Post-acute COVID-19 and Cardiovascular Health
Thank you to Oluwabunmi Ogungbe, PhD, MPH, RN; Ruth-Alma Turkson-Ocran PhD, MPH, RN, FNP-BC; and Diana Baptiste DNP, RN, CNE, FPCNA, FAAN for this article on post-acute COVID-19 and cardiovascular health.

Promoting Awareness of Post-Acute Sequelae of COVID-19 and its Impact on Cardiovascular Health
What Cardiovascular Nurses Need to Know
In 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged globally, leading to the coronavirus disease 2019 (COVID-19) pandemic. Since the emergence of the SARS-CoV-2 virus in December 2019, we have seen how it has impacted the lives of our patients, families, and local and global communities. More recently, the COVID-19 virus has resurfaced in many mutations, including Delta, Omicron, and Beta variants.1 COVID-19 symptoms range from mild to severe respiratory symptoms accompanied by fatigue, fever, and malaise and have often been associated with cardiovascular complications such as myocardial infarction, emboli, and stroke. Within the last year, cardiovascular complications have been reported in the aggregate among patients infected with COVID-19.2
Several months into the pandemic, as the virus raged on, it became apparent that COVID-19 did not just affect the respiratory system but is, in fact, a multi-organ disease that impacts all body systems and organs.2 Another public health crisis continuing to emerge from the COVID-19 pandemic is the post-acute sequelae of COVID-19 (PASC), known colloquially as Long COVID, which presents lasting effects on those who have experienced previous COVID infection(s).
PASC is a condition identified by the persistence of COVID-19 symptoms after recovery from an acute COVID-19 infection. The World Health Organization (WHO) clinical case definition for PASC is:
“Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others and generally have an impact on everyday functioning. Symptoms may be new onset following initial recovery from an acute COVID-19 episode or persist from the initial illness. Symptoms may also fluctuate or relapse over time.”3
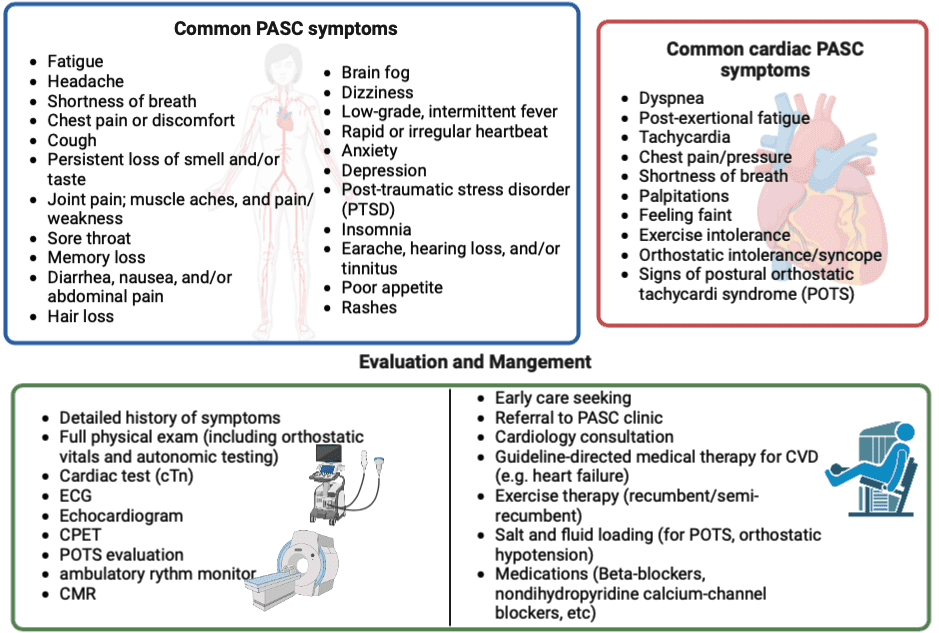
Although not much is known about the lasting effects of PASC, cardiovascular nurses need to be aware of these symptoms and understand how they impact the overall well-being and quality of life of patients. The underlying mechanisms of PASC are still largely unknown, and promoting awareness among clinicians as well as people who have experienced a COVID-19 infection is essential. Ongoing research is being done to investigate the etiology, idiopathy, and symptomology of PASC.2,4 However, based on patient cases, researchers theorize that PASC can cause residual organ damage due to the hyper-immune response to the infection, leading to many symptoms (Figure 1).
