Join Chloé Villavaso MN, APRN, ACNS-C, FPCNA, AACC, as she explores Cardiovascular-Kidney-Metabolic Syndrome (CKM) also known as Cardio-renal metabolic syndrome (CRM). Listen to a recap of the 5 stages of CKM and learn how to apply guideline-directed therapy as a part of the vast healthcare team needed to treat your CKM patients.
Episode Resources
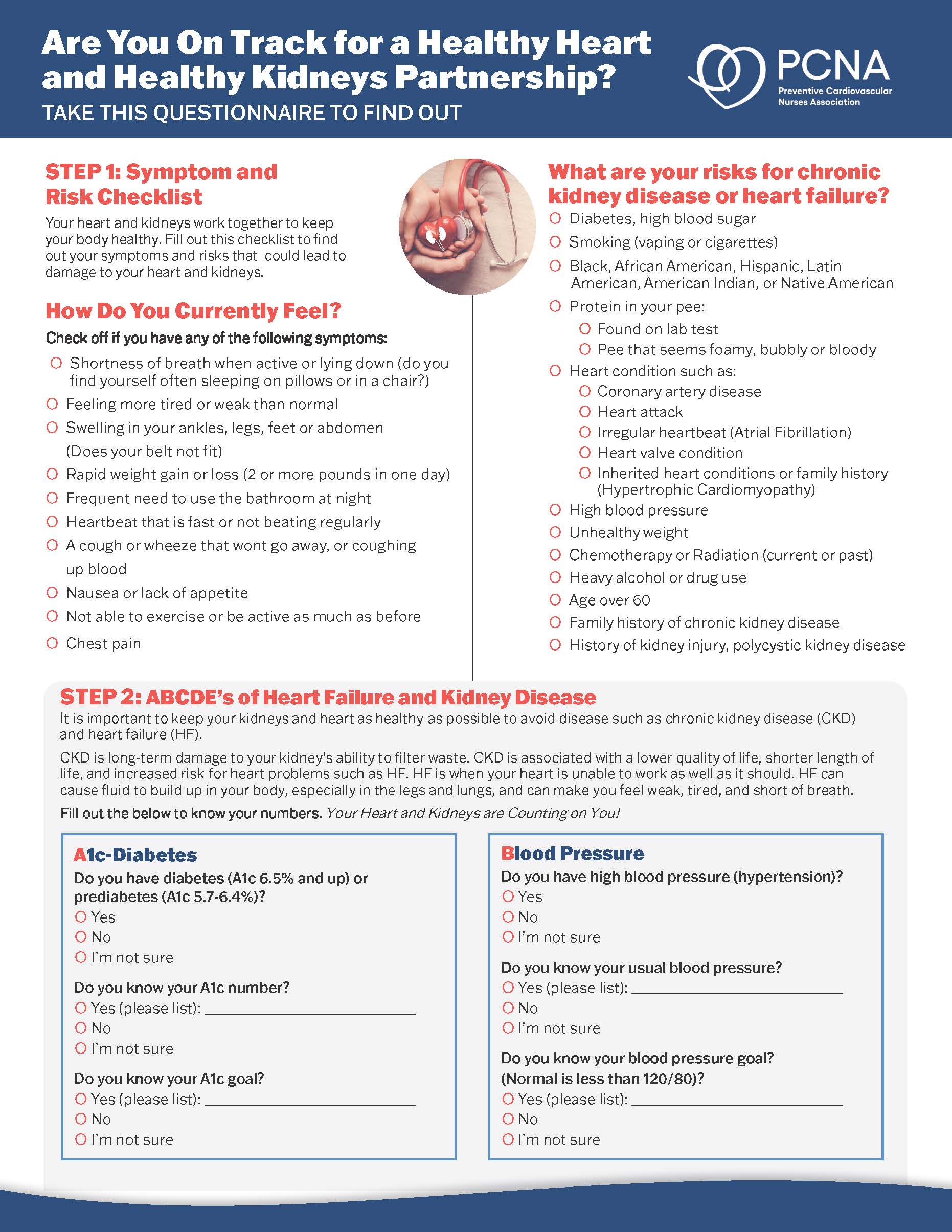
- Cardiovascular-Kidney-Metabolic Syndrome: What You Need to Know Patient Handout
- 2023 AHA Presidential Advisory and Scientific Statement
- Life’s Essential Eight
- PREVENT Tool
Supported by Boehringer Ingelheim-Lilly Alliance.
