While Lp(a) levels are generally hereditary in nature, other factors can cause elevated levels. Learn about current guidelines-directed medical therapies, and how guests Lisa Maher, DNP, ARNP, FNP-BC, FPCNA, and Kathy Byrne, MSN, CRNP, CCRN apply these guidelines to clinical practice.
Earn 0.5 contact hours and .01 pharmacology hours from listening to the podcast episode and completing the course components.
Episode Resources
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Welcome to today’s episode, the second of a three-episode miniseries on lipoprotein (a), also known as Lp(a). We encourage you to listen in to our first episode about prevalence and testing, and also to the third episode, which covers the impacts of Lp(a) on the body and CVD risk, clinical trials, and research.
This episode is available for CE contact hours. Please be sure to follow the link in the episode show notes to complete the post-test and access your CE certificate. To help us learn more about this topic, we’re talking today with Lisa Maher and Kathy Byrne. Lisa, could you please introduce yourself?
Lisa Maher (guest): Hi and thanks, Geralyn. I’m very excited to work on [00:01:00] part of this podcast on Lp(a). I’m a Nurse Practitioner with Unity Point Clinics and work at the Unity Point Health Allen Hospital Cardiovascular Center, located in Waterloo, Iowa. I am the current President-elect of PCNA and also a chapter leader of the Cedar Valley, Iowa Chapter.
I work in a general cardiology setting, treating patients of all ages with cardiovascular disease. Along with this, I also manage a specialized sleep clinic in which I work with patients with underlying cardiovascular risk factors or cardiac disease, who also have sleep, distorted breathing or sleep apnea.
In addition to treating cardiovascular patients and sleep patients, I also enjoy preventative care and have previously managed a lifestyle medicine clinic. Thanks for having me.
Geralyn Warfield (host): We’re glad to have you here. And we’re also glad to have Kathy Byrne with us. Kathy, could you introduce yourself?
Kathy Byrne (guest): Thanks, Geralyn, for the opportunity that’s afforded, been afforded me by the PCNA to participate in this very [00:02:00] important podcast.
I too am a Nurse Practitioner in both Adult and Pediatric Cardiology at the Johns Hopkins Medical Institutions in Baltimore, Maryland. There I care for adults with congenital heart disease, as well as all age groups ranging from the cradle to the grave in those with lipid disorders, I also serve as a research coordinator for ongoing studies.
Geralyn Warfield (host): We are so grateful to you both for sharing your time and expertise with us on today’s episode. Kathy, could you get us started talking a little bit about what the factors are that increase Lp(a)?
Kathy Byrne (guest): Well, to be clear, Lp(a) is almost entirely genetically determined and it’s through an autosomal, co-dominant mode of inheritance. This Lp(a) gene is fully expressed by one to two years of age, and the concentration of Lp(a) reaches adult levels by about five years of age.
In the absence of inflammation, [00:03:00] plasma Lp(a) levels are relatively consistent, but with acute illness, they may increase.
Now let’s just go back and reflect on some of the non-genetic factors that may impact Lp(a), First of all, chronic kidney disease, specifically in those individuals who have decreased glomerular filtration rates and severe proteinuria, such as those who have Nephrotic Syndrome.
We also see that Lp(a) levels increase throughout a normal pregnancy. Actually, there’s a doubling of the median value, and we see greater increases as gestation increases as well.
There are also several endocrine conditions that can impact Lp(a). Polycystic ovarian syndrome, hypothyroidism, human growth hormone, Cushing’s disease—although it’s a [00:04:00] little, it’s a little bit debated because in one study it showed that there was an increase in Lp(a) and in another, a decrease. Also, androgen deprivation therapy.
There’s a trend towards higher, a higher incidence of clinically significant Lp(a) in men with low testosterone levels. And also, we see, when there’s been an orchiectomy, or treatment with gonadotropin releasing hormone.
And then, finally, in acute myocardial infarction, be it STEMI or non-STEMI, we see an increase in that Lp(a), and it tends to increase further in the six months following an infarction.
Geralyn Warfield (host): Kathy, that was a very comprehensive list of things that can affect the levels of Lp(a) in our bodies. [00:05:00] Lisa, are there any other factors that can affect those levels?
Lisa Maher (guest): Yeah, there are, and Kathy did a great job touching on so many different topics, but a couple more would be age, acute illness and sex differences.
So, when we talk about Lp(a), Kathy has mentioned earlier that they’re established early in childhood and remain relatively constant throughout life. But again, it should be noted that there is some controversy as far as when at what age children should be screened.
