Heart and kidney function are intricately connected, with variations in one impacting the other. Guest Rajesh Mohandas, MD, MPH discusses chronic kidney disease and its impacts on CVD, chronic kidney disease treatments with cardioprotective effects, and considerations for kidney function when treating cardiovascular diseases such as heart failure.
Welcome to Heart to Heart Nurses, brought to you by the Preventive Cardiovascular Nurses Association. PCNA’s mission is to promote nurses as leaders in cardiovascular disease prevention and management.
Geralyn Warfield (host): Today we’re in conversation with Dr. Raj Mohandas, and we’re going to be learning a little bit more about chronic kidney disease and the function of the kidneys and how that relates to cardiovascular health. And Dr. Raj, I’m going to take a moment and let you introduce yourself to our audience, and then we’ll dive right in.
Raj Mohandas (guest): I’m Dr. Rajesh Mohandas. I’m a nephrologist and Chief of the section of Nephrology at Louisiana State University Health Science Center in New Orleans. My own clinical focus is on hypertension and chronic kidney disease. And I have a research laboratory that investigates the molecular mechanisms that mediate increased vascular stiffness in kidney disease and how increased vascular stiffness itself leads to atherosclerosis.
So, thank you so much for having me. I’m, it’s a [00:01:00] pleasure and I’m looking forward to this conversation.
Geralyn Warfield (host): Oh, we definitely are as well. So, let’s get started talking a little bit about how heart and kidney function are connected.
Raj Mohandas (guest): So, the heart and kidney function are very intricately interconnected. The heart pumps oxygenated blood to all organs in the body. The kidneys are important to maintain optimal blood volume, so if kidney function is suboptimal, then there’s salt and water retention. This will lead to increased blood volume and hypertension.
On the flip side, if the heart function is impaired, then blood supply to the kidneys decrease, or the pressure in the renal veins can be elevated, both of which can cause kidney dysfunction. So, we need both the heart and kidney to work together to maintain homeostasis.
Geralyn Warfield (host): So, one of the things that I think our audience would like to know a little bit more about is why patients with kidney disease have a higher risk of cardiovascular disease.
Raj Mohandas (guest): That’s a really interesting question. We know that elderly patients with kidney disease are more likely to die from heart disease than they [00:02:00] are to progress to end stage kidney disease requiring dialysis.
Both decreasing renal function, as well as presence of protein in the urine, increase the risk of heart disease. We still do not understand completely why kidney disease causes cardiovascular disease. This is an area of focus of research in our laboratory. Well, kidney dysfunction is associated with inflammation and oxidative stress, which can cause endothelial dysfunction and permit atherosclerosis. Further, in kidney disease, serum levels of phosphate, as well as that of the phosphaturic hormones, FGF 23 and parathyroid, are increased. This can lead to vascular calcification, increased vascular stiffness, and myocardial dysfunction.
In addition, when you have advanced kidney disease, you have metabolic complications such as metabolic acidosis and accumulation of uremic toxins, which can accelerate atherosclerosis. So, the kidneys can contribute to cardiovascular disease in a multitude of ways, and we are still unclear about the major mechanism driving these [00:03:00] effects.
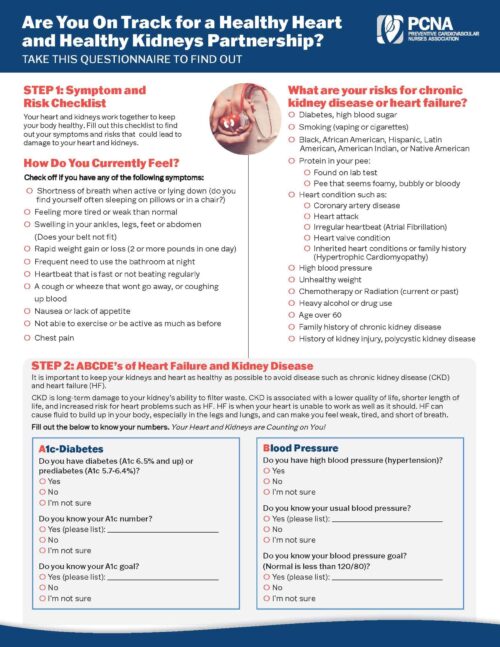
Geralyn Warfield (host): So, as our listeners who are working with patients with kidney disease are thinking about all these interrelationships, how should we go about helping those patients prevent cardiovascular disease?
