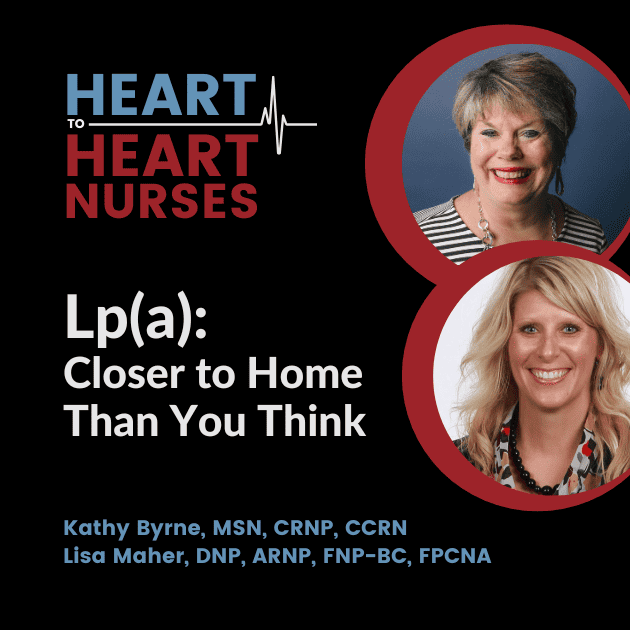
Guests Kathy Byrne, MSN, CRNP, CCRN.,and Lisa Maher, DNP, ARNP, FNP-BC, FPCNA, describe the most common genetic dyslipidemia–elevated lipoprotein (a), or Lp(a). The discussion includes testing for Lp(a)–especially for family members, and others who may be at risk. Resources for patients and HCPs are also part of the conversation.
Earn 0.25 CE contact hours from listening to the podcast episode and completing the course components.
Episode Resources
- PCNA patient education sheet – Lipoprotein(a) – What You Need to Know
- National Lipid Association
- Family Heart Foundation
- European Atherosclerosis Society Lp(a) Consensus Statement
- 2018 AHA/ACC multi-society guidelines
- American Heart Association
Welcome to Heart to Heart Nurses. Brought to you by the Preventive Cardiovascular Nurses Association. PC’s Mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Welcome to today’s episode, the first in the three episode miniseries on lipoprotein a. For more information on this topic, we encourage you to listen to our second episode and our third episode in this same series, which you’ll find in the same area where you’ve found this episode. This particular episode as the other two in this miniseries are available for CE contact hours.
Please make sure you follow the link in the episode show notes to complete the post-test and the evaluation, and to access your CE certificate. With that, I’d like to introduce today’s guest, Kathy Byrne and Lisa Meher, and they are going to be our subject matter experts on this particular [00:01:00] topic. Kathy, I’m hoping you could introduce yourself first, and then Lisa, you could certainly follow and introduce yourself before we dive into our topic.
Thanks, Lyn. I’d like to thank the P C N A for the opportunity to participate in this podcast on LP little a. I’m a nurse practitioner within the pediatric and adult cardiology departments at the Johns Hopkins Medical Institutes Institutions in Baltimore, Maryland. Um, at these two clinics I care for adults with congenital heart disease as well as all age groups who have lipid disorders.
And this of course includes screening for elevated LP little A and treatment in those who have known, um, diagnosis of elevated. LP a. And my name is Lisa Mayer, and I also wanna say a special thanks to you, Lyn and to P C N A for allowing me to participate in this podcast. I’m a nurse practitioner as well.
I work with [00:02:00] Unity Point Clinics and work at the Unity Point Health Allen Hospital Cardiovascular Center, located in Waterloo, Iowa. I am the current President-elect of P C N A and also the chapter leader of Cedar Valley, Iowa Chapter. I work in a general cardiology setting and treat patients of all ages with cardiovascular disease, along with working in a general cardiology clinic.
I manage a specialized sleep clinic in which I work with patients with underlying cardiovascular risk factors or cardiac disease who also have sleep disorder breathing, or sleep apnea. Also in addition to these two clinics I’ve previously managed, um, a prevention, uh, clinic, which was called Our Lifestyle Medicine Clinic.
