Keeping the Lantern Lit: The Role of Self-care in Preventing Burnout
An anonymous author once shared that an empty lantern provides no light. A healthcare professional (HCP) that has experienced burnout is as ineffective as an empty lantern. HCPs experience job burnout at alarming rates, which significantly compromises patient safety and quality of care (Agency for Healthcare Research and Quality, 2017).
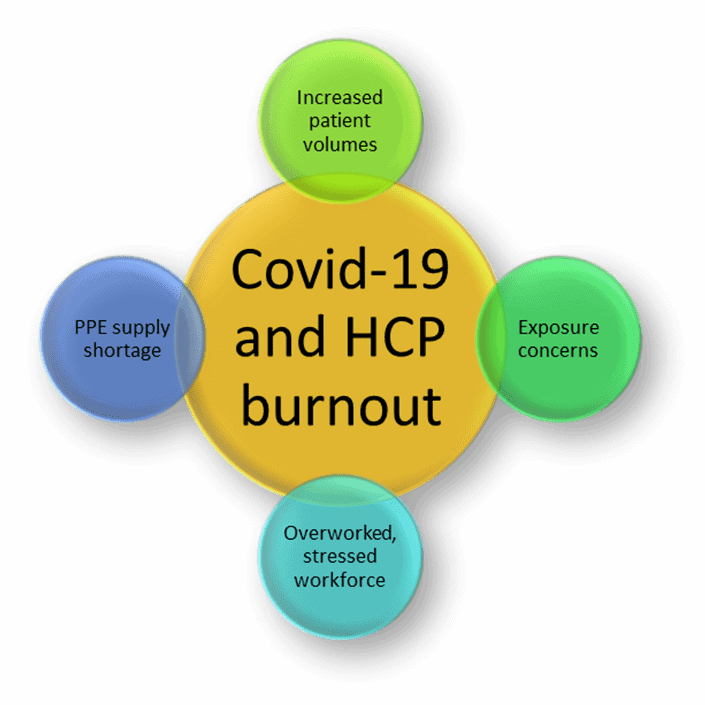
The COVID-19 pandemic has dramatically exacerbated the issue, bringing increased levels of stress and anxiety as healthcare workers are exposed to the disease, have limited personal protective resources, and are tasked with increased patient volumes requiring enhanced performance (Brusie, 2019; Green et al., 2020). Overall, 50% of nurses, physicians, and other healthcare workers experience symptoms of burnout, often characterized by the following manifestations: headaches, gastrointestinal complaints, ineffective coping, lack of energy, and fatigue (Cairns, 2020; Green et al., 2020). In 2019, about 15% of nurses surveyed indicated that they experienced burnout (Brusie, 2019). According to Berg, physicians are afflicted with at least one symptom of burnout, reporting a high incidence throughout their careers (Berg, 2020).
Job burnout is not a medical diagnosis, but rather, an experience in which the underlying symptoms may indicate a more significant issue like depression (Mayo Clinic staff, 2018). Preventing burnout is vital to maintaining the safety and well-being of patients and healthcare workers alike. Moreover, a leader who experiences symptoms of burnout will struggle to communicate effectively with their team.
A study of 20 nurses and physicians who were provided with six self-care strategies demonstrated relief of burnout and were able to develop better resilience (Shanafelt et al., 2020). Another study of more than 7,000 workers revealed that employees who experienced burnout were more likely to exhaust more sick time or terminate their employment (Cairns, 2020).
The leading causes of burnout reported by workers include:
- workload management difficulty
- feelings of unfairness in the workplace
- unclear roles
- poor communication
- impracticable time stresses
- family responsibilities
- electronic health record capacity (Cairns, 2020; Wei et al., 2020).
Managing Burnout
Managing and preventing burnout is essential to ensure the well-being of employees, patient safety, and quality of care (Agency for Healthcare Research and Quality, 2017; Cairns, 2020). Reducing stressors is one strategy to prevent burnout (Cairns, 2020; Wei et al., 2020) along with improving lifestyle habits by implementing self-care strategies such as regular exercise, practicing meditation, maintaining regular sleep and other home routines, as well as seeking support from family or friends (Cairns, 2020; Girgrah, 2020; Green et al., 2020; Kapil, 2020).
The issue of burnout cannot be solved by individual change alone. Leaders at the organizational level, as well as policymakers, have an obligation to evaluate the contributing factors of burnout on a systems-level (Richards, 2017). The local leadership at an institution may be able to help alleviate the burden of burnout by communicating with the team via huddle scenarios and implementing a program to recognize employees consistently. On a larger scale, healthcare workers rely on the administrators to lead change by determining how to improve the working environment, increase morale and minimize unnecessary demands on the healthcare team to keep a safe environment for workers and patients collectively (Green et al., 2020; Richards, 2017).
The coronavirus pandemic has increased stress levels and disrupted lives around the world. Healthcare professionals are tasked with caring for a high volume of very ill patients while risking their health to do so. Burnout is a dangerous manifestation of these stressors affecting the health care team, the individual well-being, and the safety of patients. Recognizing the signs of burnout, seeking support, and implementing work strategies such as improving communication to improve team morale are strategies that will help to combat burnout. A collective effort individually and on a systems level to keep the lantern-lit will benefit the safety and welfare of workers and patients.
Learn More
PCNA’s Online Learning Library has a free 1.0 CE course titled Caring for Ourselves So We Can Care for Others. An expert on nurse burnout, self-care, and how to cultivate resilience, Dr. Cynda Rushton provides practical tips and strategies as well as evidence to explain their long-term benefit.
The closing keynote, “Fearless Soul: The Call to Nursing and the Courage to Stay” at the 2021 Cardiovascular Nursing Symposium General Sessions will touch on this topic.
5 Self-Care Ideas for Nurses – This PCNA article from 2018 has five things you can do to manage your burnout.
References
Agency for Healthcare Research and Quality. (2017). Physician Burnout. Ahrq.Gov.
Berg, S. (2020). Physician burnout: Which medical specialties feel the most stress. American Medical Association.
Brusie, C. (2019). Study Reveals Alarming Statistics on Nurse Burnout. Nurse.org.
Cairns, R. (2020, April 27). What is burnout? How to recognize the signs and recover from work-related stress. The American Institute of Stress.
Girgrah, N. (2020, March 20). 5 Self-Care Habits for Healthcare Workers During COVID-19 | Ochsner Health. Ochsner Health System.
Green, S., Markaki, A., Baird, J., Murray, P., & Edwards, R. (2020). Addressing Healthcare Professional Burnout: A Quality Improvement Intervention. Worldviews on Evidence-Based Nursing, 17(3), 213–220.
Kapil, R. (2020). Self-Care Tips for Health Care Workers. Mental Health First Aid. mentalhealthfirstaid.org
Mayo clinic staff. (2018). Know the signs of job burnout. Mayo Clinic.
Richards, C. (2017). A Gold Bond to Restore Joy to Nursing: A Collaborative Exchange of Ideas to Address Burnout (PDF).
Shanafelt, T. D., Makowski, M. S., Wang, H., Bohman, B., Leonard, M., Harrington, R. A., Minor, L., & Trockel, M. (2020). Association of Burnout, Professional Fulfillment, and Self-care Practices of Physician Leaders With Their Independently Rated Leadership Effectiveness. JAMA Network Open, 3(6), e207961.
Wei, H., Kifner, H., Dawes, M. E., Wei, T. L., & Boyd, J. M. (2020). Self-care Strategies to Combat Burnout Among Pediatric Critical Care Nurses and Physicians. Critical Care Nurse, 40(2), 44–53.