So, Lp(a) should also be obtained in the absence of an acute illness. So, Lp(a) levels may be elevated as an acute phase reactant. And also too, there are notable differences in sex, in that plasma Lp(a) concentration levels remain relatively constant throughout life in men. And with women, they tend to increase after menopause.
Geralyn Warfield (host): Well, I really appreciate that comprehensive [00:06:00] overview of how Lp(a) stays relatively constant in our lives, but can increase due to that inflammation or other factors. And we obviously cannot control necessarily the levels that we get genetically in our bodies.
But as healthcare professionals, how do you deal with individuals that you are working with in the clinic that have elevated levels of Lp(a)?
Lisa Maher (guest): That’s a great question, Geralyn. So, when I try to think of Lp(a), I try in my head to separate those groups. So, there are two main subgroups that I want to talk about. And first, it’s those that were thinking about primary prevention, so those without any atherosclerotic coronary vascular disease.
And then the second group would be those with ASCVD risk, or secondary prevention.
So, in the presence of elevated Lp(a), treatment of both groups should be focused on optimal control of those modifiable risk factors. We definitely want to [00:07:00] talk about education directed at smoking cessation, nutrition and diet counseling, as well as exercise counseling. And we should, in our practice, especially if we’re treating cardiovascular patients, be focused at providing that education to all.
So, when we talk about primary prevention, it’s essential to attain the following key elements of a routine assessment:
- So, we want to do a thorough review of the individualized risk factors.
- We want to calculate that ASCVD risk with the equation.
- And we want to assess any family history of any early atherosclerotic cardiovascular disease.
Sometimes if you phrase it that way, if you say, and I have found out too, if you just say, “Hey, do you have any family history of any coronary disease?” You know, they sit there and they think, or sometimes they will really know. But then I get into more specific, “Do you have any family members who have had a history of a heart attack, or do you have any family members who have had a history of stents, or [00:08:00] coronary bypass?” And then they understand and then you usually get a lot more from them at that point.
So, if those risk factors are present, and the calculated ASCVD risk is considered either borderline or higher—so greater than or equal to 5% in that 10 years according to the pooled risk equations—or if there is family history of early ASCVD or familiar hypercholesterolemia, then elevated lipoprotein (a) should be considered a risk enhancer. And then treatment should ultimately focus on risk factor modification, specifically LDL-lowering.
So, even with optimal control of risk factors, and those not considered to be high risk, subclinical aortic atherosclerosis might be present. So, when we think of this or when we have suspicion for this, it may be helpful to use the [00:09:00] coronary artery calcification, or CAC, score.
And this can provide a reclassification of that low risk to intermediate- or high-risk. So basically, that’s saying that if you have a patient who has elevated lipoprotein (a), and you are kind of on the borderline as far as do you treat them or not, getting that CAC score can help you determine how aggressive you want to be with that.
Then switching gears and talking about secondary prevention—so remember, those are patients who have identified ASCVD—there is evidence that even with the use of statin and antiplatelet therapies, the risk recurrence of events are increased by having high, or elevated, lipoprotein (a).
So, management of those patients should focus on intensifying those LDL-lowering. And then the higher risk of events in those with high lipoprotein (a) [00:10:00] was associated with a greater absolute benefit of further LDL-lowering with PCSK9 inhibitors.
Kathy Byrne (guest): Lisa, thank you so much. Those are very key points, and I have to say, that’s the way I practice as well, really focusing in, honing in, on primary prevention and then on secondary prevention.
And I think we need to keep this in the forefront of our minds as practitioners when we look at folks who, have particularly, very high family, very high incidents of coronary disease within their families, or aortic stenosis, as well as recurring disease. So very key points.
I want to discuss a little bit some of the medical therapies for increased Lp(a).
And you mentioned PCSK9 inhibitors, and I’ll go back and just reflect on that in a couple of [00:11:00] seconds. But I want to say that currently we really don’t have direct evidence from randomized clinical trials that lowering Lp(a) reduces risk for cardiovascular disease. But stay tuned. Okay?
But we do know that conventional lipid-lowering therapies do not lower Lp(a) to the extent observed for LDL cholesterol. That does not mean that we still don’t treat, and treat aggressively. And statins generally don’t have an effect on Lp(a) lowering. And in fact, some studies have suggested an increase in Lp(a) levels with those seen on statins. However, never fear, a review and meta-analysis suggests that the changes in Lp(a) in response to statins are not significant. So, we needn’t have a fear of using the [00:12:00] statins.