We are so grateful to you both for spending time with us today. And why don’t we go ahead and get started and let’s start our discussion talking a little bit about why we should care about Lipoprotein a or LP Little a. Kathy, could you get us started? Sure. I think we should first, um, [00:03:00] discuss the prevalence of LP Little.
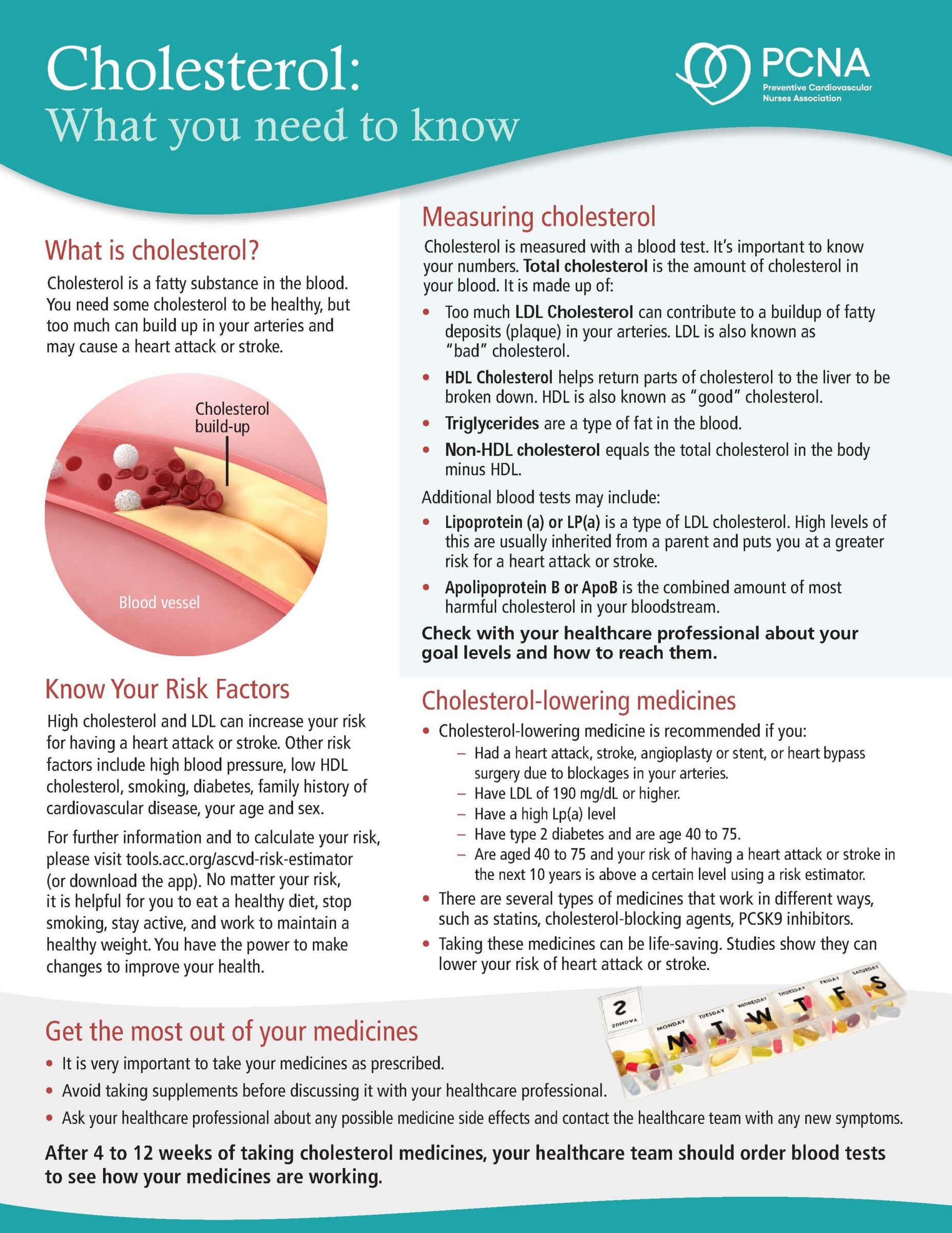
A LP Little A was identified more than 60 years ago, however, in recent years, it has come to be recognized as a prevalent risk factor for cardiovascular disease. I. Very briefly, lipoprotein little A is an L D L like particle that’s synthesized in the liver, and it’s known to be increased in individuals with cardiovascular events.