Raj Mohandas (guest): A lot of intervention that we have to prevent heart disease in patients with kidney disease—and without kidney disease—are, are effective in those with kidney disease as well. So, eating healthy, regular exercise, controlling blood pressure to 130/80 mm or less, using statins to prevent hyperlipidemia, are all effective in decreasing the risk of cardiovascular disease in this population.
In addition, these are really exciting times because we have new drugs now, which could perhaps cut the risk of cardiovascular disease in patients with kidney disease, as well as be effective in treating chronic kidney disease.
Geralyn Warfield (host): So, these new drugs that you’ve described to prevent cardiovascular disease in patients with kidney disease, could you talk a little bit further about those?
Raj Mohandas (guest): Absolutely. So, we have not had [00:04:00] a new drug to treat kidney disease in over 20 years. Since the addition of ACE inhibitors in the eighties, there’s not been a new drug that’s been approved to treat chronic kidney disease.
So, there’s a lot of excitement around this new group of medications called SGLT2 inhibitors. These drugs inhibit the sodium glucose cotransporter in the proximal tubal, which is normally responsible for reabsorbing 90% of the filtered glucose. So, inhibiting this transporter will cause increased loss of glucose in the urine and thus lower blood sugars.
So, they were approved to treat diabetes. Although they were introduced to treat elevated blood sugars, they only have modest effects on lowering blood sugars. These drugs are also lower blood pressure, promote weight loss, and have other effects on metabolism and cellular signaling pathways that could be beneficial to cardiovascular health.
So, they appear to have protective effects on kidney function as well as heart function. Overall, they decrease proteinuria and slow down worsening of kidney disease. They also decrease [00:05:00] cardiovascular disease and heart failure hospitalization, both in patients with reduced as well as preserved ejection fraction, and these drugs seem to work in patients with kidney disease as well as without kidney disease.
So, these drugs are probably better called renal or cardiovascular drug rather than an anti-diabetic medication. And I, I suspect the structure will change how we practice medicine now and for years to come.
Geralyn Warfield (host): Well, there’s a lot of new information that our audience is learning today about chronic kidney disease and cardiovascular disease. We’re going to take a quick break and we’ll be right back.
Geralyn Warfield (host): We’re back with Dr. Raj Mohandas talking about chronic kidney disease and cardiovascular disease, and we’ve just learned about the new classes of medication that are available to actually have cardioprotective effects while you’re treating kidney disease.
And I’m sure our audience is curious how safe these medications are. Could you discuss that a bit, please?
Raj Mohandas (guest): Overall, these medications are remarkably safe. Because of our experience with Rosiglitazone [00:06:00] in the past, the FDA in 2008 issued guidance recommending that all anti-diabetic medications be monitored for cardiovascular safety.
So, Rosiglitazone was effective in lowering blood sugars, but those beneficial effects came at the cost of increased cardiovascular death. So, later it had to be withdrawn from the market in most parts of the world.
Overall, SGLT2 inhibitors are remarkably safe. So, the most common side effects include an increased risk of fungal infections of the genitalia and ketoacidosis. So, it’s recommended that SGLT2 inhibitors be held when you’re sick. Since SGLT2 inhibitors promote glycosuria, or loss of glucose in the urine, even with ketoacidosis, blood sugars can often be normal—the so-called euglycemic ketoacidosis. So, when patients have symptoms that could be suggestive of ketoacidosis, it’s important that we check for ketones.
Some studies have suggested that there’s an increased risk of fractures and amputations. in. How it’s [00:07:00] reassuring that perhaps these more serious side effects have not been consistently observed across all other studies, or even within the same medication in other studies. So overall, they’re really safe.