And then, back to the PCSK9 inhibitors. We have found that they reduce Lp(a) by 20 to 30%. And of course, we know that they can lower LDL cholesterol levels by up to 70%.
And in the two major studies we have found that, in the ODYSSEY outcome studies and in FOURIER, we have found that there was decreased cardiovascular risk, independent of the LDL reduction.
But how do those, what is the mechanism, I should say, of how, Lp(a) is lowered? We’re not, we’re not certain at this point.
Other medical therapies: mipomersen, which is an antisense oligonucleotide that lowers Lp(a) and FH patients by 21 to 30%. However, that is no longer available as a treatment in the [00:13:00] United States for us.
And then, lomitapide is an MTP inhibitor and in one report it was shown that it lowers Lp(a) by 19%. However, lomitapide can be associated with liver enzyme elevation and hepatic steatosis. And so, that may be difficult for some individuals to tolerate.
And then finally, I want to mention niacin, because that tends to have a dose-dependent effect on Lp(a), lowering it up to 20 to 40%. However, in studies, particularly in AIM-HIGH and the HPS2-THRIVE studies, they have not been associated with reduced cardiovascular risk. And so, we do not use them for Lp(a)-lowering.
And a lot of patients come into the office and they are certainly [00:14:00] geared up and ask specifically about, “Can we put me on niacin?”
A couple other things that I do want to mention, and that would be post-menopausal estrogen replacement. This is not recommended. okay. Not recommended. However, it does decrease Lp(a) and cardiovascular disease in combination with estrogen and progesterone—progestin, I should say—versus a placebo.
And then LDL apheresis. Now that is a, a treatment that lowers Lp(a) by 60 to 80% with each treatment.
And over the long haul, we find that there’s an overall decrease by about 25 to 40%. And that’s because—why the discrepancies?—and that’s because those Lp(a) levels rebound right after a treatment has been completed.
It’s the [00:15:00] only effective treatment that we currently have, and it’s the only treatment that’s been approved by the FDA for individuals who have increased Lp(a) along with ASCVD and LDL cholesterol levels greater than 100 mg/dL. They also say that the Lp(a) should be greater than 60 mg/dL. And remember, that’s a mass measurement.
So, you can, I’ve gotten LDL apheresis approved for individuals who have had their Lp(a)s measured with, nmols.
The downside of LDL apheresis is that it’s expensive. It is time consuming, and finally it’s not widely available. There are only about 60 to 70 treatment centers across the United States.
Our [00:16:00] biggest therapies that are on the horizon are the antisense oligonucleotides that target the Lp(a) messenger RNA, as well as short interfering RNA therapies. They target hepatic Apo A production. And that results in an Lp(a) decrease from about 60 to 90%/
Administration of these therapies have shown that there have been minimal side effects, and trials are in progress. Stay tuned because you’re going to be hearing much more about this in our third podcast on Lp(a).
And what about low, low dose aspirin? It does decrease risk in patients with ASCVD, and in primary prevention. And in the ESPRIT trial—the sub-study of the ESPRIT trial—those individuals [00:17:00] who were treated with low dose aspirin, and were carriers of an Lp(a) polymorphism, had a six, had a 46%, excuse me, 46% relative risk reduction for the combined endpoint of MACE.
So, lots of treatments out there. However, the only one that has been proven at the moment would be LDL apheresis. And then stay tuned for those small molecule RNAs, interfering RNAs.
Geralyn Warfield (host): Thank you both so very much for that comprehensive view of what Lp(a) looks like in terms of studies that are out there and how we might be looking to treat Lp(a) that is elevated.
We’re going to take a quick break and we will be right back.
Geralyn Warfield (host): We’re back with Kathy Byrne and Lisa Maher discussing Lp(a). And we’ve talked a little bit about treatments. We’ve talked a little bit [00:18:00] about what that looks like in clinical practice, but I’m hoping we could actually focus a little bit on what that might look like for a particular patient in terms of a case study.
Lisa Maher (guest): Sure, I’ll start with that. So, actually, I have a patient who I just started seeing within the last six months. Her name is Nicolette and, she came to me actually having her, lipoprotein (a) already drawn. So her lipoprotein (a) was elevated at 266 nmol/L.
So, her main complaint is of concern that she now has this elevated lipoprotein (a) level and kind of what to do with it.