Despite optimal L D L uh, management, I. LP little A is made up of an APO lipoprotein B 100, and this is bound to Apo lo apo lipoprotein A. It derives its atherogenic from both apo A and A O B, as well as its pro-inflammatory and most likely prothrombotic characteristics from April. An estimated 1.4 billion individuals globally, or 10 to 30% of [00:04:00] the population globally, and this comes from an N H L B I report, have LP A levels that are equal to or greater than 50 milligrams per deciliter.
Or 100 uh, mil per liter. These percentages may actually be higher in individuals who already have established A S C V D in those who have calcific aortic valve disease or chronic kidney disease. It’s important to note that individuals with normal lipids can have elevated lipoprotein little A and I think we’ll emphasize this a few times throughout our talk evidence for LP Little A.
Having an independent association with cardiovascular risk has been found in epidemiologic Mendelian randomization and genome-wide studies. Thanks for sharing all that. Kathy, as Kathy has said, and I’ll touch on a little bit, um, [00:05:00] more on some of the things she touched, uh, about, but lipoprotein a is so important, but as a clinician in clinical practice, it’s something I found that still a lot of people are not familiar with.
I. And as Kathy said, it was identified more than 60 years ago, first discovered in 1963, and again as an L D L, like particle with an additional protein. APO lipoprotein, a coiled around it. It is the most common genetic dyslipidemia. And nearly one in five individuals are affected in the United States. Um, based on the lipoprotein a levels of greater than 50 milligrams per deciliter, or greater than 120 al per liter.
I. It’s also linked to several cardiovascular diseases to include MI or myocardial infarction, stroke and aortic stenosis. So when we talk about lipoprotein a, one of the things we wanna talk about or address is also who is [00:06:00] appropriate. To manage or to draw those levels in, um, these patients. Um, we want to have, um, we want to be aggressive with these patients and we wanna look at preventative treatment strategies for those patients with heterozygous, familial hypercholesterolemia, also known as fh, premature, A S C V D.
A family history of premature A S C V D, progressive A S C V D, despite optimal medical therapy. And I should also clarify, when I talk about A S C V A A S C V D, I’m, um, referring to those patients with atherosclerotic cardiovascular disease, those patients with. Recent acute coronary syndromes and those who have a family history of elevated lipoprotein a.
I’d just like to add a couple comments to what, uh, Lisa has said. And first and foremost, in children, we can check their levels [00:07:00] when they are young. In fact, we know that they, uh, reach adult LP a levels by the age of five. As well, we might want to test, uh, individuals who have been found to have increased atherosclerosis.
On CT angiography and those who have had positive coronary calcium scores who do not have conventional risk factors such as longstanding diabetes or um, smoking histories. Well, you have definitely opened our eyes. Or our ears, since we’re on an audio podcast, to the prevalence of this particular disease and how it may be affecting many of our patients that we may not even have been considering previously.
And I’m hoping we could talk just a little bit more about what type of patients that we should be, you know, thinking about for those elevated levels. And maybe, Lisa, you could get us started in this part of our conversation. Sure, thanks. So when we are considering [00:08:00] who to look at for elevated levels of, uh, lipoprotein a, um, we want to purchase or we want to proceed with proactive screening of those patients that we talked about as above, so especially those with MI or stroke.
Those with that premature family history, we want to pay, uh, particular attention to those patients too, who we have optimized their, um, lipid lowering agents and they still have high L D L. They also frequently have high levels of lipoprotein a many researchers and clinicians. Argue that individuals should have lipoprotein a measured at least once in their lifetime.