Impact of post-acute COVID-19 on Cardiovascular Health
Mechanisms underlying the impact of COVID-19 on the cardiovascular system are still emerging. Cardiovascular involvement in COVID-19 may be determined by the extent of the viral inoculum, the magnitude of the host immune response, and the presence of underlying comorbidities. Some explanations that have been postulated to date include chronic inflammation perpetuated by persistent viral reservoirs in the myocardium, i.e., direct viral assault; delayed autoimmune response to cardiac antigens;5 endothelial activation; and microvascular thrombosis.6,7
The most common cardiopulmonary PASC symptoms are cough, dyspnea, post-exertional fatigue, chest pain/pressure, and palpitations.8 Others are signs of cardiovascular autonomic dysfunction such as tachycardia, orthostatic intolerance and syncope, and signs of postural orthostatic tachycardiac syndrome (POTS).9 The prevalence of cardiac-specific PASC symptoms is substantial; a recent study among community-dwelling persons – the majority not previously hospitalized for COVID-19 – reported a 43% and 27% prevalence of cardiac PASC symptoms and new-onset diagnoses of cardiovascular disease, respectively.10
There is also evidence that the risks and burden of cardiovascular disease after COVID-19 are substantial after 1 year of follow-up – and is evident even among people who were never hospitalized.11 Cardiovascular disease diagnosis after COVID-19 infection has been reported to span several categories, including cerebrovascular disorders, dysrhythmias, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure, and thromboembolic disease.11
Some documented risk factors of cardiac PASC include increasing age, underlying cardiovascular diseases, and other cardiometabolic conditions such as obesity and/or diabetes, female sex, poor socio-economic status, etc.12 There is an equal possibility that COVID-19 may contribute substantially to worsening the prognosis of existing cardiovascular risk factors and increased risk of complications.1. This underscores the need for risk stratification, early diagnosis, and early intervention.
Approaches to Management of Post-acute COVID-19 and Cardiovascular Health
We urge nurses to perform minimally invasive cardiovascular assessments for patients who report PASC symptoms. Initial assessment should include a detailed history of cardiac symptoms, previous SARS-CoV-2 infection, and a comprehensive physical assessment. Cardiopulmonary testing, including lab measurements of cardiac troponin (preferably high-sensitivity troponin), electrocardiographic, and echocardiographic evaluation, should be prioritized. Chest imaging such as chest x-ray and cardiac magnetic resonance imaging (CMR), cardiac and pulmonary functional testing, and the evaluation of exercise capacity and oxygenation (including cardiopulmonary exercise test [CPET]) should also be considered based on abnormal findings or with persistent cardiopulmonary symptoms such as exercise intolerance, to help patients recognize their exercise capacity and limitations13
Cardiovascular nurses are in a pivotal position to advocate for early risk stratification of patients who have previously had COVID-19 to be recommended for cardiology consultation and evaluation. The American College of Cardiology recommends cardiology consultation for persons with PASC in the following cases:
- Abnormal cardiac test results (Cardiac Troponin)
- Underlying CVD or worsening symptoms
- Cardiac complications following SARS-CoV-2 infection
- Persistent cardiopulmonary symptoms that defy other explanations2
Non-pharmacological recommendations that cardiovascular nurses can provide to patients include suggesting breathing exercises, breathlessness management strategies, or pulmonary rehabilitation to persons with dyspnea. 2 Other recommendations include ample amounts of fluid, compression stockings, abdominal binders, physical therapy, and behavioral modifications for persons with orthostatic hypotension and other symptoms of POTS. 2
For persons with severe persistent chest discomfort that threatens their quality of life, nonsteroidal anti-inflammatory drugs (NSAIDs) at their lowest effective dosing may be recommended in the absence of renal dysfunction and other contraindications. Alternatively, inhaled bronchodilators may be appropriate for chest tightness attributed to bronchospasms.2
In addition, one of the most reported symptoms is limited exercise tolerance, which includes tiredness with little to no activity. Therefore, swimming, cycling, and short-lasting duration may be recommended initially for patients with cardiac PASC with a progressive transition to upright exercises as tolerated and with improved functionality.13
As with other acute and chronic conditions, encouraging continued medication adherence for patients previously prescribed cardiovascular medications is also important.
