Cultural Safety
The Pursuit of Health Equity in Cardiovascular Healthcare
Thank you to Raven Pierre, MSN, RN and Diana Baptiste, DNP, RN, CNE, FPCNA, FAAN for this article on cultural safety.
The Burden of Cardiovascular Disease
Cardiovascular disease (CVD) remains the leading cause of disability, hospitalization, and death in the United States, disproportionately affecting racial and ethnic minority groups to an alarming degree.1,2,3 Members of racial and ethnic minority groups often have poorer health outcomes and are more likely to experience CVD-related premature death. These health disparities are not solely attributed to biological factors, but in fact, are often a result of many social and environmental challenges faced by those afflicted with CVD.1,3,4
CVD and Health Disparities
The American Heart Association (AHA) expanded its focus from addressing existing CVD and its risk factors to adding strategies such as the consideration of the social determinants that would also directly promote the health of the population.1,3,4
Social determinants of health (SDoH) are organized into 6 domains, including:
- Economic stability
- Education
- Food
- Neighborhood and physical environment
- Healthcare system
- Community and social context
Traditionally, CVD treatment guidelines have utilized existing CVD prevention and management paradigms, often with limited consideration of SDoH.1,3,7
Recently, along with the six domains of SDoH, the AHA included culture and language as interrelated social factors influencing access to healthcare. Ultimately, successful multilevel interventions incorporating SDOH have direct impacts on CVD outcomes and health equity, such as reducing health disparities, improving health behaviors and access, and reducing the impact of adverse conditions.1,4
In the United States, the emphasis on diverse patient populations is rapidly progressing toward the inclusion of marginalized individuals, such as those who are aging, women, members of the LGBTQ+ community, immigrants and displaced migrants or refugees, and those who are Black and Indigenous People of Color (BIPOC).3 The emerging acknowledgment of these groups has shifted nurses’ responsibility to focus on external and environmental factors that influence cardiovascular health.
Cardiovascular nurses are also responsible for examining the barriers and social factors influencing the healthcare behaviors of these and all individuals. Emerging public health issues among these populations often result in alarming circumstances that provoke a call to action.1 Cardiovascular nurses must be vigilant in tailoring interventions to meet the unique needs of diverse populations. With the evolving healthcare needs of our population, cardiovascular nurses have the responsibility to increasingly recognize the importance of applying cultural competence to create a safe patient environment.

Pursuit of Cultural Safety in Cardiovascular Care
Cultural competence is a broad concept with various definitions that requires multiple levels of cultural awareness, knowledge, and skills about the cultural behaviors, needs, and values of others.5, 6,7 Cultural competence has been widely utilized as a tool to improve healthcare provision and reduce ethnic health disparities.8 Although the term competence implies expertise, it is without a finite endpoint: one cannot truly master cultural competence.8,9
In recent years, there has been a movement away from cultural competence strategies in healthcare toward the adoption of cultural humility as a strategy to foster a more inclusive approach to targeting health disparities.6,7,8 The term cultural humility was developed as a more desirable goal than cultural competence.6,7 Cultural humility provides a stepwise approach towards nurse-patient relationships that foster empowerment, mutual benefit, lifelong learning, partnerships, optimal care, and respect, and eliminate the power imbalances often experienced between patients and healthcare providers.6,8
Cultural competence and cultural humility remain important strategies, but it does not stop there. Both provide a path toward the goal of establishing safety within patient-provider relationships from a cultural perspective. There is a distinction between the provision of physically safe healthcare and culturally safe care.