Given that those levels are largely stable throughout life. And as Kathy said, once a child reaches over the age of five, most recent, uh, version of the US lipid guidelines includes a new recommendation for lipoprotein, a measurement on select individuals as a risk enhancer. And this [00:09:00] should further raise awareness of lipoprotein a.
So when I talk about patients in clinic, once I find an elevated lipoprotein a level, I always wanna address the importance of cascade screening or testing their family members. There is a general agreement that Cascade L p a screening of children. Is reasonable when a parent with elevated lipoprotein A is identified.
Also, those, um, are appropriate when there is a family member or family history of premature cardiovascular disease. Also, when a child, um, when a case of, uh, an elevated lipoprotein a is found in a child, we wanna reverse cascade screening of the parents, uh, which would be recommended. I would also like to add that, um, in our clinic, which is a referral based clinic only, um, we do do LP little a testing on all patients who present.
And this is just because we really feel [00:10:00] it’s been a decision over the years that we want to provide comprehensive lipid care. And so all individuals will have one measurement of LP little a. So now that we’ve talked about who should be tested, I think we need to talk about what testing entails. Now again, you know, it’s currently debated as to whether there should be routine screening for lipoprotein little a or in those, um, who have specific conditions.
But when we decide or decision is made, LP little A is measured via a routine non-fasting blood test. Again, we’ll emphasize the fact that because LP little a’s levels generally remain co. Fairly constant or consistent throughout the lifestyle, uh, throughout the life cycle. One needs only to measure it once, except for the fact that we do find in post-menopausal [00:11:00] women that their lipoprotein little A levels tend to go up, and so we may recheck them again.
Um, by measuring these levels, we can certainly identify these high risk patients, and it’s been recommended by the European Atherosclerosis Society that they be tested at least once during a lifetime. Their, um, their, um, recommendations are a little more stringent than the, um, a c C and a h a guidelines certainly.
Um, In the 2018 A C C A H A Multi society, um, guidelines. We talked about LP little a being a risk enhancer, and it’s a risk enhancer for primary prevention in those without prior cardiovascular disease, but it’s uncertain whether we should start a statin and so, If they have a, an LP little, a level that is greater than 125 al per [00:12:00] liter, that would favor statin, um, initiation.
And that’s a Class one recommendation. Uh, there’s more limited guidance as to when it should be measured, um, according to the A, c C and a h a, it’s a relative, uh, indication. If there’s a family history as we’ve talked about, or premature A S C V D. Or there’s a personal history of A S C V D that’s not been explained by the major risk factors, whereas the Europeans really like to measure it in anyone who’s had premature cardiovascular disease, family history of cardiovascular disease, or elevated LP little, a FH or familial hypercholesterolemia.
If they have recurrent cardiovascular disease, despite optimal lipid lowering treatment, or if there’s greater than a 5%, uh, 10 year risk of fatal myocardial infarction. All of these things have actually [00:13:00] been mentioned by Lisa previously. So when we are looking at measuring Lipoprotein li delay, it’s worth mentioning that this is not included in the standard lipid panel, but is a specific discreet test that must be, um, ordered.
So, Now when we measure this, when we measure the LP little A, um, suffice it to say that it is a lipoprotein little, a is a very highly heterogeneous structure, meaning that, um, there are many different iso. Isoform sizes within the population. And we also notice that there are differences among, uh, different ethnic groups.
It becomes problematic as to what the cut points should be for certain ethnic groups and whether, um, LP little a, uh, should be measured in, uh, mass units such as milligrams per deciliter or in particle concentrations. Uh, in, uh, [00:14:00] nanomoles per liter, um, oftentimes in the past, okay. All we had available to us were mass measurements or milligrams per deciliter.
So I have been finding that in more recent years if we’ve had patients who have had these measurements in milligrams per deciliter, we often repeat them and we’ll find, um, some differences. And so that is very important. It is also not recommended to convert LP little A from milligrams per deciliter to nanomoles per liter.