Geralyn Warfield (host): So, when should our practitioners that are listening to this podcast start worrying about kidney function?
Raj Mohandas (guest): Well, let me start by telling you when not to worry about kidney function. We know that acute and chronic kidney disease are associated with excess cardiovascular mortality. However, small trends and increases in creatinine, or a decrease in glomerular filtration rate, might just signify hemodynamic changes that could be beneficial in the long run.
For example, we know in diabetic kidney disease, one of the main culprits that drives kidney disease is hyperfiltration. So, the afferent arterial [that] brings blood to the glomerulus is dilated, which leads to increased pressure within the glomerulus. This leads to increased filtration, so at first, kidney function appears increased. However, in the long run, hyperfiltration leads to [00:08:00] loss of nephrons and kidney failure.
And ACE inhibitors or ARBs work by dilating the efferent arterial and decreasing pressure within the glomerulus. In the short term, this could result in an increase in creatine and decreased GFR. However, in the long term, it protects kidney function.
In fact, patients whose creatinine increases with initiation of ACE or ARB therapy are more likely to benefit from therapy with ACE or ARB. Similarly, initiation of SGLT2 inhibitors decreased sodium and glucose reabsorption in the proximal tubule. So, the increased sodium that delivered to the distal nephron will cause constriction of the afferent arterial. So this, again, will decrease pressure within the glomerulus and over the long term, preserves renal function.
So, it’s important that practitioners be aware of how these drugs can affect renal function and not discontinue therapy when you see small increases in creatinine or declines in GFR because they have tremendous benefits over time.
Similarly, we know in patients with [00:09:00] heart failure, it’s important to obtain adequate decongestion. Studies have shown patients who attain euvolemia or dry weight, even in the face of slightly increased creatinine, do much better over time. Having said that, I think if you see persistently worsening kidney function or signs of heavy proteinuria or blood in the urine, that might be time to consult a nephrologist earlier to make sure there’s no other underlying disease that’s being overlooked.
Geralyn Warfield (host): So, just like in many aspects of cardiovascular care, working with patients with kidney disease definitely takes a team effort. And I really appreciate the fact that you have shared with us today some great information for our listeners to take and use in clinical practice. But I do have one more final question. It’s a little bit more basic than working just with chronic kidney disease patients, and that is for each and every one of us, how much water should we drink every day?
Raj Mohandas (guest): Well, that’s a very interesting question and perhaps one that’s commonly heard these days. In fact, I think it might have even been covered on MythBusters, at least on the online version. [00:10:00]
Well, there is a common saying that once you drink eight glasses of eight ounces a day of water. Well, clearly drinking less water than you need can lead to kidney dysfunction over time. However, there’s no evidence that drinking more water than you need is helpful to maintain or improve kidney health.
Patients with urinary stones might need to drink a lot more than that to maintain a urine output of two liters or more. So also, if you have polycystic kidney disease, it might be beneficial to drink more water to suppress ADH secretion. However, in the normal population whose thirst mechanisms are intact, our bodies are extremely sensitive in detecting and informing us when to drink more water.
So, I would recommend listening to your body. Definitely drink water if you’re thirsty. Or if you notice that the urine is a dark amber color.
Geralyn Warfield (host): Well, thank you so very much, Dr. Raj Mohandas for being with us today to talk about chronic kidney disease and cardiovascular disease and the connections between the kidneys and the heart.
We have a lot to think about [00:11:00] and I think it’s time for us all to go get a glass of water. And thank you so very much for being with
We invite you to visit pcna.net for clinical resources, continuing education, and much more.
I’m your host Geralyn Warfield, and we will see you next time. [00:18:00]
Thank you for listening to Heart to Heart Nurses. We invite you to visit pcna.net for clinical resources, continuing education, and much more
Topics
- Kidney Disease
Published on
January 3, 2023
Listen on:
MD MPH
Related Resources