and education and training?
Michelle Johnson So I agree with what’s been said. I would highlight too that it is of shared responsibility and while we, of course, want to look at strategies [00:09:00] and behaviors and techniques that we can equip our young trainees with, that this is a responsibility also of institutions and training programs and the medical profession as a whole. The burden and responsibility doesn’t lie solely on the trainees. So, to echo what’s been said before, there is a paucity really of information. We don’t have a lot of evidence-based approaches to understand techniques and how to mitigate burnout and as has been said before including these strategies or what is known in training programs is relatively new. Techniques are putting in place programs that will ensure med student wellbeing is important. Making sure that there are adequate services for students who identify as being in burnout or in distress, optimizing learning [00:10:00] environments, looking at curriculum, grading, how the day is structured, all of those types of things, providing, support, making students feel a sense of belonging, not feeling isolated, all these things help to mitigate burnout. And there’s certainly space for more of this to be done in medical education and support.
Frank Jaskulke Yeah. And you, you started going this direction a little bit at your mention of the institutional responsibility as well. What about on the management side, like setting aside the educational piece, you have, you’ve both illuminated a handful of the challenges that exist in healthcare at the bedside today. Dr. Johnson, I might ask you to start and then Nikki, following with you, what about the, the management or the administrative side? Are there things that healthcare organizations can do, should do, are doing to create a better environment where the, the burnout is reduced or where it’s better managed if it can’t be [00:11:00] reduced?
Michelle Johnson So I think there’s certainly opportunity to decrease burnout. And I would highlight that physicians are known to have high levels of individual resilience, so the techniques to decrease burnout are not going to be effective if all we look at is individual resilience on the part of our clinician workforce. So, I’ll give you some examples of things that cause burnout. We’ve already mentioned instability and institutions can set the tone for what behaviors will and will not be accepted in their clinical environments. We know that having the electronic health record, transitions to bureaucratic tasks, all of these things add to burnout. And making sure that we are asking our clinicians to [00:12:00] be efficient and providing them with best tools to do so. Support staff, you know, manageable work schedules. We’ve already talked about, making sure that people feel respected, both from their peers and from the patients who they treat all of those things are institutional mandates that can have positive impact on efforts to mitigate burnout.
Frank Jaskulke Indeed, and Nikki, I’d ask for your perspective as well. And you mentioned a couple of minutes ago that there can be also different challenges for nurses, clinicians, providers of color. Could you maybe expand upon that as well?
Nikki Akparewa Yeah, sure. So, one example that I’ll share with you that really stuck out to me when I was going through my training initially was, I remember having a peer colleague of mine, another nurse of color that started with me, and she was in her orientation. She left a bed up a little bit too high while she was [00:13:00] trying to learn how to do her job, right? This is when in the first couple of months and they pulled her into the office, told her they wanted to extend her orientation, offered to send her to another unit to work somewhere else. Okay. She did not feel comfortable with the approach that they took to that process. Meanwhile, a peer who, a white nurse, who walked out of a patient’s room, told the patient to do their own hibicleanse, the patient you know, takes all of their monitoring devices off. We didn’t even realize, you know, that the patient was off the monitor. Someone comes in the room, finds this patient has actually passed away. And this nurse was cross trained to our ICU, which is a coveted thing, right? So when I saw this kind of interaction happen, I, and some things happened to me as well, but that was stark for me to watch how one nurse of color left a bet up and was said, was told, hey, you can go somewhere [00:14:00] else to work. Another nurse who was partially at least, you know, sort of responsible for this patient’s demise was offered a promotion to the ICU. So, many things happened in my career along the way where I did not feel like I had enough psychological safety, right? Which is that believe that I’m safe to take risks and a personal risk-taking other types of risk taking. So, psychological safety is a huge, huge factor I want to say for promoting civil behaviors in the nursing profession and making sure that we’re creating environments where equity really is present and persons are not coming into work, feeling like you will treat someone else, you know, very differently than you treat me because of the perceptions that you may have about people of color and what you expect them to be able to do or not be able to do.