You will find that there are some conversion factors that are um, listed. However, we do not recommend this because it’s really like comparing apples to oranges. So we don’t do that. Um, so suffice it to say there’s a current lack of standardization of LP little a assays. And the cut points, again, are lacking for different risk groups, ethnic [00:15:00] populations, and comorbidities.
We’ve been speaking with Kathy Byrne and Lisa Mayer about LP Little A and we’re gonna take a quick break and we’ll be right back. We have been discussing LP little a prevalence and testing and there is definitely a lot to learn about LP Little a. What kinds of resources would the two of you, uh, offer to our audience as being available to help those patients and their families and caregivers to become more knowledgeable about this particular disease that is indeed so prevalent?
I’ll jump in there right away and, and, uh, certainly put a plug in there. For P C N A, we have an informational tear sheet for patients that’s very informative and it’s used for generalized education and to promo to promote a conversation on testing so it. It is something that we can hand to our patients or send to them, and it is, it actually facilitates a conversation, allows them to, [00:16:00] allowing them to formulate questions as well.
I think that’s great. Kathy? Um, I too use a lot of P C N A materials with my patients because it is so patient centered and patient friendly. I think that’s important because sometimes we do forget the patient aspect in all of this when we’re looking. At educating clinicians, um, I usually look to, um, two different sources.
One is the National Lipid Association or the N L A and the other is the American Heart Association, or the a h a. I was actually fortunate enough, fortunate enough to be part of a global think tank on lipoprotein a with scientists and clinicians worldwide, and we. Talked a lot about the, um, uh, points that Kathy made in the last discussion where we are lacking, um, clinical assays.
We’re lacking those cut points, um, for different risk groups and those ethnic populations. So that was a great opportunity and, um, look forward, um, [00:17:00] to more information to come out on this in the future. Lisa, if I might add another resource that I actually. Um, used, particularly with patients is the Family Heart Foundation, which was formally the FH or, uh, familial Hyperlipidemia Foundation.
It provides a great deal of information for both clinicians and patients, and you can find information on research studies that are ongoing. Those are incredible resources for our audience, and I’m hoping that, uh, we haven’t let a, I’m gonna start that over again. Sorry. Those are all incredible resources for our audience, and I’m hoping that we’ve covered everything, but perhaps there’s something that we’ve missed that you would like to add since we have just a bit of time here at the end of our conversation.
Lisa, did you have anything that we inadvertently missed? Yeah, I just wanna add a couple more things that I think are important to touch on. One would be if the clinician decides to measure. Uh, LP little a in a clinical practice and you see [00:18:00] a value of greater than 100, greater than or equal to 180 milligrams per deciliter, or 430 m per liter.
That may indicate the need for aggressive L D L uh, lowering, um, and attention to addressing other non lipid modifiable risk factors. And then the other thing I wanna say is the l P A related risk. Like that of other risk factors is of greatest clinical significance to those with additional A S C V D risk factors.
So basically what I’m telling people is, Hey, we wanna pay attention to it. It’s important to measure. And I would also like to add as a final point, that we can’t forget, um, lifestyle modification, although that does not directly impact the LP little a it certainly does. Um, Help to modify risk. As a reminder to our audience, this episode is available for CE contact hours.
You’ll want to make sure that you follow the link in the episode show notes [00:19:00] that will lead you to complete your evaluation and your posttest so that you can then access your CE certificate. I would like to give a hardy thank you to our guests Kathy Byrne and Lisa Mayer for sharing their expertise and those clinical pearls with all of us that we can take and apply right away.
We’d also like to thank Novartis Pharmaceuticals Corporation for their grant funding for this particular podcast episode, and the other two related podcast episodes that we invite you to listen to as well. This is your host, Gerald Warfield, and we will see you next time.
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more.
Topics
- Lipid Management
Published on
September 5, 2023
Listen on:

MSN, CRNP, CCRN

DNP, ARNP, FNP-BC, FPCNA
Related Resources

Online Interactive Guides
Cholesterol: Journey to a Healthier Lifestyle Online Interactive Patient Guide
February 12, 2025