In a perfect world, everyone would have regular connections with a health care team to focus on disease prevention and management. In reality, a variety of barriers keep people from primary and preventive care, leading many to seek attention only when they are in crisis, straining emergency departments and urgent care settings.
While multiple solutions are needed to address the challenge of access to equitable care and the goal of reducing risk for cardiovascular disease (CVD), stroke, and other acute and chronic health issues, in just about every location, healthcare professionals can meet individuals where they are, such as at local screening events. These community considerations for cardiovascular care can help alleviate the gap faced by many individuals and help identify those with acute needs who require rapid referral to avoid devastating consequences.
Best Practices in Community Screenings
Community screenings are one way to address the need to identify individual risk for, or presence of, CVD. Either on their own or in association with larger events such as heart walks or community festivals, community screenings make it easy for individuals to be screened for CVD risk factors (e.g., hypertension, diabetes, hypercholesterolemia, etc.), or even disease identification (e.g., AFib, peripheral artery disease, etc.).
Screening events are a lifeline and a bridge between individuals who may be at risk, have undiagnosed issues, and have no or limited access to care. The goal is typically to increase awareness, provide a real-time assessment of health measures, empower individuals to continue to improve their health, and—when warranted—connect people to immediate care.
Community outreach spans a wide range of locations, services, and timelines. This article will focus on two specific outreach efforts, and the commonalities in effective planning and implementation of community screening events.
Baltimore, MD
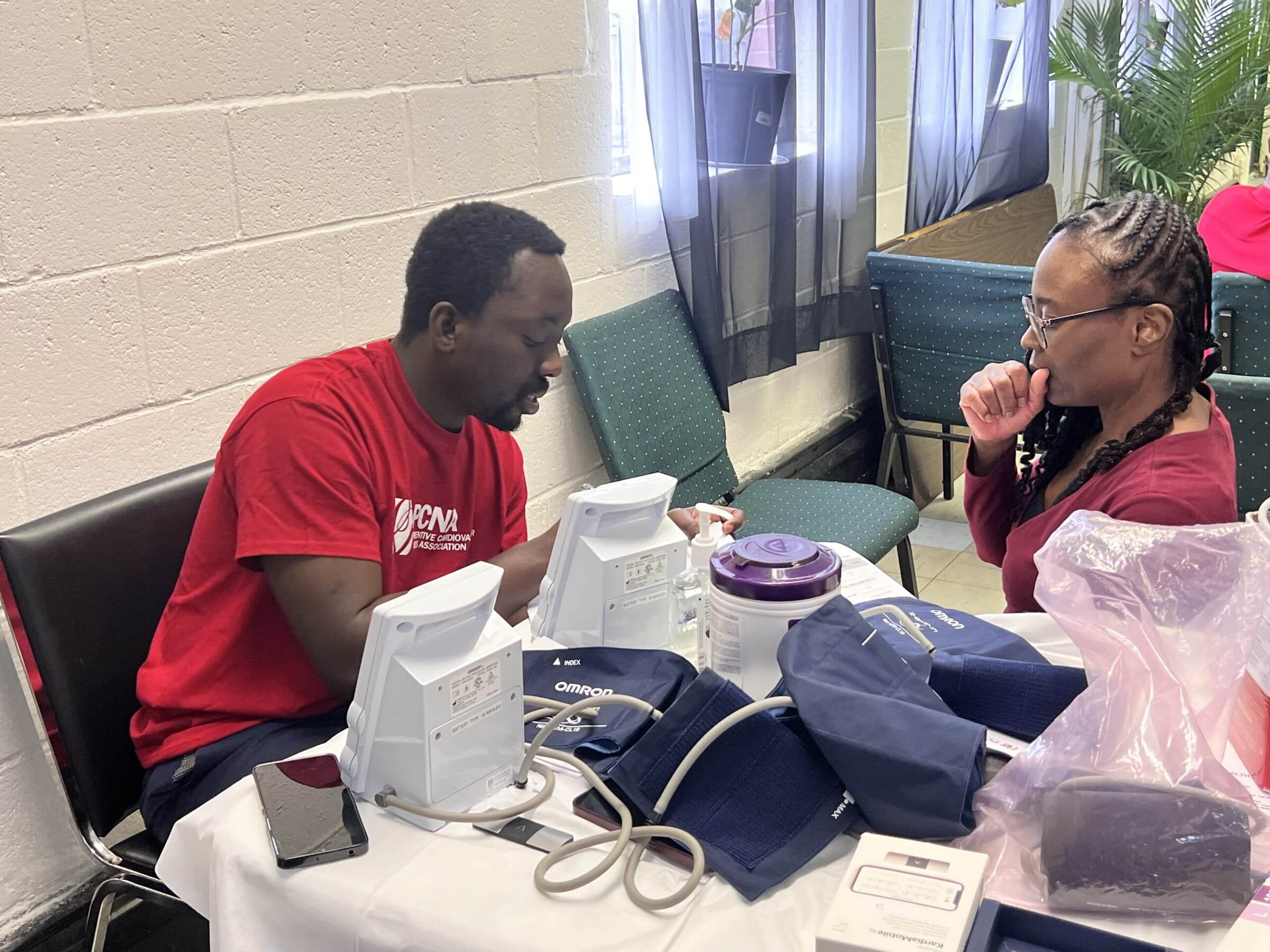
The Baltimore area chapter of the Preventive Cardiovascular Nurses Association recently completed a multi-year research project to identify best practices for community screening events, with a focus on hypertension and atrial fibrillation (AFib), which are both major contributors to CVD morbidity and mortality. The study team focused their recruitment efforts on Black adults aged 35 and older. 
