Any diagnosis of cardiovascular disease can present challenges for our patients. However, cardiovascular-kidney-metabolic syndrome (CKM), which is also referred to as Cardio-renal metabolic syndrome (CRM), can have even more drastic effects on our patients. Hear from two cardiovascular patients, who also happen to be nurses, as they discuss navigating their specific treatment journeys.
Episode Resources
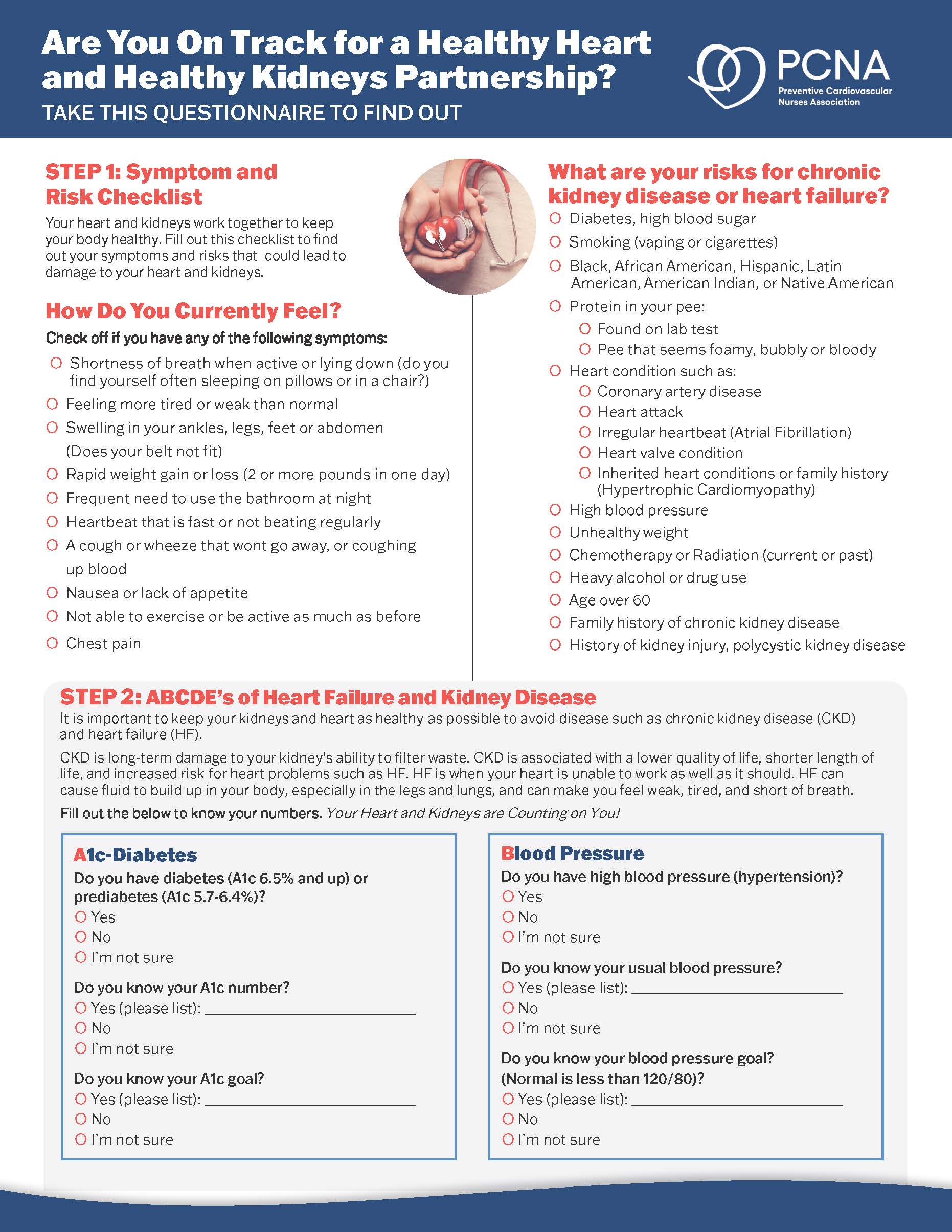
- Cardiovascular-Kidney-Metabolic Syndrome: What You Need to Know Patient Handout
- WomenHeart
- Cardiometabolic Health Congress Lifestyle Management Hub
- Cleveland Clinic Center for CardioMetabolic Health
Supported by Boehringer Ingelheim-Lilly Alliance.