Cultural safety represents an established sense of safety between cardiovascular patients and their providers. Unlike cultural competence strategies, cultural safety does not reinforce the notion that healthcare providers should learn about the cultural customs of different ethnic groups. Cultural safety strives to achieve better care through being aware of differences, decolonizing, considering power relationships, implementing reflective practice, and “allowing the patient to determine whether a clinical encounter is safe.”5 Without a sufficient level of cultural safety, patients could be less likely to disclose cultural and personal practices relevant to maintaining their cardiovascular health, thus contributing to health inequities 5
A Path to Achieving Cultural Safety to Promote Health Equity in Cardiovascular Care
Evidence-based literature asserts that in order to achieve cultural safety, cardiovascular nurses and health care organizations must “engage in ongoing self-reflection and self-awareness and hold themselves accountable for providing culturally safe care, as defined by the patient and their communities.”5 Diversification of the cardiovascular nurse workforce is an evidence-based approach to providing equitable care but does not guarantee the automatic utilization of culturally safe practices.5 Operationalizing an approach to achieving cultural safety by promoting heightened awareness would be advantageous to eliminate health disparities.8
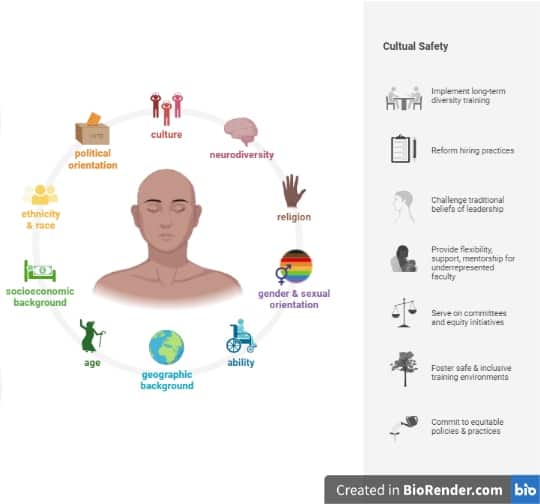
Clinical interactions across cultures can be plagued with harmful stereotypes, implicit bias, and organizational structures and characteristics that can threaten the delivery of safe and equitable healthcare.5,8 Cultural safety requires a continuous process of self-awareness that fosters the reduction of bias and prejudices and the application of cultural competence and cultural humility necessary to achieve equity in the healthcare environment (See Figure).
Figure. Pathways to achieving cultural safety in cardiovascular care
Recommendations
Addressing CVD and health disparities is everyone’s responsibility. It is imperative that we understand the factors that influence these inequities and become champions at mitigating risks in efforts to eradicate health disparities and achieve health equity.5,8 Evidence-based recommendations for achieving cultural safety during patient interactions include:
- Acknowledge that race/ethnicity alone does not account for health disparities in CVD and its risk factors.
- Consider the health behaviors, social determinants of health, and cultural beliefs influencing health outcomes.
- Exercise cultural humility as a tool to be used toward achieving cultural safety with patients
- Provide culturally tailored interventions and informed care to improve the cardiovascular health of diverse populations.
- Cultural Safety is necessary to establish and maintain trusting relationships with all patients, especially with those who are socially at-risk, marginalized, or vulnerable.
Cardiovascular nurses are trained and qualified to address health inequities across the care continuum. Given the rapidly changing landscape of patient populations, cardiovascular nurses and other healthcare professionals must be acutely aware of their role in optimizing culturally safe care for all patients.
Related Resources
- On-demand course: Cultural Safety vs Cultural Competency in the Pursuit of Health Equity
References
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. https://doi.org/10.1161/cir.0000000000000678
- Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9):e139-e596.https://doi.org/10.1161/cir.0000000000000757
- Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873-898.
- Jilani MH, Javed Z, Yahya T, et al. Social Determinants of Health and Cardiovascular Disease: Current State and Future Directions Towards Healthcare Equity. Current Atherosclerosis Reports. 2021;23(9):55. https://doi.org/10.1007/s11883-021-00949-w
- Curtis E, Jones R, Tipene-Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. International Journal for Equity in Health. 2019;18(1):174. https://doi.org/10.1186/s12939-019-1082-3
- Foronda C, Baptiste D, Ousman K, Reinholdt M. Cultural humility: A concept analysis. Journal of Transcultural Nursing. 2016;27(3):210-217. doi: 10.1177/104365961559
- Foronda CL, Prather S, Baptiste D, Luctkar-Flude M. Cultural humility toolkit. Nurse Educator. 2022;E Pub Ahead of Print. doi: 10.1097/NNE.0000000000001182
- Powell-Wiley TM, Baumer Y, Baah FO, Baez, et al. Social determinants of cardiovascular disease. Circulation Research. 2022;130(5):782-799.