Using a 12-month timeframe, the initiative was designed to address cardiovascular health disparities among Black residents in Baltimore City through targeted screenings and associated follow-up interventions. The team was not only interested in providing outreach screening for community members, but in identifying best practices and developing an effective, standardized approach to community-based education that could be replicated elsewhere.
In partnership with community centers and faith communities across Baltimore City, screening dates were carefully scheduled to maximize accessibility for working community members. Events were promoted through posted flyers and community announcements. At each event, the study team spent about 15 minutes with each individual assessing hypertension and AFib risk and providing each participant with a ‘report card’ documenting their screening results to share with healthcare professionals.
With participant consent, the study team followed up within 2 weeks of the event to assess whether or not the individual had connected with healthcare professionals. Subsequent quarterly phone check-ins, each lasting 10 minutes, continued for 12 months. Beyond data collection, the calls allowed team members to identify and address barriers to care, as well as maintain engagement with screening event participants.
You can find a full report, Community-Engaged Research for Cardiovascular Nurses, which included recommendations for effective screening events.
Southwest, GA
Each June, more than 120 faculty, alumni, and undergraduate and graduate student volunteers from Emory University’s Nell Hodgson Woodruff School of Nursing and other academic partners spend 2 weeks delivering vital health care to farm workers and their families in a farming community in southwest GA.

Each day, the students deliver preventive care, such as screenings and well-child physicals. Now in its 32nd year, the community outreach program reaches over 1,200 individuals at the height of the growing season. The temporary workers, hired by local farms in accordance with federal visa and wage requirements, often have no health insurance and are among the poorest of all workers in the country.
In addition to screenings for CVD-related diseases such as hypertension and diabetes as well as other disease states, participants receive care for work-related injuries, receive information on how to reduce conditions such as back strain by using proper lifting techniques, and even details about staying hydrated, sun and insect protects, and much more.
Unique perspectives for the students include working in the heat and humidity, providing team-focused care with an interprofessional health care delivery model, and providing care at the local clinic, night camp, and area elementary school.
Find more details about the Farm Worker Family Health Program project.
Common Themes and Key Takeaways
1. Forging and maintaining long-term relationships
Key to the success of both outreach programs is the engagement of nurses and other healthcare professionals in building trust and nurturing meaningful relationships with community members. It is important to recognize that this is a long-term connection and is not completed through a ‘helicopter’ model of dropping in for a quick event and then leaving. It is accomplished through a continuous, collaborative effort that ensures that interventions are sensitive, accessible, and impactful. This commitment ensures that community members are respected and engaged.
2. The importance of planning, and the ability to pivot
Just as in clinical settings, planning for community outreach ensures adequate staffing and supplies to meet the anticipated need. And, just as in the clinic, it is important to plan for the unexpected, such as a participant who needs to get to the hospital due to an acute crisis. Three examples include considering ‘What if…?’ situations as event planning progresses, identifying in advance the support and resources that are available, and helping screening participants access these resources if needed.
3. Knowing your audience
If your team will be working with individuals with mobility issues, plan ahead to ensure that your event is set up for success. A location that is easy to find and navigate around can go a long way to making participants feel comfortable, whether or not they have mobility issues. If you anticipate possibly working with participants with language barriers, the use of in-person or virtual translation services will help those in attendance to effectively understand the screenings, results, and proposed next steps.
5. Providing nonjudgmental care
It is important for staff and volunteers who plan, implement, and follow-up community health screenings to recognize that participants may have a long-standing fear of health care, lack of experience with providers, or other barriers that may make them uncomfortable during the outreach encounter. Some ways to improve the encounter include an extra dose of patience, more time spent in getting to know the individual before diving right into questions and diagnostics, and ensuring that information is shared in a non-judgmental manner and in a language that is comfortable for attendees.
Healthcare professionals involved in outreach events should be mindful that some participants may not have any other opportunity to receive health care throughout the year, and to be on the lookout for any ‘red flags’ that might require immediate intervention.
Recognize that participants may not be able to follow ‘traditional’ advice such as regularly accessing and eating healthy foods, staying active, etc. Work to identify ways that participants can take small steps towards better health to help them leave the event with a more positive outlook on what is next.
6. Empowering participants to continue their relationship with the healthcare community
Providing details about what took place during the screening, and suggested next steps and related resources, can help participants know what next steps to follow. A list of no-cost or affordable clinics with hours that extend beyond the usual workday, for example, may benefit those who worry about lost wages with a trip to an emergency room or clinic that includes time away from work. Take-home educational materials can reinforce the information shared during the outreach event and provide an opportunity for attendees to share information with their family members or caregivers to support needed next steps.
Resources for Success
Published on
July 1, 2025

PhD, MPH, RN, CDCES, FAHA, FPCNA, FAAN
Related Resources
Sorry, we couldn't find any resources.