Cardiovascular-kidney-metabolic syndrome, also known as cardio-renal metabolic syndrome, has been growing in prevalence over the past 20 years. Join Dr. Koirala in this episode as she explores this syndrome and what risk factors to look out for in clinical practice.
Episode Resources
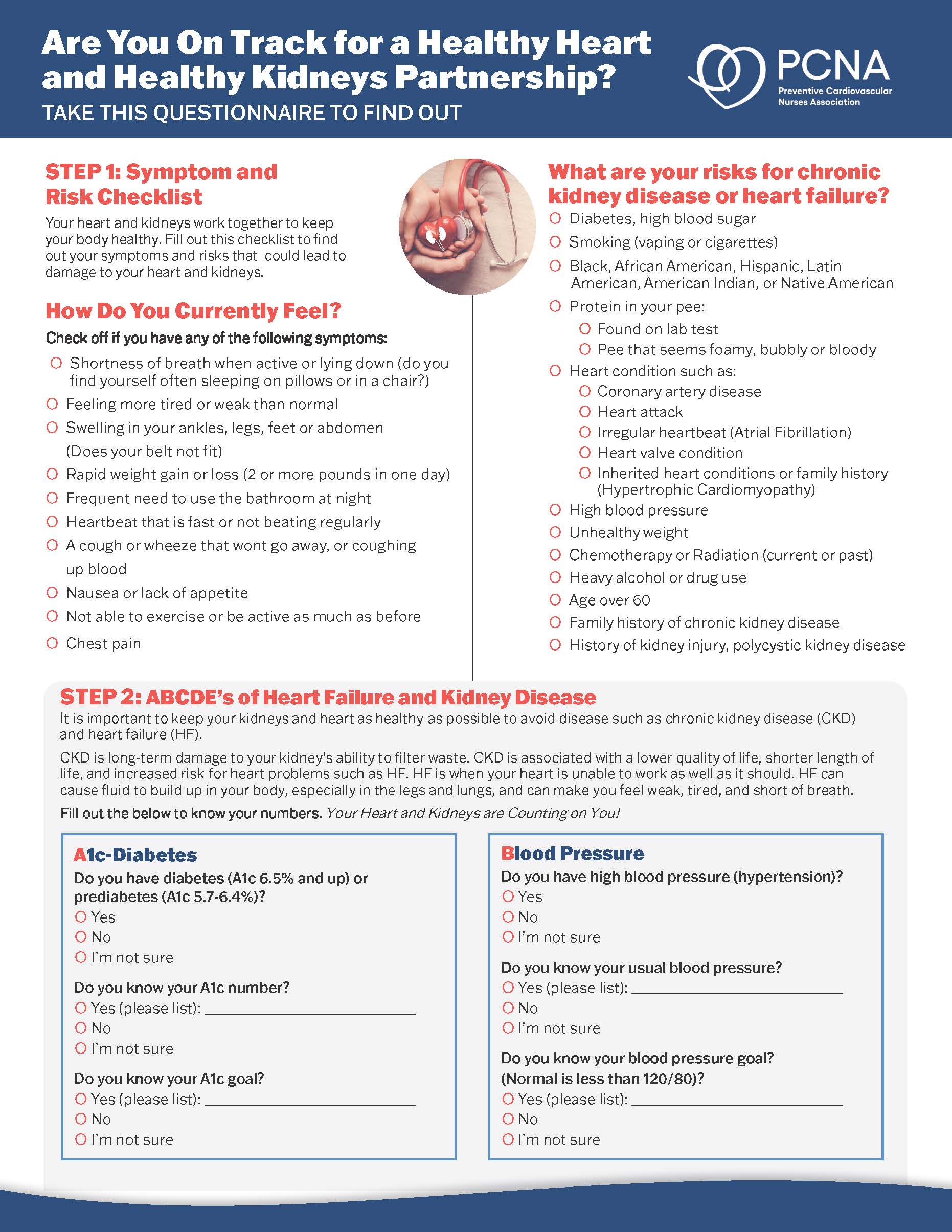
- Cardiovascular-Kidney-Metabolic Syndrome: What You Need to Know Patient Handout
- 2023 AHA Presidential Advisory and Scientific Statement
- Life’s Essential Eight
Supported by Boehringer Ingelheim-Lilly Alliance.
Geralyn (00:20)
Welcome to today’s episode, the first of a three-part series that explores CardioRenal Metabolic Syndrome, which is also known as CRM. I’d like to welcome back Dr. Binu Koirala, who has previously been a guest on this podcast. Could you please introduce yourself to our audience?
Binu Koirala (00:36)
Sure. Thank you so much for having me here today. I’m Binu Koirala. I’m an assistant professor at the Johns Hopkins School of Nursing. My clinical and research expertise include prevention and management of cardiometabolic disease and multiple chronic conditions. And I serve in multiple committees within PCNA, and I’m also a Maryland chapter president for the PCNA. And I’m so happy to be here today.