And so while we’re battling, you know, burnout and, all [00:15:00] of these different things, you know, nurses of color report higher, much higher levels of burnout and emotional lack of safety than their white counterpart nurses and so being mindful of how we create our environments, right? Just for everyone, how we create inclusive spaces, how we, what I like to call coaching culture or create places where persons can come in and they can feel like they can express themselves and they can, you know, say things without fear of retaliation, I think is really, really significant. And I wanted to also point out, you know, because I’m a huge advocate for coaching and that really is just creating space for people to be motivated to do their best work. The Cleveland clinic did a really, really excellent process on promoting coaching culture with their physicians, where they were actually able to help the health system avoid 84 million dollars in physician turnover costs over the past decade by [00:16:00] allowing physicians to coach each other. Right? And Dr. Johnson mentioned the resiliency with physicians. I would say the same is true in nursing. I don’t think we have been offered this opportunity in nursing, but what this example shows is that we can save money by, you know, allowing peers to coach each other to support each other. It also helped them with increased leadership. So there’s a lot of value in really promoting a culture and organizations that says, yes, you do belong. We do believe in what you have to say. We want to hear what you offer. All of those things are really necessary and vital, I think, in contributing to the sense of safety and validation for people in our healthcare professions.
Frank Jaskulke You know, you both have talked about the tone, culture, the organization set up and the environment it creates. And I think for the listeners, I would really highlight that of the ability of an [00:17:00] organization to create an environment that is or is not conducive to healthy behaviors, healthy activities, healthy lives. Including for its workforce. So I appreciate you both really highlighting that area. Maybe Dr. Johnson coming back to you for a moment. Are there differences that you’ve observed among the specialties even? Do we see burnout breaking down differently among the different specialties that are out there? Or do you have any perspective on that?
Michelle Johnson Yes, we have data on that and it’s I guess consistently what you would intuitively expect. So those specialties that practice on the front lines have higher rates of burnout and indeed over the past, you know, since the pandemic during a pandemic have seen increases, disproportionate increases. So emergency room physicians, internal medicine, [00:18:00] OBGYN, family medicine, those people who are already on the front line have had higher reported rates of burnout. And these are also practices where people report a higher, you know, lack of autonomy, which tends to drive higher levels of burnout. And we see in a converse, we see that people who are in solo practices, office based solo practices, tend to have less burnout reported in the surveys that have been done. And then in terms of what data exists on physicians of color. I would say there’s limited data and there’s a definite need for more research in this area to understand the unique experiences of physicians of color.