Geralyn (00:20)
I’d like to welcome our audience to today’s episode, which is the second of a three-part mini-series exploring Cardiovascular-Kidney-Metabolic Syndrome, which is also known as CKM.
Our previous episode defined CKM, which we’ve also referred to as CardioRenal Metabolic Syndrome, or CRM, and we also explored risk factors and common associated comorbidities. Today, we’re going to focus a little bit more on best practices for these patients, and I’m so excited to have in the studio today, Chloé Villavaso. She’s a PCNA board member, a chapter leader, and a clinical nurse who treats patients with CKM in the outpatient setting.
Could you please, Chloé, introduce yourself or reintroduce yourself to our audience?
Chloé Villavaso (01:02)
Thanks for the introduction, Geralyn. As you stated, I’m a clinical nurse specialist caring for CKM and other cardiovascular patients in the outpatient setting. I’m clinical faculty at Tulane University School of Medicine, and I’ve been a cardiovascular nurse for over 22 years.
Geralyn (01:21)
Well, I suspect our audience can tell that we have a great expert with us today, and I really appreciate you being back with us on our podcast. In our previous episode, Dr. Koirala addressed the four stages of CKM syndrome. Could you, Chloé, please inform our listeners a little bit more about the resources available to guide clinical practice of CKM, and specifically, how clinicians can best care for those patients within each of those four stages?
Chloé Villavaso (01:48)
Absolutely. In 2023, the AHA released a presidential advisory and a scientific statement on cardiovascular-kidney-metabolic health. These expert groups recommend specific clinical practice guidelines for each of the, actually, five steps of CKM.
So, beginning with stage zero, these individuals have no CKM risk factors. They have normal lipids, blood pressure, waist circumference, etcetera. Treatment is aimed at providing education and monitoring to maintain cardiovascular health.