Geralyn (01:01)
Well, thank you. We’re so happy to have you on today’s episode, and I’m really looking forward to our conversation. So, let’s jump in. I mentioned earlier that this episode is about CardioRenal Metabolic Syndrome, sometimes called CRM, but to what does that refer?
Binu Koirala (01:16)
Okay, so there are different terms like cardiovascular-kidney-metabolic syndrome or cardiorenal metabolic syndrome or cardiometabolic renal disease. So, for the discussion today, I’ll be mostly talking as CKM syndrome. And also for our listeners, I’ll be mostly focusing or referring to recent presidential advisory published from the American Heart Association, and we will provide the link to the full paper at the podcast show notes.
So, starting with its definition, in a simple way, it’s overlap between metabolic conditions, such as obesity and type two diabetes, and cardiovascular disease, and chronic kidney disease, occurring at the same time in same individual. And as a clinicians and healthcare providers, we already knew that there is a bidirectional association between heart and kidney.
And then there is like pathophysiological influence of metabolic risk factors in this relationship. And we also knew about the cardiometabolic syndrome. We also knew about the kidney affecting the association between metabolic risk factors and cardiovascular disease. So, there were like all these relationships going on with these three conditions. Then we identified multiple people. Like there was prevalence of the CKM increasing with the same individual having all three conditions over time.
So, if we look at the burden like since 1999 to 2020, the CKM prevalence was doubled, like where the individual has all three conditions. So, there was more discussion about like how we can move towards more integrated holistic approach for prevention and management of these conditions because of its higher impact on morbidity and mortality.
So, then the CKM syndrome name came up as appropriate diagnosis for this condition.
So, as I said, it overlaps with three systems. It’s a multi-system disorder, and it nearly affects every major organ system in our body. However, research and other data, we have seen higher clinical impact on cardiovascular disease. So American Heart Association published this advisory highlighting the risk factors, stages, as well as the appropriate prevention and management strategies to decrease its burden.
Geralyn (03:45)
So, with all these different organ systems involved, I can imagine that trying to figure out that an individual has this syndrome might be a little complex. So, I’m hoping that you could address for our audience some of the risk factors and comorbidities that we should be looking for in clinical practice.
Binu Koirala (04:03)
Yes, and that’s a great question. So, if we look into the risk of the CKM, like in general, we estimate that one in every three people have some type of risk factor that contributes to cardiovascular disease or metabolic disorder or kidney disease. So, it’s really important to have some screening and regular follow-ups about your health conditions to identify early.
So, if I have to talk about risk factors of CKM syndrome, I would generally classify it under four categories, which are excess dysfunctional adiposity, metabolic risk factors, chronic kidney disease, and cardiovascular disease itself.
So, let’s go one by one. The first one, excess adiposity, which is also like excess fat in our body, which we can identify from the BMI and waist circumference as a clinical indicator of obesity, and it is also a major risk factor for both metabolic syndrome and cardiovascular diseases. So, we really need to look into like the excess fat. And it has been proposed that the syndrome primarily originates with the excess or dysfunctional adiposity, which secretes some pro-inflammatory and pro-oxidative products, which leads to the damage in our heart and kidney and also reduction in our insulin sensitivity.
So that’s the primary cause we have identified. So, it’s really important to look for that as a primary risk factor.
Second, metabolic risk factors such as hypertension, hyperglyceridemia, type two diabetes, and metabolic syndrome.
And I said third, chronic kidney disease, which is closely associated with metabolic syndrome and cardiovascular disease. As we all know [that] kidneys plays very important role in our body to remove waste and excess fluid. So that if the kidney function is impaired, it will build up harmful substances in our body, exacerbating the metabolic and cardiovascular conditions. So, looking for what, like looking for the cardiac, chronic kidney risk factors and then kidney disease is really important.
And as I said, cardiovascular disease itself, because range of conditions including coronary artery disease, heart failure, hypertension, all these comorbidities are often interrelated with metabolic syndrome as they share common risk factors like such as obesity, high blood pressure and diabetes.
All these risk factors are really important to look into in our patients to identify CKM. And also here, I really want to highlight the importance of looking into some of the other risk factors which can range from like individual factors such as genetics, chronic inflammatory conditions, as well as like behavioral factors like tobacco use, sleep, diet, physical activity.
And then bigger, like structural and community factors like built environment, food insecurity, those kinds of things. Because social determinants of health, like unemployment, low family income, and food insecurity are associated with advanced stages of CKM. So, it’s really important to do some regular screening and comprehensive health assessment among patients.
And if we see any of these risk factors, looking more into stages and where they are and intervening early is really important.
Geralyn (07:39)
Thank you so very much for that great overview of some of the things that we should be looking for. We are going to continue our conversation in just a moment after a quick break.
We’re back to continue our discussion about CardioRenal Metabolic Disease and the interplay between all of our organ systems and how that might look in clinical practice. Right before the break, we were talking about regular screening and how that helps us identify individuals who might be at risk for this.