So, looking back at her history, she has tried and has been unsuccessful with numerous statin therapies, and her main complaint with those, was myalgias. So, she recently had luck trialing and, and we recently started an older statin, and she has [00:19:00] been doing well on that since she started. just within the last couple of months.
She also recently started a cholesterol absorption inhibitor and she actually just got approved for a PCSK9 inhibitor. So, I’m very excited about that.
To risk stratify her more, because she does not have any known coronary artery disease—and really, her only risk factors were hypertension, her elevated lipids, and then this elevated, lipoprotein (a)—I did draw a CAC score. Her CAC score was greater than 100.
And again, she has not had any previous documented coronary artery disease.
I continue to follow her routinely, secondary to her concern, with her risk factors. And, with that elevated lipoprotein (a), I have recommended cascade screening in her [00:20:00] family members. Now when talking to the patient, her mother and father have both passed away, but I did recommend cascade screening in her siblings and also in her children. She has not, to my knowledge, nobody has completed that yet, so I am unaware of that.
When talking with her too, about her family history, there are no significant events of any cardiovascular disease at an age of 50 or less.
But she is definitely one who calls my office a lot. I see her a lot. I provide a lot of reassurance to her. And she is someone who I am looking forward and watching the trials very closely to see what is coming down the pipeline.
So, with her, again, I do a lot of counseling. in this case, I don’t know that I really offer a lot more except, you [00:21:00] know, routinely watch and check her, her baseline lipids, her blood pressure, and, and keep her risk factors under control.
I also talk to her extensively about her diet. I sent her to a dietician. Then we talk about exercise each time she comes in. So, we, we try to touch base on, I feel like I’m having the repeated conversation with her each time, but, usually she leaves the visit at least calmed down a little bit.
And then, again, I just see her routinely and really it’s for her request.when I see her back. She usually likes to see me about once a month. So, I’ve gotten to know a lot about her and we’ve developed a great relationship. And again, I’m just looking forward to treatment of her Lp(a) in the near future.
Kathy Byrne (guest): Oh, wow, Lisa. You know, I have to say that that’s the type of patient that we see also in our clinic. And it’s, frequent, okay, because I think the patients do [00:22:00] need reassurance because we don’t have established therapies for them other than LDL apheresis.
But if they are plugged into our clinics, once the results of the studies are known, or if other studies arise and they qualify for them, although they’re generally for folks at this point with ASCVD, they know that they, they will be, entered into those trials if possible. So, we keep them aware.
And I think the cascade screening is very important.
I just saw a gentleman, Gary, who is 42 years old, and he was referred to me by, actually his children were referred over from our adult preventive cardiology clinic, because he has premature coronary disease having sustained the myocardial infarction at 40.
And so, [00:23:00] he has three children. And he has an a very high Lp(a)—his Lp(a) is in the 400 range.
And so, his children were referred to me. They had lipid panels, and their lipids were kind of borderline. You know, they had a mixed kind of phenotype with some elevated triglycerides and some elevated, LDL. And they’re on the chunkier side. And so, when we checked their Lp(a)s they were also elevated. Now, not to the extent that their father’s levels were, but still they were certainly over 100 in each one of them.
And so, we are honing in on risk factor modifications. And I think the parents have really embraced risk factor modification for their children as well because they know, they have seen [00:24:00] and lived, or particularly Gary has lived, with all of these, with premature coronary disease.
Geralyn Warfield (host): Thank you both for those clinical applications to the discussion that we’ve been having about Lp(a).
Is there anything else that you’d like to add that we’ve neglected to discuss already?
Kathy Byrne (guest): So, the only thing that I would say is, we need to keep in mind that Lp(a) has a very important role in cardiovascular risk assessment. And it needs to be in the forefront in our minds.
Keep in mind that it’s under measured. And so, if it’s under measured, we’re not going to be able to identify it. So, we need to increase our awareness and increase our colleagues’ awareness of in whom, and when to test.
Lisa Maher (guest): I agree. Kathy, you couldn’t have said it better.
I think one of the things that we can do is at least start putting this on people’s radar. Whether that’s, you know, talking to patients more about this and [00:25:00] definitely educating clinicians about the importance of, of drawing and testing for lipoprotein (a). Anything that we can do to raise awareness, will be helpful to prevent any further cardiovascular outcomes.
Geralyn Warfield (host): Thank you both so much.
I’d like to remind our audience that this episode is available for CE contact hours. And to make sure that you follow the link in the episode show notes, so that you can complete your post-test and evaluation and access your CE certificate.