Geralyn (00:20)
Welcome to today’s episode, the third of a three-part series that explores Cardio-Renal Metabolic Syndrome, or CRM. Our previous episode discussed guideline-directed treatment for patients with CRM. And today, we’re joined by Lyn Benke and Maureen Tippen to guide us on the patient experience and how nurses can support that patient’s journey. Lyn and Maureen, could you introduce yourselves?
Lyn Behnke (00:44)
Hi, I’m Lyn Behnke. I’m a WomanHeart Champion with a long and varied career in primary care, cardiovascular care, critical care, family practice, psychiatric, cardiovascular nurse practitioner, assistant professor, and a researcher with over 50 publications and invited presentations in the past 10 years.
I also serve as a rural health equity consultant for Saginaw Valley State University in Saginaw, Michigan, and adjunct faculty at the University of Michigan Flint, where I met my great colleague Maureen Tippen. My research interests include primary care of women living with heart disease and appropriate medical diagnosis of women with heart disease. My passion is obviously getting women diagnosed and treated appropriately with cardiovascular disease. Obviously, prevention is the key.
I really became even more interested with my own path with heart disease. And it’s been apparent in my practice and my presentation to nurses, students and other women with heart disease. I do have cardiometabolic syndrome characterized by obesity, diabetes type two, hypertension, coronary artery disease, stage two diastolic failure, CKD, and peripheral artery disease. Maureen?
Maureen (02:12)
My name is Maureen Tippen and I am also a registered nurse and retired associate professor of pediatric nursing at the University of Michigan, Flint. I am also a recovering patient from a coronary artery disease just with my last catheterization a mere eight days ago. And I am also interested in cardiac health for women and having that message sent out.
I have a long career in nursing, 42 years to be exact. And I have primarily worked with children in both the clinical and outpatient area, teaching in the clinical area, as well as developing international service learning courses for college students over the course of my career and 25 years of traveling to countries to service the underserved in Peru, Cambodia, Laos, and India, and the Dominican Republic. And I’m still a volunteer for the medical mission in the Dominican Republic. I couldn’t go this year because of my cardiac issues, but I plan to go back next year.
I support a group of hospice volunteers that do a camp in bereavement for children every year as well. So, I try to stay active in the things that interest me now, and one is the messaging of cardiac disease in women.
Geralyn (03:39)
Thank you so much. I know you both have quite the journey that you’d like to share. So, Lyn, I’m hoping that you could start sharing your journey with CardioRenal Metabolic Syndrome.
Lyn Behnke (03:49)
Thank you. In 2008, three months after my 50th birthday, I had a funny pain in my neck. And I tried acupuncture, I tried chiropractic, I tried all kinds of things, and I couldn’t get rid of it. I called my primary care provider on Monday and said I need an MRI of my neck. Because of course, I know everything right. And she said no, she said, “I need to remind you that you just turned 50, you’re overweight, you have high blood pressure, you have a high stress job.” And I said, thank you very much. Let’s do a stress test. And so, I flunked it spectacularly, the stress test and ended up with bypass surgery and essentially have done fairly well. I have had few more stents since then.
But following lifestyle changes, and of course, I’m an adrenaline junkie and I keep doing things that are stressful. But recently I was thinking that I had statin intolerance where you get muscle cramps from statin drugs. But come to find out it was actually peripheral artery disease. And I recently underwent surgery to bypass the blocked arteries in my legs.
And the challenge of having a procedure like this is that I had to be off my GLP-1s for 10 days. My renal status was stable. In order to balance fluids, my dry weight needed to be accurate as I gained 50 pounds during the procedure with all the fluids that they’d given me, which didn’t make my heart happy and unfortunately put me into heart failure.
So, post procedure, I had to balance meds for hypertension, take more diuretics, but not too much diuretics so that my kidneys didn’t suffer, but enough to allow me to breathe. It’s a constant balancing act. Post-surgically, I was told to eat a high protein diet, but a high protein diet generally has more fat than I’m used to. And it’s also not good for my kidneys. And I have to control carbohydrate with my kidneys. And I have to be mindful of the type and quality of protein with my heart. So, I also have to be mindful about the sodium and potassium as well as my weight and the magnesium that I have in my diet. And fortunately, my wife loves to cook. So, she’s been willing to take on the challenges with diet and that kind of thing. Having healthy foods in a rural and sometimes frontier area is a huge challenge and it’s expensive.