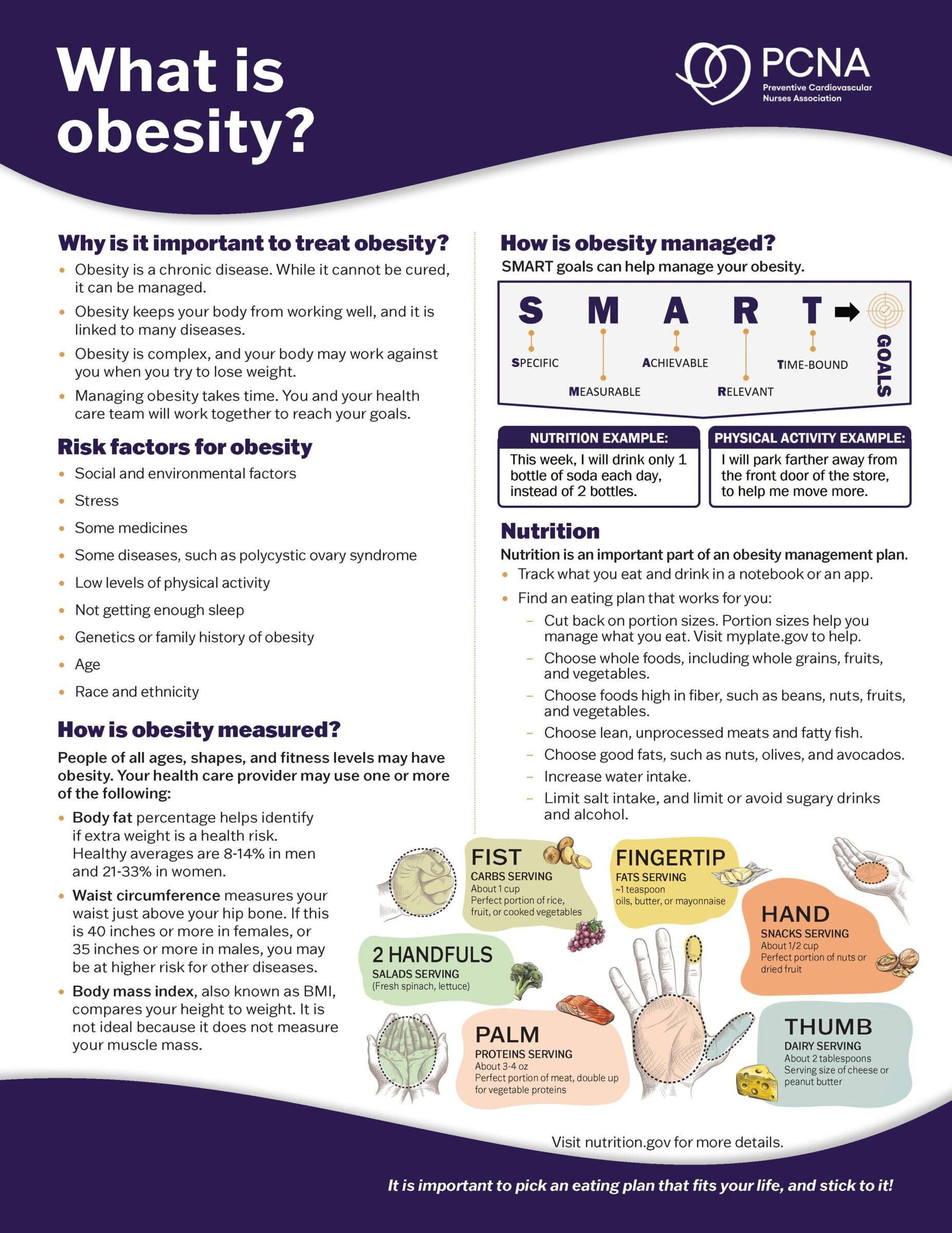
The second stage is stage one, where these individuals present with overweight, obesity, abdominal obesity, or pre-diabetes. Interventions are focused on weight reduction, including non-judgmental weight loss counseling, dietary counseling, incretin-based therapies like Semaglutide® and Tirzepatide®, and bariatric surgery.
Moving on to the third stage, stage two, this includes individuals with metabolic risk factors like hypertension, diabetes, and metabolic syndrome or chronic kidney disease. Treatment should focus on lifestyle modifications and optimizing lipid, antihypertensive, and diabetes therapies according to guidelines. Pharmacologic therapies include statins, Ezetimibe®, icosapent ethyl, ACE inhibitors, angiotensin receptor blockers, SGLT2 inhibitors, and GLP1 receptor agonist when indicated.
The next stage is stage three. This includes individuals that meet the same criteria that I listed in stage two with the addition of subclinical ASCVD or subclinical heart failure. CAC scoring and CCN geography can be considered to diagnose subclinical ASCVD. Subclinical heart failure, on the other hand, can be diagnosed by drawing an NT-ProBNP and by echocardiography. In addition to lifestyle modifications, pharmacologic treatment for individuals in stage three CKM include the treatments recommended in stage two with the addition of Aspirin®, PCSK9 inhibitors, and beta blockers when indicated.
Then moving on to the final stage of CKM is stage four. These individuals, they have clinical cardiovascular disease like heart failure, stroke, AFib, PAD, and coronary heart disease with chronic kidney disease or other CKM risk factors. Treatment includes recommendations that I previously mentioned in the previous stages, along with other therapies like finerenone and sacubitril/valsartan. It’s important to promote Life’s Essential Eight, screen for the social determinants of health, and implement interdisciplinary care for patients with CKM.