Thank you again to our guests, Lisa Maher and Kathy Byrne, for sharing their expertise and their clinical pearls with us today.
We’d also like to thank Novartis Pharmaceuticals Corporation for their grant funding for this episode.
This is your host, Geralyn Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Lipid Management
Published on
September 5, 2023
Listen on:

MSN, CRNP, CCRN

DNP, ARNP, FNP-BC, FPCNA
Related Resources

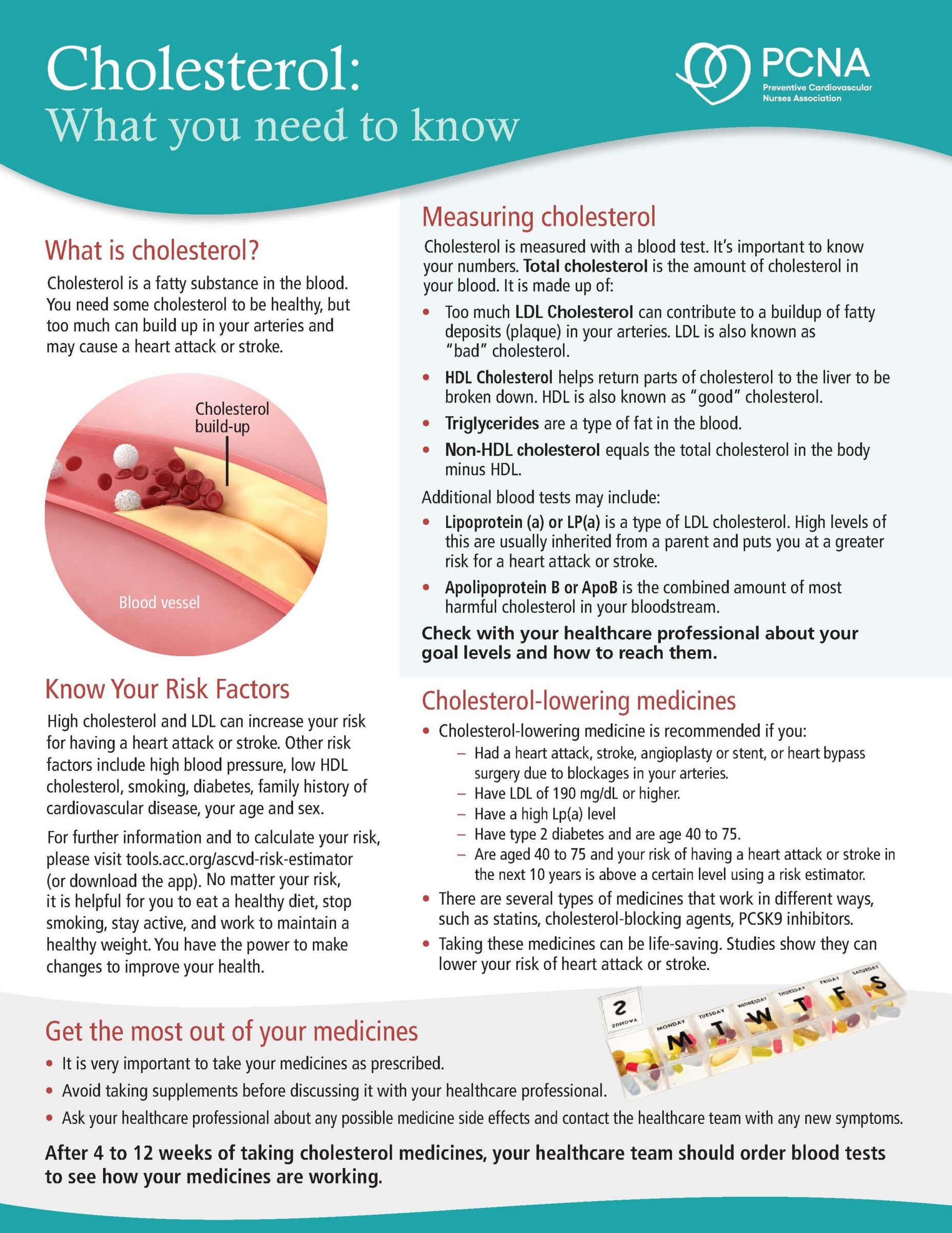
Online Interactive Guides
Cholesterol: Journey to a Healthier Lifestyle Online Interactive Patient Guide
February 12, 2025