There is also an urgent need for improved access to care and increased awareness of cardiac-related PASC symptoms among nursing and other clinicians. The diagnosis of PASC can be complicated, and patients may express dissatisfaction with providers not giving them answers regarding their PASC symptoms.10 In addition, there are post-COVID clinics that design targeted therapies and treatment plans for patients experiencing Long COVID symptoms. Nurses may play a vital role in identifying and referring patients to these PASC clinics for more targeted interventions with the goals of improved quality of life and patient outcomes.
As research in this area emerges, the role of clinicians in patient education is vital. This includes recognizing credible research as well as identifying and disabusing misinformation and disinformation. Educating patients on the symptoms of cardiac PASC and encouraging them to seek care early is also important. Providers should also engage in conversations with patients on issues like vaccine hesitancy due to vaccine-associated myocarditis, explain the risk-to-benefit ratio of vaccines, and demonstrate shared decision-making to foster trust and ensure that patient needs are addressed and their questions answered.
Related Resources
- Podcast Episode with Ty Gluckman: Cardiovascular Sequelae of COVID-19 in Adults: 2022 ACC Expert Consensus Decision Pathway
- CE Course: COVID Throm-basics
- Article: Cardiac Biomarkers and COVID-19
References
- Roy B, Dhillon J, Habib N, Pugazhandhi B. Global variants of COVID-19: Current understanding. Journal of Biomedical Sciences. 2021;8(1):8-11.
- Gluckman Ty J, Bhave Nicole M, Allen Larry A, et al. 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial Involvement, Post-Acute Sequelae of SARS-CoV-2 Infection, and Return to Play. Journal of the American College of Cardiology. 2022;79(17):1717-1756.
- World Health Organization. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. World Health Organization Website: World Health Organization; 2021.
- Elseidy SA, Awad AK, Vorla M, et al. Cardiovascular complications in the Post-Acute COVID-19 syndrome (PACS). Int J Cardiol Heart Vasc. 2022;40:101012.
- Blagova O, Varionchik N, Zaidenov V, Savina P, Sarkisova N. Anti‐heart antibodies levels and their correlation with clinical symptoms and outcomes in patients with confirmed or suspected diagnosis COVID‐19. European Journal of Immunology. 2021;51(4):893-902.
- Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis—diagnosis, treatment options, and current controversies. Nature Reviews Cardiology. 2015;12(11):670-680.
- Giustino G, Pinney SP, Lala A, et al. Coronavirus and cardiovascular disease, myocardial injury, and arrhythmia: JACC focus seminar. Journal of the American College of Cardiology. 2020;76(17):2011-2023.
- Wang SY, Adejumo P, See C, Onuma OK, Miller EJ, Spatz ES. Characteristics of patients referred to a cardiovascular disease clinic for post-acute sequelae of SARS-CoV-2 infection. medRxiv. 2021.
- Bisaccia G, Ricci F, Recce V, et al. Post-acute sequelae of COVID-19 and cardiovascular autonomic dysfunction: What do we know? Journal of cardiovascular development and disease. 2021;8(11):156.
- Ogungbe O, Gilotra NA, Davidson PM, et al. Cardiac Post-acute Sequelae symptoms of SARS-CoV-2 in Community-Dwelling Adults: Cross-sectional Study. (PDF) medRxiv. 2022:2022.2007.2005.22277260.
- Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022;28(3):583-590.
- Raman B, Bluemke DA, Lüscher TF, Neubauer S. Long COVID: post-acute sequelae of COVID-19 with a cardiovascular focus. Eur Heart J. 2022;43(11):1157-1172.
- Mikkelsen ME, Abramoff MB, Elmore JG. COVID-19: Evaluation and management of adults with persistent symptoms following acute illness (“Long COVID”). In: Manaker S, Elmore JG, Finlay G, Kunins L. UpToDate2022.