And so, trying to balance all these different things that I have to do for the different components of cardiometabolic disease is really a difficult thing to do.
Geralyn (06:30)
Lyn, thank you so very much for sharing your journey and about the complexities that you face with this particular disease state and all the nuances that are required to make sure that you stay healthy. Maureen, what has your experience been like?
Maureen (06:43)
I was diagnosed in June of 2022 I call that my retirement gift. And I am not your typical patient that [present] so I had a little hard time. Actually, I had a very difficult time and people believing me that something was wrong.
I have a long history of running marathons, the Boston included, and have a lifelong commitment to exercise and fitness. It’s my lifestyle. So, I had a healthy lifestyle. What I had going against me was a family history of early cardiac death. And my internist was following me pretty well. And then she retired.
It ended up being difficult for me because people would look at me and go, you’re not having any symptoms. But I was having some symptoms. And my symptoms were rather silent. And I finally went to the new physician, and I said, something is wrong with me. And the reason being is I had to stop while I was running.
Now, saying that to a physician sometimes is like, “Okay, look at you, old lady, just stop.” right? But she did believe me, and she said, and this is actually what truly happened, she said, “If you wait, you’re going to have to wait a long time, go to the emergency room and I’ll call my colleague.” And that’s how I got into the system. So, it ended up being somewhat of a crisis when it kind of didn’t have to be, if the timing would have been better for things.
So long story short, I ended up in that month with three cardiac CATHs and four stents and not getting optimal care. So, after I left the hospital, I went to a new provider and that provider followed me for a year and a half. I had a second opinion at Mayo Clinic because at that point I felt like I had been shuffled around so much I needed someone just to sit down and look at me freshly. And they did. And the Mayo Clinic, while I was there, I was diagnosed with the LDRR gene, which is a gene that, you have a 20-fold increase for early cardiovascular disease.
So, finding out that was sad, but it was also good because I felt like I wasn’t being punished for having a healthy lifestyle. After all that, I did as much as I could. And so, with that, my two daughters both have the gene, and so far one grandchild does. So, they’re all getting care, which it will be, you know, for the next generation very helpful.
So lastly, what happened is that in August of this year, I started having chest pain again. And my physician that was following me told me, Maureen, there’s no way you can have the activity level you have and have something that’s wrong with you. And didn’t do any testing. Actually, took me off a medication that ended up being problematic. So again, in October when I had my visit with the physician, I said, something’s wrong, I just know something is wrong. So, he said, I don’t think your problem is cardiac, I think it’s GI, and he ordered Prilosec® for me thinking that I had GERD.
So I said, okay, I’ll take it, but in my heart, I knew it wasn’t that. And I took it for the three weeks, and I didn’t even finish the three weeks, and I was at my daughter’s at a different geographical area here in Michigan, and I was having chest pain, and the nearest hospital was a different hospital that I had already been to. So, I went there. They took my complaints very seriously, admitted me and I had great follow-up and cardiac CATH just this last Monday and I had 90% blockage in my distal LAD that was repaired so I was heard.
Geralyn (10:58)
I would like to thank you both from the bottom of my heart for sharing your stories, your complex journeys with our audience. I think sometimes it’s very easy for us as clinicians to check off boxes, “Yes, I’ve tried this. Yes, I’ve tried this.” But I think that you, with your great perspectives as both healthcare professionals and patients, sometimes know a little bit more than those of us that are not healthcare professionals and patients, that as a patient, here’s what I need to do. I need to be an advocate for myself, and I need to make sure that I am heard. And sometimes it’s a very complex process as you both have described.
So, thank you so much for sharing your journey. The next part of our conversation, I’d like to talk a little bit more, after a quick break, I just want you to think about what it’s like for you as healthcare professionals in guiding your patients who are dealing with this disease. So, we are going to take a quick break, and we will be right back.
Thanks so much to our audience for rejoining us for our discussion about CardioRenal Metabolic Syndrome. Right before the break, we heard stories from a patient perspective about what this disease trajectory might look like and the importance of advocating for ourselves. But from a perspective of a healthcare professional, both of you are nurses. And could you share with our audience about how nurses can best support their patients through this diagnosis of CRM?
Lyn Behnke (12:17)
I think one of the key things that we as healthcare clinicians, nurses and nurse practitioners and physicians too is you really have to think about the self-care that that patient has to perform. I have a routine every morning. I can tell you exactly what I ate [on] February 6th of 2014 because I use MyFitnessPal. But you get up, you go to the bathroom, you weigh yourself, check your blood sugar, check your blood pressure, then do the yoga. And it’s a self-care journey that most of us, particularly as women, aren’t used to doing.