What exists, we have seen that, as we’ve heard from our nursing colleagues, not feeling valued at work [00:19:00] contributes to physician burnout. Feeling that you have low advancement compared to your peers. Perceived racial or ethnic barriers to advance and all of these things add to physician burnout. And so when we talk about institutional measures to try to mitigate what is a very expensive thing, I mean, replacing workforces. You know, again, as has been said, it costs a lot of time and also a lot of financial resources. It’s much more efficient to keep your already trained force. And so making sure that you have an equitable system, that you have transparency in how it is people are hired, how people get promoted, how people are compensated, all of these things are very important so that everybody can feel that you’re being treated in the same way to, you know, to decrease the chances of burnout and people leaving.
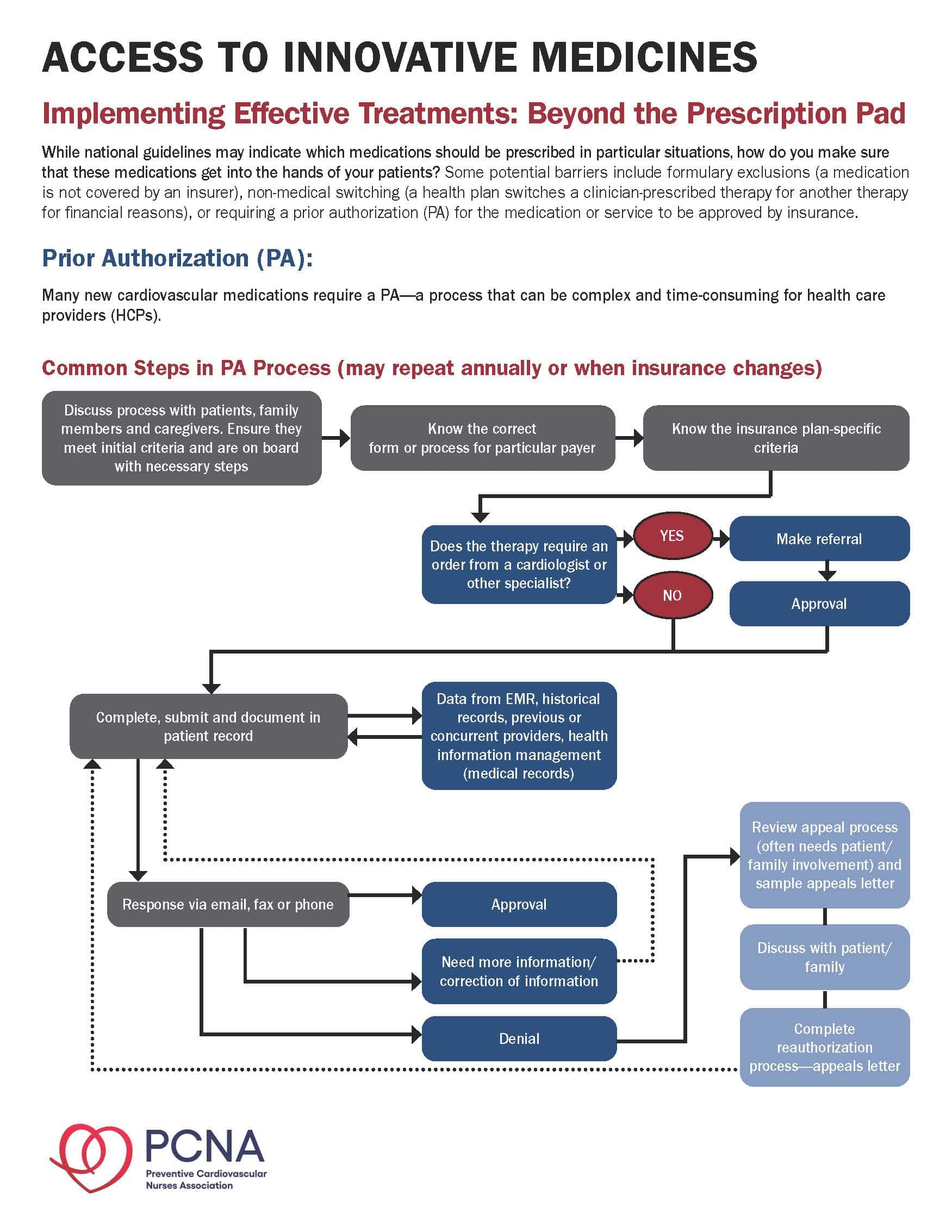
Frank Jaskulke Well, maybe related to some of that, [00:20:00] what about some of the tools that have been in place? You mentioned health record systems earlier, but I think of things like, prior authorization and step therapy and other systems that are in place where seemingly the intent is to manage better or provide better care. Do those contribute in any way to some of the challenges that you’re observing?
Michelle Johnson They do and I would like to, you know, congratulate those groups who have been instrumental in trying to get changes in some of these areas such as prior authorization. Most recent changes that the plan is to have at least for procedures, prior authorization done on a computer-based way rather than, you know, a series of phone calls and a phone tag, you know, which is just very time sink. The electronic medical record certainly has many advantages but understanding that [00:21:00] having a clinician spending more time on the computer than on a face to face encounter with a patient might not be what it is we desire. Seeing how it is, you know, perhaps AI and scribes can help decrease some of the burden that physicians feel from documentation and bureaucratic type of responsibilities would also be helpful.
Frank Jaskulke Indeed. And, you know, I think another big topic that’s been out there, we talked a little bit about education and training at the beginning, but there was a recent, you know, very significant Supreme Court case effectively eliminating affirmative action in higher education. Maybe Nikki, I’d start with you and ask, what’s your perspective on the potential impact of this case on building and growing a diverse workforce in health care? And then, Dr. Johnson, I’d ask you the same.
