Homozygous Familial Hypercholesterolemia: Addressing Extreme LDL-C
Addressing extreme lipoprotein cholesterol (LDL-C) in patients with homozygous familial hypercholesterolemia (HoFH) early can help improve patient outcomes and avoid atherosclerotic cardiovascular disease, heart attack, or stroke in even the youngest patients. While this disease is rare, affecting an estimated 1 in 160,000 to 1 in 300,000 individuals, it is incumbent on everyone in the cardiovascular care team to recognize those at risk, obtain a diagnosis as early as possible, and work with patients and their families to address this genetic disease.
Hypercholesterolemia and CVD
Hypercholesterolemia is a key factor in the development of atherosclerosis. Over 38% of U.S. adults are estimated to have elevated total blood cholesterol (≥200 mg/dL), and 27.8% of adults have low-density LDL-C levels ≥130 mg/dL.[1] Guidelines-directed therapy for patients with hypercholesterolemia generally includes a combination of lifestyle and pharmacotherapies—yet for some patients, more intensive therapy may be needed, and the patient’s family members may need to be treated as well.
Familial Hypercholesterolemia
Underdiagnosed and undertreated, Familial Hypercholesterolemia (FH) is a genetic disorder characterized by high LDL-C levels and a significantly increased risk of CHD.[2],[3] It is estimated that FH impacts 1 in 250 individuals across the globe. Early diagnosis is critical and leads to treatments and management strategies to reduce the risk of heart attack, stroke, or death in patients with FH.
Individuals who have received one copy of the gene from their parents have a form called heterozygous FH (HeFH), which is characterized by LDL-C levels >190 mg/dL that respond well to drug therapy.
The most severe form, homozygous FH (also known as HoFH), affects an estimated 1 in 160,000 to 1 in 300,000 individuals who receive one copy of the gene from each of their parents.[4] This rare disease may affect children, putting them at risk for atherosclerosis, heart attack, or stroke, even as children, teens, or young adults.
Symptoms of HoFH: What to look for in clinical practice
Patients with HoFH may exhibit an array of symptoms, or none at all.
- Patients may be asymptomatic, so a thorough family history or a blood test may be the first indication of a potential issue.
- With HoFH, patients’ LDL-C levels are in the range of 400 to 1,000+ mg/dL. Even on standard medications at the highest levels, these patients do not generally respond well, and LDL-C levels remain extremely high.
- Patients may exhibit xanthelasmas and xanthomas—deposits of cholesterol found under the skin, or around the eyes.
- A corneal arcus may be present. This is a deposit of gray, white, or yellow cholesterol in a ring around the edge of the cornea.
Early diagnosis of FH and HoFH in the pediatric population is critical to improved outcomes and a healthier life. Recently-approved pharmacotherapies specifically for patients (including pediatric patients) with HoFH, along with other LDL-C lowering therapies and lifestyle modifications, reduce the risk of—or slow the progression of—CHD and can lead to a longer, healthier life.
HoFH can be diagnosed with a blood test, physical exam, and family history. To identify other family members that may be at risk, genetic testing is recommended.
Genetic Testing: A Family Affair
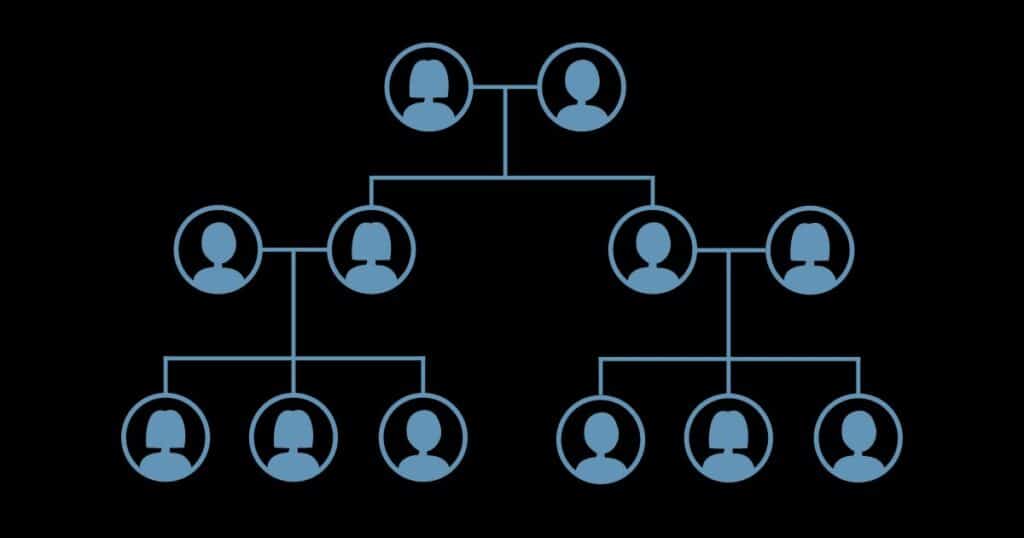
With diseases such as FH, a genetic test can be used to confirm the diagnosis and identify the genetic component of hypercholesterolemia. Particularly for the most severe form of HoFH, it is recommended that 1st-degree relatives (parents, siblings, and children) also get a genetic test. The results can identify family members who may have either HeFH or HoFH and not even know it, and lead to treatments to help them avoid heart disease, heart attack, or stroke.
Case Example
Ms. SW, a 25-year-old female, is seen in your clinical setting. She has been eating a heart-healthy diet since college and is an avid bicyclist with an average of 150 miles or more each week. Ms. SW was referred to your clinic by her ophthalmologist, who noticed a corneal arcus at her exam 2 weeks ago. She has no physical complaints.
Ms. SW completed her family history online prior to coming into the clinic. She indicates that her father was diagnosed with very high cholesterol about 10 years ago, and is on medication to control it. Her brother, now aged 42, had a heart attack about 6 months ago.
Based on her family history, you suspect FH and recommend a lipid panel. The results are an LDL-C of 279. While you are treating her with medication, you suggest a meeting with a genetic counselor. Ms. SW decides to complete a genetic test and is identified as having HoFH. Based on her diagnosis, other family members also agree to a genetic test, and two additional family members are diagnosed with HoFH, including her brother.
HOFH Resources
PCNA will have a new family education resource available in July 2023 to help parents with HoFH share with their children about the disease. You’ll be able to find it here.
- PCNA: What is Familial Hypercholesterolemia? Patient Education
- Family Heart Foundation: Homozygous FH
- American College of Cardiology: HoFH: Diagnosis and Emerging Therapies
References
[1] Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics—2022 Update: A Report from the American Heart Association. Circulation 2022;145(8):e153-e639
[2] Hopkins PN, Toth PP, Ballantyne CM, Radar DJ. National Lipid Association Expert Panel on Familial Hypercholesterolemia. Familial hypercholesterolemias: prevalence, genetics, diagnosis and screening recommendations from the National lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipidol. 2011;5(3 suppl):S9-17. doi: 10.1016/j.jacl.2011.03.452.
[3] Nordestgaard BG, Chapman MJ, Humphries SE, et al. European Atherosclerosis Society Consensus Panel. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013; 34:3478–390a. doi: 10.1093/eurheartj/eht273.
[4] Vallejo-Vaz AJ, Ray KK. Epidemiology of familial hypercholesterolaemia: Community and clinical. Atherosclerosis. 2018 Oct;277:289-297. Doi:10.1016/j.atherosclerosis.2018.06.855.