Geralyn (05:14)
We’ve been discussing CKM with Chloé Villavaso and are going to take a quick break and we will see you in just a moment.
We’re back to continue our discussion with Chloé Villavaso about Cardiovascular-Kidney-Metabolic Syndrome. Right before our break you were talking about kind of the continuum through those five stages of this particular arrangement of diseases and I know that you probably see these patients in a variety of settings.
So how would this look in the clinical setting as you are trying to deal with the complexities of transitioning them from one particular care setting to another?
Chloé Villavaso (05:50)
That’s a very important question, Geralyn. Common settings for patients with CKM include the home or the community, the hospital, and outpatient settings such as dialysis, cardiology, endocrinology, primary care, advanced heart failure, nephrology, weight loss, and lipid clinics. It’s challenging to coordinate care if all healthcare facilities are not linked through an integrated EMR.
Clinicians caring for patients with CKM should not practice in silos, rather collaborate with other specialists on the healthcare team. Since navigating through the often-fragmented healthcare system creates barriers to care, patients should be educated on CKM prevention, management treatment, and resources. Clinicians should refer patients to social workers, certified health coaches, and dieticians to address the social aspects that affect patients with CKM. For example, if a patient can’t afford a GLP-1 receptor agonist or doesn’t have transportation to multiple clinic appointments, these barriers have to be overcome to ensure adequate care for patients with CKM.
Geralyn (07:10)
I suspect for these patients with CKM also because they’re often being seen by a variety of providers or professionals that there is some inertia to treat because we always expect that somebody else is taking care of the patient in that regard. So how would you encourage us to be active in participation in that diagnosis and that treatment? And obviously, we’re all looking to have better patient outcomes as a result of that.
Chloé Villavaso (07:37)
Yes, there are several ways to overcome and avoid clinical inertia. I would say the most important, in my opinion, is to stay current on the literature. This will keep the latest research and best practices at the top of the clinician’s mind.
Second would be to collaborate with other members of the healthcare team. Because CKM is a complex syndrome that requires collaboration from various specialties, CKM patients need an organized, highly functioning, and highly skilled healthcare team.
Geralyn (08:13)
So, our final question for you today, Chloé, is what’s one key takeaway that you would like to leave with the audience?
Chloé Villavaso (08:18)
Well, I actually have a couple if that’s okay, because this is a really complex condition. So, I would say first I would like to say to the listeners that CKM is a triad made up of kidney disease, cardiovascular disease, and metabolic conditions. If a patient presents to your clinic with obesity, think CKM. If they present with diabetes, think CKM.
Don’t just treat one condition. Go into prevention mode and start addressing the full range of risk factors that could potentially become a problem.
One more thing I like to leave our listeners with is [that] CKM is unique in that the social determinants of health play a key role in the development of this condition. Individuals who are disadvantaged socially have the highest rates of CKM risk factors. Screening for and addressing the social determinants of health are key to providing care for those with CKM.
Clinicians should also consider using the PREVENT risk tool to assess a patient’s risk for developing CKM. The PREVENT tool factors in the social influence of zip code and renal function to determine cardiovascular risk.
Geralyn (09:37)
Chloé, we’re so grateful that you have been here today to share a little bit more about CKM and that diagnosis, that team effort that it’s going to take for all of us to be aware, to be conscious of, to get that diagnosis and get those treatment plans moving right along.
This episode, as I said earlier, is part of a three-part mini-series exploring Cardio-Renal Metabolic Syndrome. And for more information, we encourage you to visit the show notes from today’s episode and also listen to the other two episodes in this mini-series.
We’d like to thank the Boehringer Ingelheim – Lilly Alliance for their unrestricted grant of funding for this particular miniseries. And this is your host, Geralyn Warfield, and we will see you next time.
Topics
- Kidney Disease
- Obesity Management
Published on
May 20, 2025
Listen on:

MN, APRN, ACNS-BC, FPCNA, AACC
Related Resources