And then you also alluded to the fact that there are stages. Could you maybe talk a little bit more about those stages for us?
Binu Koirala (08:09)
Sure. So, as I said, we really need to do some regular screening for CKM risk factors and it’s really important. And to enhance the prevention and management, the American Heart Association came up with the five stages, including discussing about the sum of the risk factors and what we can do about that. So, I would go one by one.
The first is stage zero where there is no CKM factors, like there is none of the risk factors such as there is no hypertension, is no obesity, is no type two diabetes, there is not any risk factors. So, the goal here for these individuals is to stay healthy at the same stage by following Life’s Essential Eight, doing wellness visit, and screening for risk factors such as blood pressure, triglyceride, high density lipoprotein, cholesterol, and blood sugar regularly, like three to five years. So, the goal here is to stay healthy.
Then comes stage one, where there is excess or dysfunctional adiposity in the people’s body. That means higher excess fat in the body. So, this includes someone who is overweight or obese and or having some impaired glucose intolerance or pre-diabetic. And the goal of care here is the more like prevention of CKM. So, following the healthy lifestyle and highly recommending the goal of weight loss because of this like higher adiposity in the body.
Then we move on to stage two where there is presence of metabolic risk factors. So those risk factors are like hypertriglyceridemia, hypertension, diabetes, and metabolic syndrome. And there might be moderate to high risk for chronic kidney disease too. So, the goal here is to treat or address these risk factor as early as possible to prevent from cardiovascular disease and kidney dysfunction.
And then we move on to stage three where there is subclinical cardiovascular disease such as atherosclerotic cardiovascular disease or heart failure, or there is higher predicted risk for cardiovascular disease or chronic kidney disease. So, to identify these individuals in this stage, clinicians need to be very careful and should consider some of the risk calculators like CAC score and kidney staging too. So there are different things they can do to identify them early. And the goal here will be to identify it in early stage and aggressively manage those risk factors to prevent from the progression.
And the final stage four is where there is clinical CVD in CKM syndrome. And this includes the diagnosis of cardiovascular disease with and without kidney failure. And individuals may already have heart attacks, stroke, chronic heart failure or other conditions such as arterial fibrillation or peripheral artery disease. You will see the clinical manifestation of these disease conditions.
So, as I said, it’s really important to do early detection of these stages and help identify where the individuals are and implement the tailored individualized approach to prevent from CKM progression to the metabolic cardiovascular and kidney complexities.
Geralyn (11:46)
So, does AHA or any other group provide an age at which this screening should start?
Binu Koirala (11:53)
So, the CKM is primarily seen among people with old age, so the prevalence of CKM increases with increasing age. But there has been studies [that have] found that people less than 65 years old also have one or two risk factors for the CKM.
So, starting early is helpful. That’s why they select, even if you are in the stage zero, take the screening as a life course perspective, you can do screening as a whole life regardless of the age. And you can do like three to five years of screening for the stage one and like generally stage zero. And for stage one, generally every two to three years. And if you are in stage two to four, you have to do screening annually to look into where you are with [those] risk factor so you can intervene early for the appropriate prevention and management.
Geralyn (12:51)
A final question for you and that is; we have talked about a lot of different aspects of this particular interplay between heart, between vasculature, between diabetes, between our kidneys. Is there one key takeaway that you would love for our audience to be able to talk about or know by the time they’re done listening or watching?
Binu Koirala (13:10)
Yes, definitely yes. So quick summary, CKM syndrome is prevalent and it’s growing in burden for both morbidity and mortality. And CKM is a multi-system, multi-faceted issue, so which requires multidisciplinary approach to prevention, screening, and management.
So [the] traditional way of just looking at one condition might not be appropriate here, so we need to work with the team. And the main one takeaway here would be early detection of CKM will allow a timely management of these risk factors such as hypertension, diabetes, dyslipidemia. So, this can prevent the overall progression of CKM syndrome.
So, as healthcare providers, especially nurses, we have a central role in identifying these risk factors early and optimizing the health of our patient population to improve the cardiovascular and other health outcomes.
Geralyn (14:10)
We are so grateful to you, Dr. Binu Koirala, for today’s insightful conversation. And I hope our audience has walked away with a lot of information that they can take with them to apply into clinical practice this afternoon or tomorrow morning, depending upon when you’re watching or listening.
This particular episode is part of a three-part mini-series on this topic. And for additional information, as Dr. Koirala said, we’ve got some resources in the show notes for you. And we’d also encourage you to participate in parts two and three of this mini-series.
We’d like to thank the Boehringer Ingelheim – Lilly Alliance for their unrestricted grant funding for this podcast miniseries. And this is your host, Geralyn Warfield, and we will see you next time.
Topics
- Kidney Disease
- Obesity Management
Published on
May 20, 2025
Listen on:

PhD, MGS, RN
Related Resources