So, monitoring ourselves, monitoring our body, checking in as Maureen said, she knew something was wrong. Same way with me, I’ve known that there’s something wrong with my legs. And so trying to get all these pieces together.
Making sure I know what the medications are. The GLP1s have been a game changer in terms of my type 2 diabetes. Weight loss has been extremely helpful. I do live in an area where I can grow vegetables and those kinds of things and can and all those kinds of activities so that I can assure a healthy food supply.
Trying to balance medications from the cardiologist and the nephrologist and the primary care and knowing what you’re supposed to take when and why is a significant challenge.
But those are the questions and those are the things that you have to think about as a clinician to help the patient be successful in keeping these diseases stable and at bay.
Geralyn (14:02)
Maureen, what about you? What kinds of things as a healthcare professional do you think are important in this journey for patients?
Maureen (14:09)
I think probably the most important thing that I realized was bias. And so you see someone perhaps that is fit and you think well they must eat a very healthy diet and no one really asked me about my diet even though I do follow a good diet and have but how do you know that unless you ask me.
And so, getting to that next level and not just looking at the patient and saying, I don’t have to talk to them about that.
Maybe another example of that from a patient perspective is that in the last two and a half years, I’ve had five procedures where I’ve had nuclear scans or cardiac CATHs. And I want to know what my kidneys look like. And no one really puts all those pieces together that in that short period of time, there was a lot of trauma there.
So, looking at the total patient and what they’ve been through historically, not just what they’re there for you right at the moment. Which I understand, know, health care and how busy people are to just treat the problem as it is right now, but historically looking at who you are I think is very, important, either positive or negatively.
Looking at the total patient is probably the thing that I would want to emphasize, as well as what Lyn said about the medication management. Don’t assume people know what time to take medicines or how to distance them out.
Even something as simple as being on Asprin® now, you know what that means with also being on Plavix®. I mean, there’s things you have to think about in a different way. And I think those little minor things get missed sometimes. And so, I guess take a pause is my advice. Take a pause and really look at the total person.
Geralyn (16:05)
I appreciate both of your perspectives from both a patient and as a clinician and recognizing that there’s the art as well as the science of nursing. And looking at people holistically, being supportive of all the complications that they’re dealing with in their life and being supportive and asking questions and just being present, I think is a really great suggestion that you’ve provided.
I have one final question for both of you and that is what one key takeaway would you like to leave with our audience today? And Maureen, maybe I’ll start with you.
Maureen (16:37)
What would I want to give a key takeaway is basically women are different, and every woman is different. Lyn and I are different. We both have cardiovascular disease, but we are different. Our problems are different.
And so, look at each woman individually. Look at the total person.
And the other probably take away that, especially if you have a person who’s compliant and you assume, they’re OK mentally. And the mental health aspect of cardiovascular disease is so important. And if I didn’t have my colleague, Lyn, I wouldn’t have even realized what was happening to me in the mental health aspect of it’s a grief process.
And I don’t think that with any, you know, it’s a death of your health that you have to come back from and adapt to that. And so even, you know, people say, well, how you doing? I’m happy to be alive. But really, how are you doing? And that mental health aspect, it’s just always there.
And just because you’re thriving, let’s say, physically, and your happy things are going well, and you’re feeling better, there’s still that aspect of the mental health that needs to be, I would guess, probed. Because somebody would ask me, how are you doing? I’d say, I’m doing great, because I did feel better. But then there’s this underlying piece that’s always kind of nipping at you.
Geralyn (18:11)
Lyn, how about you? What would your key takeaway be for our audience?
Lyn Behnke (18:15)
Maureen, that was perfect in terms of the mental health. And the key takeaway, I think, really is for women to advocate for themselves. As you heard, Maureen put it out there. I’ve put it out there.
Advocate, educate yourself, get support if you aren’t getting what you need from your healthcare clinician, change. Get another opinion. Go to a women’s heart center. Because as Maureen said, women are different than men. Women are different from each other and have all kinds of issues that men don’t have. Men don’t have postpartum cardiomyopathy. Men don’t have a long-standing hypertension that ends up in heart failure with preserved ejection fraction.
So, there’s all kinds of subtleties and you have to advocate for yourself, check yourself, when you get these kinds of issues, get a process for your self-care. And self-care isn’t selfish.