Nikki Akparewa Yeah, that’s an excellent question. And it’s interesting that you asked that [00:22:00] because I’m actually going to be starting in, you know, full time academia. I actually posted the same question to the National League for Nurses, just to kind of get a sense of like, what do they think? Because, you know, I’m kind of new to this process and, you know, the responses are really varied. I think part of the biggest challenge with this is that people don’t know enough about what affirmative action is. You know, has really done. And myself included, right? I’m not a politician. I don’t, you know, go looking for what that all means in each and every interaction, but what I can tell you is that with the, you know, the academics, the leaders that I have spoken with, they’ve mentioned something called the chilling effect, and I don’t know if, you know, that’s a familiar term, but essentially the chilling effect is when persons don’t really know what they can and cannot teach. Or how, you know, they can talk about real life things like how race has [00:23:00] impacted us, historically. When people don’t know how to do that, it really makes it more difficult for them to want to teach those things. And then also, when you’re really thinking about academics, it forces you to be really, really intentional. Right? Around maybe we cannot really consider race in terms of admissions, but what are the other factors that we can consider? And if you’re working at an institution where they’re not wanting to take those types of things into consideration. It’s going to pose a barrier, right? It’s going to make it more difficult for persons who would like to pursue school or pursue advanced, training to really feel like they can safely and comfortably do that. And it makes it more challenging for academic, leaders to think through what is it that we can and cannot do. So I, my belief is, that this is going to be a [00:24:00] challenge that we’re all going to have to face. I know for nursing, we’ve been doing a lot of work around health equity and our standards, our AACN, our credentialing body, the way we’re trying to standardize health equity. So I’m interested to see what ways in which, you know, our credentialing body is going to really navigate this terrain. It’s all really new. I know that for our standards, we’ve really been pushing health equity. So my hope is that there’s going to be some guidance to all of our academic institutions as to what are some ways that we can navigate this new terrain, because I think a lot of people are gonna not really know what the next step is. My hope is that we would continue to create open, honest dialogue with our, between our students, with our faculty, with our clinical partners, so that we’re all thinking together, right? The worst thing I think we can do is get into these silo [00:25:00] behaviors where we think we have to create these, you know, these processes independently. We don’t have to do that. We can collaborate one with another and we can learn together so that we can truly support each other. But I do think this is going to be a challenge. I do think it’s going to be significant. And I do think we’re going to have to work together to get through it.
Frank Jaskulke Thank you. And Dr. Johnson, your perspective.
Michelle Johnson So we have plenty of documentation in literature that diverse teams are more productive. They ask different clinical questions, they ask different research questions, and this is true in the medical arena. It’s also true in a non-medical arena and the affirmative action allowed us to have more diverse students at tertiary institutions or institutions of higher learning. So, without question, this is going to make it more challenging to have diverse representation, not only in [00:26:00] medicine, but across the board. And so healthcare industry, as well as other industries are going to have to be creative about how it is they maintain or create diversity when they’re not ensured that those people will be in the schools, in institutions of higher learning. There are discussions about looking at economic diversity as a way of making sure that we have representation from across socioeconomic strata. There are discussions about looking at seeing, you know, colleges will admit the top 10 percent from local schools, as ways of trying to be sure that we’ve reached all students, all talented students. Recognizing that not everyone has the same opportunities if they’re coming from schools that are not as well resourced. If [00:27:00] they do not have an opportunity to have coaching, private coaches, SAT classes, you know, and all the rest of it. So we have a heavy lift to have ahead of us and it’s not unique to health care. Certainly it will be something, a challenge that we have to take on. And we can see, you know, states where affirmative action had been struck down before and the numbers of diverse medical students suffered.
Frank Jaskulke A heavy lift indeed. And I think that might be the right spot to wrap up this part of the discussion. And so I want to say, thank you to both of you for sharing your perspectives, sharing your insights and stories and helping us advance this conversation today.
Nikki Akparewa Thanks for having me.
Michelle Johnson Thanks very much for the opportunity. It’s really a timely discussion and yeah, I’m sure everyone would appreciate it.
Frank Jaskulke And [00:28:00] folks, a very timely and very important discussion. Certainly. And one I hope will continue a couple more times. That’s been another episode of the Medical Alley Podcast. If you’re not already a subscriber, make sure you get over to MedicalAlleyPodcast.org or you can find us on Apple, Spotify, or wherever you go for your podcasts. And would you do me a favor, would you share this episode with at least two other people? I know I normally ask for one, but this is a really important topic. So share it with at least two other people. Help spread this story and this information so that more people will hear it and understand. If you do that, I’d really appreciate it.
Until next time, have a great day.
Thank you for listening to Heart to Heart Nurses. [00:29:00] We invite you to visit PCNA. net for clinical resources, continuing education, and much more.
Topics
- Health Equity
Published on
September 19, 2023
Listen on:

MD, MPH

RN, MSN, MPH
Related Resources