Geralyn (19:27)
We are so grateful to our guests today, Dr. Lyn Benke and Maureen Tippen for sharing their experience with CardioRenal Metabolic Syndrome. This episode is part of a three-part series, and for additional information, we encourage our audience to visit the show notes from today’s episode and also listen to the other two episodes in this mini-series.
We’d like to thank the Boehringer-Ingelheim – Lilly Alliance for their unrestricted grant funding for this mini-series. And this is your host, Geralyn Warfield, and we will see you next time.
Topics
- Kidney Disease
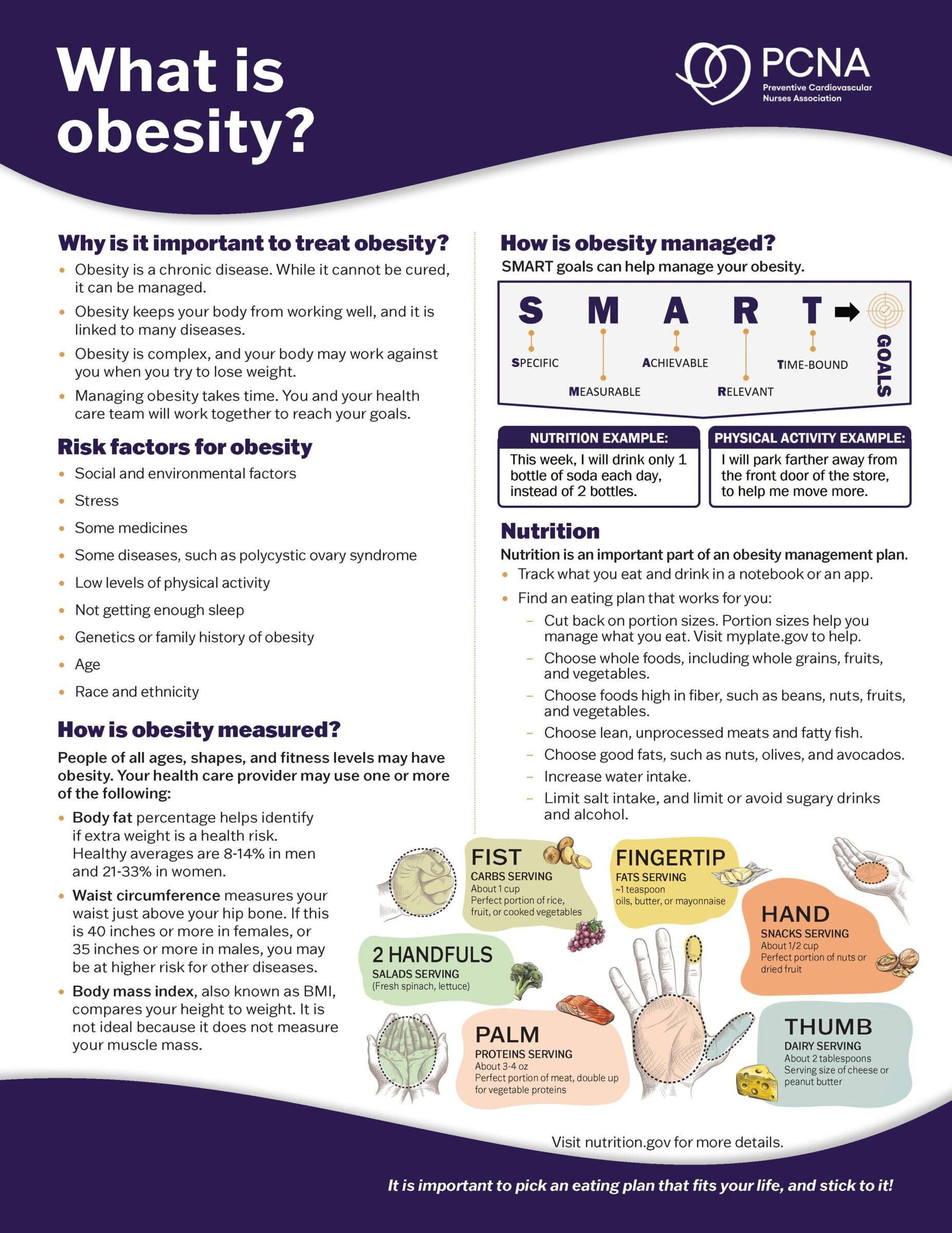
- Obesity Management
Published on
May 20, 2025
Listen on:
Related Resources